ch26 slides
advertisement

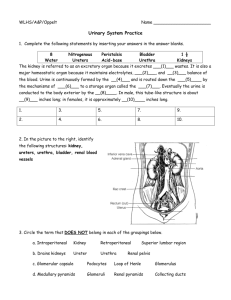
Principles of Anatomy and Physiology Thirteenth Edition Gerard J. Tortora • Bryan H. Derrickson Chapter 26 The Urinary System Copyright © 2012 by John Wiley & Sons, Inc. Diaphragm Esophagus RIGHT KIDNEY Left adrenal (suprarenal) gland Left renal vein Right renal artery RIGHT URETER LEFT KIDNEY Abdominal aorta Inferior vena cava URINARY BLADDER LEFT URETER Left ovary URETHRA Rectum Uterus Adrenal (suprarenal) gland Inferior vena cava Suprarenal arteries Renal artery Renal vein KIDNEY URETER LATERAL MEDIAL (b) Anterior view Transverse plane ANTERIOR Large intestine Stomach Liver Pancreas Renal artery and vein View Layers Inferior vena cava Peritoneum Abdominal aorta Body of L2 RENAL HILUM RENAL FASCIA LEFT KIDNEY ADIPOSE CAPSULE RENAL CAPSULE Spleen Rib RIGHT KIDNEY POSTERIOR (a) Inferior view of transverse section of abdomen (L2) Quadratus lumborum muscle SUPERIOR Lung Parasagittal plane Liver Diaphragm Adrenal (suprarenal) gland Twelfth rib Peritoneum Right kidney ADIPOSE CAPSULE RENAL CAPSULE Quadratus lumborum muscle Large intestine Hip bone POSTERIOR ANTERIOR (b) Parasagittal section through right kidney Layers RENAL FASCIA PATH OF URINE DRAINAGE: Nephron Collecting duct Renal hilum Minor calyx Renal cortex Renal artery Renal medulla Renal vein Major calyx Renal pelvis Renal column Renal pyramid in renal medulla Renal papilla Ureter Renal capsule Urinary bladder (a) Anterior view of dissection of right kidney SUPERIOR Renal capsule Renal cortex Minor calyx Renal artery Renal vein Major calyx Renal pelvis Ureter LATERAL MEDIAL (b) Posterior view of dissection of left kidney Glomerulus Frontal plane Afferent arteriole Peritubular capillary Efferent arteriole Interlobular vein Vasa recta Blood supply of nephron Interlobular artery Renal capsule Arcuate artery Interlobar artery Segmental artery Renal cortex Renal artery Renal vein Interlobar vein Renal pyramid in renal medulla Arcuate vein Interlobular vein (a) Frontal section of right kidney Renal artery Segmental arteries Interlobar arteries Arcuate arteries Interlobular arteries Afferent arterioles Glomerular capillaries Efferent arterioles Peritubular capillaries Interlobular veins Arcuate veins Interlobar veins (b) Path of blood flow Renal vein Renal capsule Renal corpuscle: Proximal convoluted tubule Glomerular (Bowman's) capsule Glomerulus Peritubular capillary Efferent arteriole Distal convoluted tubule Afferent arteriole Interlobular artery Interlobular vein Arcuate vein Renal cortex Renal cortex Renal medulla Renal medulla Arcuate artery Corticomedullary junction Renal papilla Loop of Henle: Minor calyx Descending limb FLOW OF FLUID THROUGH A CORTICAL NEPHRON Ascending limb Kidney Collecting duct Glomerular (Bowman's) capsule Proximal convoluted tubule Papillary duct Descending limb of the loop of Henle Renal papilla Ascending limb of the loop of Henle Distal convoluted tubule (drains into collecting duct) Minor calyx Urine (a) Cortical nephron and vascular supply Renal capsule Distal convoluted tubule Renal corpuscle: Proximal convoluted tubule Glomerular (Bowman's) capsule Glomerulus Peritubular capillary Afferent arteriole Efferent arteriole Interlobular artery Renal cortex Interlobular vein Renal cortex Renal medulla Arcuate vein Renal medulla Renal papilla Arcuate artery Peritubular capillary Minor calyx Corticomedullary