Building the Evidence for the Patient-Centered Medical Home
advertisement
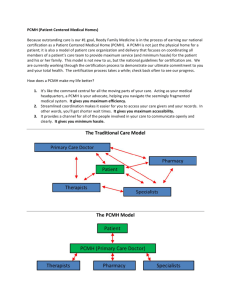
Building the Evidence for the Patient-Centered Medical Home Eric Schneider, M.D., M.Sc. Senior Scientist and Director, RAND Boston Associate Professor, BWH, HMS, HSPH 1 PCMH Assumptions • Primary care in its current form faces extinction • Changing the structure of primary care delivery will improve process, outcomes, and costs of care • Payment reform is necessary 2 PCMH Policy: A Toxic Brew • High level of desperation among purchasers • High level of advocacy by primary care professional societies • Uncertainty about model – Implementation – Cost of investment – Effectiveness 3 Research evidence could help, but… • • • • • Complex interventions Short time horizons Small sample sizes Randomization challenges Relatively small incentives 4 Need investment and savings simultaneously Comparative Public/Private Expenditures on Health - Per Capita (2004 US$ PPP) US$ Purchasing Power Parity Per Capita 7000 6000 5000 3374 4000 3000 956 682 2209 2477 2340 2177 Canada France Germany United Kingdom 703 369 2000 1000 2728 0 public United States private 5 What is that state of the evidence? • What is the medical home intervention? • Can the medical home… – change health care delivery? – reduce the growth of health care costs? – change the health of the population? • How readily can the medical home be implemented? 6 Should we rely on evidence about parts or on the integrated whole? 7 What, exactly, is the medical home intervention? • • • • • • • Payment scheme Practice management redesign Staffing change Clinician behavior modification program Patient behavior modification program Communications project Health information technology project 8 Is it a bold stroke or an incremental change? • Does the Ptolemaic pecking order remain in place? – – – – – – Hospital Specialist physician Generalist physician Ancillary professionals Staff Patient 9 Is it standardized? 10 Or a local, custom build? 11 NCQA PPC-PCMH Scoring Standard 1: Access and Communication A. Has written standards for patient access and patient communication** B. Uses data to show it meets its standards for patient access and communication** Pt 4 5 9 Standard 2: Patient Tracking and Registry Functions A. Uses data system for basic patient information (mostly non-clinical data) B. Has clinical data system with clinical data in searchable data fields C. Uses the clinical data system D. Uses paper or electronic-based charting tools to organize clinical information** E. Uses data to identify important diagnoses and conditions in practice** F. Generates lists of patients and reminds patients and clinicians of services needed (population management) Pt Standard 3: Care Management A. Adopts and implements evidence-based guidelines for three conditions ** B. Generates reminders about preventive services for clinicians C. Uses non-physician staff to manage patient care D. Conducts care management, including care plans, assessing progress, addressing barriers E. Coordinates care//follow-up for patients who receive care in inpatient and outpatient facilities Pt 2 Standard 5: Electronic Prescribing s A. Uses electronic system to write prescriptions B. Has electronic prescription writer with safety checks C. Has electronic prescription writer with cost checks Pts 3 3 Standard 6: Test Tracking Tracks tests and identifies abnormal results s A. systematically** B. Uses electronic systems to order and retrieve tests and flag duplicate tests Pts 7 Standard 7: Referral Tracking A. Tracks referrals using paper-based or electronic system** Pts 4 3 3 6 4 3 21 3 4 3 5 8 6 13 4 Standard 8: Performance Reporting and Improvement A. Measures clinical and/or service performance by physician or across the practice** B. Survey of patients’ care experience C. Reports performance across the practice or by s physician ** D. Sets goals and takes action to improve performance E. Produces reports using standardized measures F. Transmits reports with standardized measures electronically to external entities Pts 3 3 3 3 2 1 15 5 Standard 9: Advanced Electronic Communications A. Availability of Interactive Website B. Electronic Patient Identification C. Electronic Care Management Support 20 Standard 4: Patient Self-Management Support A. Assesses language preference and other communication barriers B. Actively supports patient self-management** 2 Pt Pts 1 2 1 s 2 4 6 4 **Must Pass Elements 