Teaming Up with Patients, Families, and Community to Improve
advertisement
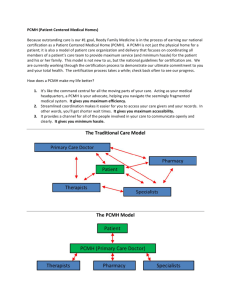
Teaming Up with Patients, Families, and Community to Improve Health Care Perry Dickinson, MD Department of Family Medicine University of Colorado Denver Outline • Transdisciplinary teamwork in the practice – clinicians and staff members • Patient- and family-centered care • Community focus • What do we know about teams? Which Way Are We Headed? Possibilities... • The PCMH model, if fully realized, will encourage and incent clinicians and practices to team up with patients, families, and the community to improve health • Coordination of care, population management, patient centered care all focus people in that direction • Dependent on payment, other structural issues – but also very dependent on us • Requires a cultural transformation PCMH is a Team Sport • No way for primary care clinicians to provide everything their patients need by themselves • Multiple levels of teamwork necessary: – Clinicians and staff members – Coordination with rest of health care system – Patients – personalized care plans, selfmanagement, patient advisory groups – Community partners Teams in the Practice • Multiple studies - using staff at higher level in team approach increases patient, staff, clinician satisfaction, quality and efficiency of care • Goal is everyone working at the top of their license and skills • Physicians are usually the biggest hurdle – hesitant to delegate tasks • Also cultural transformation for staff, patients Working Together Levels of Team Care • Multidisciplinary – each discipline independently contributes its expertise – work in parallel • Interdisciplinary – team members work together closely, communicate frequently to optimize care – each contributes skill and expertise to support the team’ work • Transdisciplinary – roles blur as functions overlap, interchange Who Is The Team? • Within the practice – everyone – front office, MAs, RNs, FNPs, PAs, physicians • Sometimes within the practice (or at least wellcoordinated with the practice) – mental and behavioral health, care managers, social services, pharmacists, others…. • Patients and families are important team members at all levels • “Medical Neighborhood” – other professionals or organizations that “share care” for your patients • Community resources Population Management • Chronic Care Model and PCMH both increase practice’s focus on populations of patients instead of the individuals who present for care • Responsibility for health (and quality indicators) of entire population of patients signed up for care • Increases awareness of importance of community issues in determining health Core Concepts of Patient- and Family-Centered Care • Respect and dignity – patient and family perspectives, cultural norms, beliefs, and choices are listened to and honored • Information Sharing – receive timely, complete, and accurate information • Participation - in care and decision-making encouraged and supported • Collaboration - on a practice-wide basis in design of delivery of care • Feedback – from patients is regularly sought and listened to Patient Input • Multiple ways to obtain patient input and feedback for practice change and improvement • Tremendous source of wisdom, ideas • Patient and family advisors – Advisory councils – Involvement in practice improvement teams • Takes time and patience (for both patients and practice) to develop fully • Patient experience survey as a quality measure Self Management Support • Providing patients with the information, tools, and support they need to take care of health problems in their daily lives • Not patient education • Personal health plans developed with patient prioritization, goal setting, action plan, monitoring • Requires that we partner with the patient and family in a different way Community Engagement • Many of the resources for selfmanagement support are in the community • Have to identify and partner with community groups • Should lead to assessment of strengths and problems in the community • Can lead to community-level advocacy Teamwork Is Central to the PCMH • So what do we know about teamwork? Crucial Elements of Teamwork • Mutual respect and trust • Willingness to abandon assumptions • Understanding of the distinct roles of each team member… • But, a willingness to blur roles when appropriate • Flexibility • Communication • Relationships! Effective Teams Need • • • • • • • Clear purpose - vision Coordination, time to meet Patience – it takes time to get there Protocols and procedures Conflict resolution skills (and willingness) Active participation by everyone Collective and individual accountability Barriers to Teamwork • Traditional hierarchical leadership • Reluctance to question “the leader” or “the expert” • Cultural differences – “cognitive maps” • Unwillingness to take on new roles • Communication styles • Lack of supportive organizational structure • Exclusion of team members Reality Even if you are on the right track, you’ll get run over if you just sit there ~ Will Rogers Thank You! • Contact Information: – Perry Dickinson: perry.dickinson@ucdenver.edu