junction Collecting duct FLOW OF FLUID THROUGH A JUXTAMEDULLARY NEPHRON Loop of Henle: Glomerular (Bowman's) capsule Proximal convoluted tubule Descending limb of the loop of Henle Kidney Descending limb Vasa recta Thick ascending limb Thin ascending limb Papillary duct Thin ascending limb of the loop of Henle Renal papilla Thick ascending limb of the loop of Henle Minor calyx Distal convoluted tubule (drains into collecting duct) Urine (b) Juxtamedullary nephron and vascular supply Microvilli Mitochondrion Apical surface Proximal convoluted tubule (PCT) Loop of Henle: descending limb and thin ascending limb Loop of Henle: thick ascending limb Most of distal convoluted tubule (DCT) Last part of DCT and all of collecting duct (CD) Intercalated cell Principal cell Renal corpuscle (external view) Parietal layer of glomerular (Bowman’s) capsule Afferent arteriole Mesangial cell Juxtaglomerular cell Capsular space Macula densa Ascending limb of loop of Henle Proximal convoluted tubule Mesangial cell Efferent arteriole Podocyte of visceral layer of glomerular (Bowman’s) capsule Endothelium of glomerulus (a) Renal corpuscle (internal view) Pedicel Glomerular capsule: Glomerulus Parietal layer Podocytes of visceral layer of glomerular capsule Visceral layer Afferent arteriole Juxtaglomerular cell Capsular space Ascending limb of loop of Henle Macula densa cell Simple squamous epithelial cells Efferent arteriole Proximal convoluted tubule LM 1380x (b) Renal corpuscle Renal corpuscle Afferent arteriole Glomerular filtration (filtration of blood plasma by glomerulus) Glomerular capsule Renal tubule and collecting duct Glomerulus Glomerular filtrate in renal tubule 1 2 Tubular reabsorption from glomerular filtrate into blood Efferent arteriole Peritubular capillaries 3 Tubular secretion Urine (contains excreted substances) from blood into glomerular filtrate Blood (contains reabsorbed substances) Podocyte of visceral layer of glomerular (Bowman’s) capsule Filtration slit Pedicel 1 Fenestration (pore) of glomerular endothelial cell: prevents filtration of blood cells but allows all components of blood plasma to pass through 2 Basal lamina of glomerulus: prevents filtration of larger proteins 3 Slit membrane between pedicels: prevents filtration of medium-sized proteins (a) Details of filtration membrane Pedicel of podocyte Filtration slit Basal lamina Lumen of glomerulus Fenestration (pore) of glomerular endothelial cell (b) Filtration membrane TEM 78,000x 1 GLOMERULAR BLOOD HYDROSTATIC PRESSURE (GBHP) = 55 mmHg 2 CAPSULAR HYDROSTATIC PRESSURE (CHP) = 15 mmHg 3 BLOOD COLLOID OSMOTIC PRESSURE (BCOP) = 30 mmHg Afferent arteriole Proximal convoluted tubule Efferent arteriole Glomerular (Bowman's) capsule Capsular space NET FILTRATION PRESSURE (NFP) = GBHP – CHP – BCOP = 55 mmHg – 15 mmHg – 30 mmHg = 10 mmHg Some stimulus disrupts homeostasis by Increasing Glomerular filtration rate (GFR) Receptors Macula densa cells of JGA detect increased delivery of Na+, Cl –, and water Input Control center Juxtaglomerular apparatus Return to homeostasis when response brings GFR back to normal Decreased secretion of nitric oxide Output Effectors Afferent arteriole constricts, which decreases blood flow through glomerulus Decrease in GFR Tubule cell Fluid in tubule lumen Na+ Peritubular capillary Na+ Na+ Paracellular reabsorption ATP Na+ Na+ ADP Na+ Na+ Key: Transcellular