Panel 1: Regina Neal - The New York Academy of Medicine
advertisement
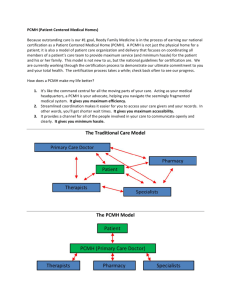
Care Coordination in the Patient-Centered Medical Home New York Academy of Medicine May 24, 2011 Starting Point Care Coordination -- one of the core functions of primary care and the PatientCentered Medical Home Goal – to provide patients with care that is: Accessible Comprehensive Continuous (relationship-based) Coordinated Definition of Care Coordination in the PCMH Care coordination is the deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient’s care to facilitate the appropriate delivery of health care services Myers D, et al. The Roles of the PCMH and ACOs in Coordinating Patient Care. AHRQ Publication No 11-M005-EF, Dec 2010 The Patient Centered Medical Home Medical home is a model for the organization of primary care that delivers the core functions of primary health care. The medical home encompasses five functions and attributes: Patient-Centered Comprehensive & Coordinated care Superb access System based approach to quality & safety http://www.pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483/what_is_pcmh_ Medical Home: What it Looks Like A health care setting that provides patients with: well-organized & on-time visits enhanced access with their own provider & care team for continuity (same day appointment availability, 24/7 telephone access, alternatives to the 1:1 visit) proactive care management (evidence base clinical care, panel management, reminder systems, registries) care coordination across settings (assistance with referrals, tracking for tests & referrals; care during transitions) patient activation, engagement & participation in decisions on care (patient centered customer driven) connections to community resources to extend resources for care focus on health outcomes & goals for improvement use of Health IT as tool to support the achievement of advanced primary care practice Health System: Community Resources Informed, Activated Patient Health Care Organization SelfDecision Delivery Clinical Management Support System Information Support Design Systems Productive Interactions Prepared, Proactive Practice Team Functional and Clinical Outcomes Medical Home: Aligned with (Chronic) Care Model Relationships Are Key “Coordination may be facilitated by certain design elements but it is more fundamentally a process of interaction among participants... specifically, coordination is carried out through relationships of shared goals, shared knowledge, and mutual respect.” (Gittell 2002, www.pcpcc.net) What’s Required to Make it Work Well-trained workforce organized as multidisciplinary care teams Mutual accountability among the team and between team and patients System designed to support care management & coordination through enhanced access, continuity and information availability Cross boundary cooperation & partnership among all provider types Technology infrastructure for information management & exchange Payment reform to support the work What Works Well-organized primary care itself better patient/staff experience, quality, reduced ED and hospital utilization Well-designed, targeted interventions to right patients (high risk/high need patients; transitions) Face-to-face interaction between patients and care coordinators to establish & maintain personal relationships Myers, D, AHRQ, Dec 2010 What Has Not Worked Disease management services delivered primarily by telephone (for Medicare beneficiaries) Targeted care coordination to low-risk Medicare patients Myers, D. AHRQ, Dec 2010 The Care Team Typically: primary care provider, nurse, medical assistant(s), front desk (greeter, registration) Associated/shared among care teams: referral specialist, nutritionist, social worker, pharmacist, behavioralist, financial specialist, educators Patient Challenge: Bridge the Gaps in the Core Care Team Front Desk Clerk Unlicensed medical assistants Licensed Nursing staff Primary Care Provider New Model: Continuous Capability in Team & Aligned Resources Front Trained MA Health Desk Medical Coaches Specialist Assistant Licensed Primary Nursing Care Staff Provider Referral Specialist, Pharmacist, Social Worker, Nutritionist, Behaviorist, Financial Specialist, Educator Referral & Test Tracking, Registry & Panel Management, Self Management Support Self Management Support, Medication Reconciliation, Clinical Issues Medical Assistants Health Coaches CDEs, Licensed Nurses Increasing Complexity of Patients Care Needs Unite Here Health Center, NYC Serves 10,000 patients -- who are members of several unions – and their families 55,000 visits annually Patients are low-wage, largely immigrant workers Center’s staff reflects its community Pharmacy, radiology, PT on site Capitated payments Principles Efforts to improve care need to focus on the sickest patients Doctors cannot successfully manage patients’ diseases alone Self-management is crucial for treating chronic conditions Using highly trained medical assistants for selfmanagement frees up clinicians (MD, DO, NP) to manage complex medical decisions Nelson, K. et al. Transforming the Role of Medical Assistants in Chronic Disease Management, Health Affairs, May 2010 What’s Possible Medical Assistants: well-trained by UHC to provide assistance to their medical provider All M.As trained to review charts to prepare for each day’s team huddle and for preventive care needs against protocols; to provide basic patient education Nine month intensive training available for M.A.s to move to being health coaches who provide clinical and selfmanagement support, e.g., monitor home BP & glucose; lead groups. Gives patients significant access to the care team EMR was key for registries to identify patients needing care management & coordination Results Data on outcomes show statistically significant improvements (p<0.05) % pts with HbA1c < 7% BP below 130/80 LDL < 100 mg/dL All A, B, C markers controlled increased from 13% to 36% Results Broader skill set for M.A.s creates new career pathways Allowed UHC to hire from its communities for cultural concordance Institutionalize strong relationships and shared backgrounds between patients and caregivers that are important to success of the model The Medical Home in the Neighborhood Community Health Workers Promotoras Extend the medical home to the neighborhood Cultural concordance Incorporate/address social factors of health in our medical homes Team Building Central to the PCMH model of care Team has shared responsibility for the health of the patient panel Building high-performance teams: Clinical & administrative systems to support team-based care and functions Clear roles among team members Permanent training environment High levels of communication within the team Team members with professional training actively mentor and train non professional/unlicensed team members Bodenheimer, Transforming Primary care: From Past Practice to Practice of the Future, Health Affairs, May 2010 Challenges Need medical training to adopt interprofessional learning opportunities as part of core curriculum Current scope of work regulations may require reform for some of these changes to take hold more widely and securely Team-building will require moving more responsibilities to non-physician team members; change management support needed (also see bullet above) Thank You