+
advertisement

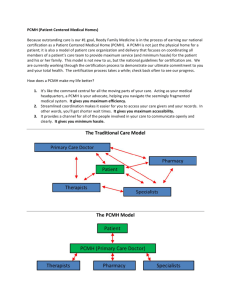
+ Will the PatientCentered Medical Home Improve Efficiency and Reduce Costs of Care? A Measurement and Research Agenda Elbert S. Huang MD MPH University of Chicago PCMH Evaluators Collaborative Efficiency Workgroup June 29, 2010 + Reference Meredith B Rosenthal, Howard B Beckman, Deb Dauser Forrest, Elbert S Huang, Bruce E Landon, S h Lewis Sarah L i Medical Care Research and Review, published p online June 2nd, 2010 PMID: 20519426 + Outline Logical L i l framework f k off costt and d efficiency ffi i workgroup What are we trying to measure? What are the common outcome measures that pilot studies? could be shared across p Describe evaluation plan for PCMH intervention in safety net clinics sponsored by Commonwealth + A Comment on Perspective Health economic evaluations must begin by establishing the perspective of the analysis Societal Payer* Health clinic) Patient Choice What care provider (integrated health system, of perspective determines y measure you Time frame for analysis Conclusion + A Comment on Perspective Diabetes Health Disparities Collaborative Experience Societal/payer / perspective Intervention highly cost-effective over time Huang et al. Health Services Research. 2007; 42 (6 Part 1): 2174-2193. Health care provider perspective (outpatient clinics) Intervention is a new cost with no source of revenue Huang et al. Jt Comm J Qual Patient Saf. 2008; 34(3): 138 146 138-146. + What Are We Trying to Measure? Costs Amount an insurer pays for care PCMH Costs Practice P i costs to implement i l the h PCMH: PCMH for f the h purpose off calculating ROI (incremental net revenues over incremental net costs of operating as a PCMH) Efficiency The extent to which resources are used to maximize health benefits at a given cost In practice we are focusing on cost and utilization metrics that help flesh out these concepts: substitution of equal quality; lower cost care (e.g., generic substitution, substitution office visits for ED ED, group visits visits, email visits) + 7 Principles of Measurement A logical connection must exist between PCMH elements and each cost/efficiency measure. Cost/efficiency measures and proxies should be evidence-based and grounded in clinical appropriateness. appropriateness Not all PCMH pilot studies are the same. “Most appropriate” measures can be selected to reflect the appropriate sequence of PCMH elements implemented. Changes ge in p patient e c care e and health e status take e time e to o accrue. Evaluations should identify intermediate outcomes that demonstrate the projects are y moving g on the path p towards improved p successfully outcomes and reduced spending. Evaluations should search for unintended positive and + 8 Logic Model Inputs: Measurable Elements of the PCMH Payment Incentives: targeting quality and cost measures (varies by pilot) Enhanced access: new modes of communication, expanded availability, language etc. Informed Care Management: disease registries, patient education, care management for high-risk populations, e-prescribing Coordination of Care: referral and test tracking, management of care transitions + 9 Payment Incentives Recent studies show modest evidence of impact, at least one study with cost savings Pay for performance (P4P), if part of the pilot, could target cost or utilization measures directly Pay for performance targeting improved care for chronic h i ill illness may save money indirectly i di tl Essentially, (1) if cost/utilization measures are in P4P and quality i does not decline i then efficiency ffi i may increase, (2) if over use measures are in P4P then efficiency may increase, or (3) if chronic care quality measures are in P4P then efficiency may improve + Enhanced Access The effect of enhanced access will differ from the effect of “primary care vs. no primary care” Access A to non-visit i i based b d care and d team visits i i may decrease primary care visits; specialty care unknown Potential reductions in emergency department utilization, hospitalization, and total costs New modes of access (after hour calls)(Lattimer 2000) Expanded primary care hours (De Maeseneer 2003, Billings 1996) Enhanced language access services (Hampers and McNulty 2002) + 11 Informed Care Management Chronic Care Model (CCM) (Pawlson 2009) May increase or decrease primary care or specialty p y care Prescription drug utilization and possibly costs might increase if PCMH successful Test utilization may also increase + 12 Informed Care Management Systematic reviews