reabsorption Diffusion Basolateral membrane Apical membrane Tight junction Interstitial fluid Active transport Sodium–potassium pump (Na+/K+ ATPase) Fluid in tubule lumen Proximal convoluted tubule cell ATP 2 Na+ Na+ Peritubular capillary Na+ Na+ ADP Key: Na+–glucose symporter Glucose Glucose Glucose Glucose facilitated diffusion transporter Diffusion Tight junction Brush border (microvilli) Interstitial fluid Sodium–potassium pump Fluid in tubule lumen Proximal convoluted tubule cell Na+ Na+ H+ Peritubular capillary HCO3– H+ ATP HCO3– Na+ HCO3– Na+ H2CO3 ADP Metabolic reactions CA CO2 Key: Na+/H+ antiporter Na+ H2O CO2 CO2 HCO3– facilitated diffusion transporter Diffusion Interstitial fluid (a) Na+ reabsorption and H+ secretion Sodium–potassium pump Fluid in tubule lumen Peritubular capillary Na+ HCO3– Na+ Na+ Key: H+ H+ CA ADP HCO3– H2CO3 H2CO3 CO2 H2O ATP H2O CO2 HCO3– Na+/H+ antiporter HCO3– facilitated diffusion transporter Diffusion Sodium–potassium pump (b) HCO3– reabsorption Fluid in tubule lumen Cl– K+ Ca2+ Mg2+ Urea H2O Proximal convoluted tubule cell Diffusion Osmosis Peritubular capillary Cl– K+ Ca2+ Mg2+ Urea H2O Fluid in tubule lumen Vasa recta Thick ascending limb cell Na+ ATP Na+ ADP Na+ 2Cl– K+ Cations: Na+ K+ Ca2+ Mg2+ Na+ Na+ 2Cl– 2Cl– 2Cl– K+ Cations Key: Na+–K+–2Cl– symporter Apical membrane (impermeable to water) Interstitial fluid is more negative than fluid in tubule lumen Leakage channels Sodium–potassium pump Diffusion Fluid in tubule lumen Principal cell Peritubular capillary K+ K+ ATP Na+ Na+ Na+ ADP Na+ K+ Key: Diffusion Interstitial fluid Leakage channels Sodium–potassium pump Some stimulus disrupts homeostasis by Increasing Osmolarity of plasma and interstitial fluid Receptors Osmoreceptors in hypothalamus Nerve impulses Input Control center Hypothalamus and posterior pituitary Return to homeostasis when response brings plasma osmolarity back to normal ADH Increased release of ADH Output Effectors H2O Principal cells become more permeable to water, which increases facultative water reabsorption Decrease in plasma osmolarity Afferent arteriole Glomerular (Bowman's) capsule Glomerulus Distal convoluted tubule Efferent arteriole 100 300 Proximal convoluted tubule 90 300 300 350 350 150 Interstitial fluid in renal cortex 350 Collecting duct 550 550 750 750 350 550 550 80 Interstitial fluid in renal medulla 750 70 900 Loop of Henle 65 65 Papillary duct Dilute urine Vasa recta Loop of Henle Juxtamedullary nephron and its blood supply together Glomerular (Bowman’s) capsule Afferent arteriole Distal convoluted tubule Efferent arteriole 300 400 600 Osmotic gradient 800 1000 Proximal convoluted tubule Interstitial fluid in renal medulla 200 HO H2O 2 300 H2O Interstitial fluid in renal cortex Flow of tubular fluid 320 300 Collecting duct 300 H2O 300 320 100 Na+Cl– 380 H2O 200 1 580 Symporters in thick ascending limb cause buildup of Na+ and Cl– in 780 renal medulla H2O 2 Countercurrent flow 1200 through loop of Henle establishes osmotic gradient H2O Na+Cl– Blood flow Presence of Na+–K+–2Cl– symporters Glomerulus 400 H2O 400 H2O H2O 3 Principal cells in collecting duct reabsorb more water when ADH is present 400 500 Na+Cl– 600 H2O Na+Cl– 600 H 2O 600 Urea 800 1000 800 980 H2O 1200 Loop of Henle (a) Reabsorption of Na+, Cl–, and water in long-loop juxtamedullary nephron 1200 1200 4 Urea recycling 700 800 causes buildup of urea in