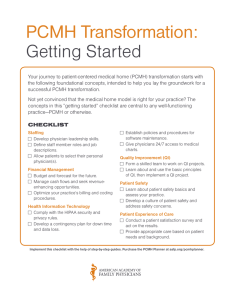
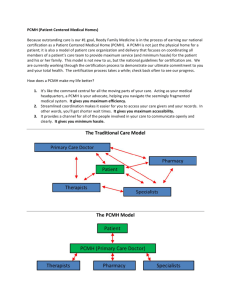
PCMH “Basics”
advertisement

Patient-Centered Medical Home Overview October 15, 2013 The Transitioning U.S. Marketplace Employers Demanding More Value for Dollars Spent on Healthcare • Global competition • Aging workforce • High healthcare cost structure • Increasing demand for productive human capital 2 Information about Healthcare Cost and Quality is Improving • HIT Proliferation via private and government investments • Consumerism-driven cost and quality transparency Employers Becoming More Adept at Pulling Levers to Get Better Value • Wellness Incentives • Value-Based Insurance Design – Prescription benefits – Medical benefits • Medicare data • Centers of Excellence • Comparative Effectiveness Research • Pay for performance Why PCMH? • The PCMH model of care is associated with: Better patient health outcomes Higher patient satisfaction Lower per-capita costs • Financial support available in SC for PCMH practices Monthly care coordination fees Bonus incentives based on performance improvement Financial rewards for seeking and achieving NCQA recognition Guidance and support through the NCQA recognition process 3 PCMH “Basics” Same-day appointments for patients who need care Promotes continuity of care and helps patients avoid unnecessary use of the emergency room, retail clinics and urgent care centers. Patients who have convenient access to their medical home are less likely to seek care from other providers Benefits: • • • • 4 Reduces unnecessary use of the ER Decreases patient use of retail clinics (fractured care) Provides continuity of care which is associated with better health outcomes Increases patient satisfaction PCMH “Basics” Clinical team meetings (AKA “Daily Huddles”) • Care teams hold regular meetings to review upcoming scheduled patient visits (“visit pre-planning”) • Typically held daily, in advance of patient visits, and include the following activities: Identifying gaps-in-care and establishing plans to address needs during visit Review of specialist reports Review of lab and imaging reports Benefits: More robust patient visits 5 PCMH “Basics” Population management & proactive outreach • The ability to identify groups of patients by condition and/or services needed • Outreaching to patients who need care (letters, phone calls) Benefits: • Prevents inactive patients from “falling through the cracks” • Improves performance on clinical measures 6 PCMH “Basics” Collaborating with patients and families to develop care plans • Providing patients with a written/electronic copy of their care plans and treatment goals • Providing education, tools and resources to help patients better manage their conditions • Tracking goals and progress with patients at each relevant visit • Assessing and addressing barriers when patients are not meeting their goals 7 PCMH “Basics” Referral and test tracking Formalized processes for tracking referrals and tests to ensure: Results and reports are received timely Abnormal results are reviewed by clinicians Results are shared with patients Benefits: - Safety! - Prevents “lost” results 8 PCMH “Basics” Continuous Quality Improvement Capturing data that can be used to track performance on important measures such as: Patient satisfaction Clinical measures (diabetic A1Cs, LDLs, annual eye & foot exams, etc.) Preventive measures (physical exams, immunizations, mammograms, etc.) Having access to useful and accurate data helps practices identify areas for improvement AND measure the success of improvement activities. Benefits: Improved performance 9 Lessons Learned Successful recognition doesn’t guarantee a successful PCMH. Identify current problems in your practice and seek to solve them through your PCMH transformation. Apply “R & D” techniques, wherever possible (Rip Off and Duplicate) Having at least one engaged physician leader within the practice is critical to success Change is practice-wide involving all staff working as a team and at the top of their license Successful transformation leads to improved physician and staff satisfaction 10 10 10 And, most importantly… PCMH isn’t just for large practice systems! Smaller practices are more nimble Not as many layers of decision-makers (fewer people to disagree!) Can define goals more quickly Communicate more easily 11 11 11