of CCM (Bodenheimer 2002; Coleman 2009) Bodenheimer review: 18/27 studies ((CHF,, asthma,, diabetes) studies showed reductions in utilization and costs with CCM Numerous more studies have found improvements in p processes of care and intermediate health outcomes (Homer 2005; Asch 2005; Chin 2007; Vargas 2007) Others have found no effect on intermediate health outcomes ((Landon 2007)) + 13 Care Coordination Geisinger medical home model with practicebased care managers and focus on care transitions for Medicare patients showed ~20% reduction in all-cause all cause readmissions (Paulus, Davis, and Steele 2008) Coleman et al. al 2006 find reductions in readmissions with independent coaches that serve patients immediately post post-discharge discharge Other non-practice based coordination efforts have been less successful Medicare Health Support demonstrations had little effect on health care spending (Peikes 2009) + 14 Logic Model Outputs: Measurable Effects that Relate to Costs and Efficiency Reasonable R bl Admissions (ambulatory-care sensitive) Readmissions ED visits (ambulatory-care sensitive) No degree d off evidence/support id / t evidence or cross-sectional only Lab tests and imaging (speculative) R f Referrals l (b (based d on cross-sectional ti l evidence id only) l ) Generic prescribing + Utilization and Cost Measures Primary care visits Specialist visits Screening and diagnostic tests Prescription P i ti Emergency g y d drugs department p visits (all ( and ambulatoryy sensitive) Hospitalizations Re-admissions (all and ambulatory-sensitive) + Utilization and Cost Measures Many stakeholders will be interested in dollar dollardenominated effects Using U i actual t l dollars d ll paid id (“allowed (“ ll d amount”) t”) may be simplest approach for evaluators but paid amounts vary Recommend using a common fee schedule as yardstick d ti k or use average rates t from f all-payers, ll allll provider data + Summary Measures Cost per case (episode) – calculated using standard episode grouper software Costs per member per month – has the advantage of simplicity but requires risk adjustment Summary measures should be calculated for entire enrolled population as well as subsets of patients (patients with diabetes, heart failure) + 18 Practice and Plan Implementation Costs We recognize that implementation and transformation costs should be counted in the full assessment of the policy Incremental outlays of resources for the pilot? Fixed and variable costs of PCMH Unclear whether evaluations are collecting these: what are likely to be key costs that are feasible to estimate that we could ask for in site visits, phone calls? + Evaluation of the Commonwealth Fund’s Safety-Net Medical Home I iti ti Initiative Principal Investigator: Marshall Chin Chin, MD MPH University of Chicago + + Study overview 68 Safety Net Clinics Federally-qualified Non-FQHCs 5 states Colorado Oregon Idaho Massachusetts Pennsylvania community health centers + Evaluation Goals Evaluate intervention to inform health care organizations policymakers y and p Patient Economic Clinical Implementation Collect data that will be useful to participating clinics and the Qualis Q ali / MacColl intervention i te e tio team tea Evaluate the PCMH initiative as a whole, and not to rate individual clinics + 3 Questions Do the clinics become PCMHs? What are the outcomes? Clinical Cli i l quality lit Patient experience Staff experience Efficiency Utilization and charges Business Case What is associated with successful implementation? + Business Case PCMH administrative costs and revenues Disease Disease--specific clinical costs and revenues Overall costs and revenues Indirect costs and benefits + Medicaid Analysis Utilize Utili d data t across 6 states t t Compare health care cost/efficiency measures of patients enrolled in PCMH clinics and non-PCMH clinics Match patients by age, gender, race, zip code, clinical case mix Ambulatory Laboratory Total sensitive hospitalizations, ED visits testing, specialist referrals costs – PMPM + Study Team Marshall Chin, MD MPH: Principal Investigator Deborah Burnet, MD: Pediatric and CommunityCommunity-Based Research Lawrence Casalino, MD PhD: Structure, Quality, and Efficiency Melinda Drum, Drum PhD: Biostatistician Elbert Huang, MD MPH: Cost and Efficiency S h Lewis, Sarah L i MSPH MSPH: P Project j M Manger Michael Quinn, PhD: InIn-depth Interviews / Experience Questionnaires Thomas Summerfelt, PhD: Medicaid Analysis Hui Tang, MS: Programmer / Statistician Anusha Vable, MPH: Project Manager