renal medulla H2O 900 H2O Na+Cl– 1000 Na+Cl– 1100 Papillary duct 1200 Concentrated urine (b) Recycling of salts and urea in vasa recta RENAL CORPUSCLE PROXIMAL CONVOLUTED TUBULE Glomerular filtration rate: 105–125 mL/min of fluid that is isotonic to blood Reabsorption (into blood) of filtered: Water 65% (osmosis) Na+ 65% (sodium–potassium pumps, symporters, antiporters) K+ 65% (diffusion) Glucose 100% (symporters and facilitated diffusion) Amino acids 100% (symporters and facilitated diffusion) Cl– 50% (diffusion) HCO3– 80–90% (facilitated diffusion) Urea 50% (diffusion) Ca2+, Mg2+ variable (diffusion) Filtered substances: water and all solutes present in blood (except proteins) including ions, glucose, amino acids, creatinine, uric acid EARLY DISTAL CONVOLUTED TUBULE Reabsorption (into blood) of: Secretion (into urine) of: H+ variable (antiporters) NH4+ variable, increases in acidosis (antiporters) Urea variable (diffusion) Creatinine small amount Water 10–15% (osmosis) Na+ 5% (symporters) CI– 5% (symporters) Ca2+ variable (stimulated by parathyroid hormone) LATE DISTAL CONVOLUTED TUBULE AND COLLECTING DUCT Reabsorption (into blood) of: At end of PCT, tubular fluid is still isotonic to blood (300 mOsm/liter). LOOP OF HENLE Water 5–9% (insertion of water channels stimulated by ADH) Na+ 1–4% (sodium–potassium pumps and sodium channels stimulated by aldosterone) HCO3– variable amount, depends on H+ secretion (antiporters) Urea variable (recycling to loop of Henle) Reabsorption (into blood) of: Water 15% (osmosis in descending limb) Na+ 20–30% (symporters in ascending limb) K+ 20–30% (symporters in ascending limb) CI– 35% (symporters in ascending limb) HCO3– 10–20% (facilitated diffusion) Ca2+, Mg2+ variable (diffusion) Secretion (into urine) of: Urea variable (recycling from collecting duct) At end of loop of Henle, tubular fluid is hypotonic (100–150 mOsm/liter). Urine Secretion (into urine) of: K+ variable amount to adjust for dietary intake (leakage channels) H+ variable amounts to maintain acid–base homeostasis (H+ pumps) Tubular fluid leaving the collecting duct is dilute when ADH level is low and concentrated when ADH level is high. Ureters Ureteral openings Frontal plane Rugae of mucosa Peritoneum Detrusor muscle Trigone Internal urethral orifice Internal urethral sphincter (involuntary) Urethra External urethral sphincter in deep muscles of perineum (voluntary) Hip bone (pubis) External urethral orifice Anterior view of frontal section Sagittal plane Uterus Urinary bladder Pubic symphysis Rectum Urethra Vagina External urethral orifice (a) Sagittal section, female Sagittal plane Urinary bladder Rectum Pubic symphysis Prostatic urethra Prostate Deep muscles of perineum Membranous urethra Penis Spongy urethra Testis Scrotum (b) Sagittal section, male External urethral orifice Degenerating pronephros Urogenital ridges Yolk sac Mesonephros Allantois Mesonephric duct Hindgut Metanephros: Cloacal membrane Ureteric bud Cloaca Metanephric mesoderm (a) Fifth week Gut Degenerating pronephros Allantois Urinary bladder Genital tubercle Urogenital sinus Mesonephros Rectum Mesonephric duct Metanephros (b) Sixth week Gonad Urinary bladder Urogenital sinus Rectum Ureter (c) Seventh week Gonad Urinary bladder Kidney Urogenital sinus Anus Ureter Rectum (d) Eighth week Kidney Urinary bladder Ureter Urogenital sinus Anus Allantois (e) Anterior view, 8-week embryo