12 Evaluated Models 1. The pediatric medical home 2. Community Care of North Carolina (CCNC) 3. National Demonstration Project (TransforMED project) 13 Can the medical home change health care delivery? • • • • • COSTS Clinical care process (measurable) Access Patient experience of care Staff work-life satisfaction 14 1. Pediatric Medical Home • Systematic review – 33 published papers describing 30 studies – 9 studies included comparison groups • Results – Most address children with special health care needs – Variety of implementations (none complete) – Generally positive associations between medical home and • • • • better health status timeliness of care family centeredness improved family functioning Homer CJ et al., Pediatrics, 2008 15 2. Community Care of North Carolina (1998-2002) • Goal of CCNC – to develop local networks of primary care providers to coordinate prevention, treatment, referral and institutional services for Medicaid beneficiaries • Chronic disease focus (asthma, DM, etc.) • Structure – 12 Networks (1 statewide and 11 local) – 246 Providers/practices – 252,190 Medicaid beneficiaries http://www.communitycarenc.com/ 16 Cost savings • Estimated Medicaid savings over 3 years for beneficiaries with asthma or diabetes in CCNC program (compared to ACCESS program after age adjustment): – Asthma: approx $3.3 million – Diabetes care approx $2.1 million • if all eligible persons in North Carolina were treated in CCNC networks (rather than ACCESS program) projected savings (on average) would have been $5.9 million in 2002 17 Utilization reduction 18 Changes in process of care were modest at best 19 CCNC Update 2007 • Savings projected at between $135 - $149 million over what would have been spent without any effort to contain costs 20 3. National Demonstration Project • 36 practices – selected from 337 motivated applicants • Randomized to facilitated vs. self-directed change – Facilitation included coaching • Two-year implementation period – Ended June 2008 Nutting et al, Annals of Family Medicine, 2009 21 National Demonstration Project: Initial Lessons Learned • Becoming a PCMH requires transformation • Technology needed for the PCMH is not ‘plugand-play’ • Transformation to the PCMH requires personal transformation of physicians • Change fatigue is a serious concern even within capable and highly motivated practices • Transformation to a PCMH is a developmental process • Transformation is a local process Nutting et al, Annals of Family Medicine, 2009 22 Readiness for the PCMH? Evidence from Massachusetts Assistance and reminders Specially-trained staff assist patient self-management Shared system to contact patients for clinical preventive services Paper reminders (% of sites) 57 53 44 Culture of quality Feedback on clinical quality Feedback on patient experience ratings New initiatives on clinical quality New initiatives on patient experience ratings Frequent meetings to discuss quality Practice has leader for clinical quality 88 66 73 47 43 58 Friedberg MF et al, Journal of General Internal Medicine, 2009 23 Prevalence of structural capabilities Access ≥1 clinician provides care in language other than English On-site language interpreters Open for regular care on weekends (% of sites) 57 32 24 Electronic health records Frequent use* 75 Specific functionalities Radiology results Lab results Specialist notes Medication list Problem list E-reminders Frequently-used, multi-functional EHR† *Computer used “usually” or “always” during patient visits. †EHR is frequently used and has all listed functionalities. 88 88 63 63 53 44 33 24 State of the Evidence: “Known unknowns” • What is the medical home intervention? – striving toward the NCQA PPC-PCMH standard • Can the medical home… – change health care delivery? • Probably true for selected settings and populations – reduce the growth of health care costs? • Unknown – change the health of the population? • Unknown • How readily can the medical home be implemented? – unknown 25 Will evidence influence policy? 26 Commonwealth Fund PCMH Evaluators’ Collaborative • Many evaluation projects across U.S. • Attempting to rigorously measure… – – – – – financing, costs, and savings degree of implementation of PCMH components changes in patient experience of care staff work-life satisfaction changes in clinical care processes • Workgroups striving to standardize measurement despite heterogeneity of demonstrations 27 Transformation in Parallel: A Chicago Perspective 28