Adrenal medulla
advertisement

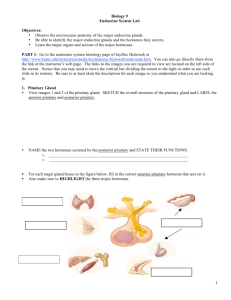
INTERFERENCES TO NUTRITIONAL NEEDS DUE TO REGULATORY MECHANISM DYSFUNCTION: ENDOCRINE DISORDERS Adrenal and Pituitary Dysfunction 2009 ENDOCRINE SYSTEM • FUNCTION: • Works with the nervous system • Coordinates the response of the body to internal and external stimuli • Goal: to maintain homeostasis ENDOCRINE GLANDS • • • • • • • Pituitary Thyroid Parathyroid Adrenals Islets of Langerhans in pancreas Ovaries testes WHAT DO ENDOCRINE GLANDS DO? • Secrete their products directly into the bloodstream • Differ from EXOCRINE GLANDS which secrete through ducts onto epithelial surface or into the GI tract HORMONES DEFINED: Chemical substances secreted by the endocrine glands WHAT DO THEY DO? • Hormones help regulate organ function • They work with the nervous system GOAL OF HORMONES • Keep concentration of hormones in bloodstream constant • When levels drop: rate of production increases • When levels are high: rate of production decreases • NEGATIVE FEEDBACK SYSTEM: mechanism for regulation of hormone concentration in the bloodstream EXAMPLE OF NEGATIVE FEEDBACK SYSTEM CONTROL OF INSULIN SECRETION: • When blood glucose levels hormone insulin secreted • Insulin glucose uptake by the cells blood glucose levels • THUS: the action of insulin ( blood glucose levels) is the opposite of the condition that stimulated insulin secretion ( blood glucose levels) HYPOTHALMUS • Link between the nervous system and endocrine system • It controls both the posterior and the anterior pituitary gland ABNORMALITIES • Based on overproduction and underproduction PITUITARY GLAND: ANTERIOR AND POSTERIOR • ANOTHER NAME: hypophysis • Master gland of endocrine system • Secretes hormones that control the secretion of hormones by other endocrine glands • It is controlled by the hypothalmus POSTERIOR PITUITARY HORMONES SECRETED: • Vasopressin (or ADH or antidiuretic hormone) STIMULATED BY: • Increase in osmolality of the blood • Decrease in blood pressure PRIMARY FUNCTION: • To control the excretion of water by the kidney POSTERIOR PITUITARY HORMONES SECRETED: • Oxytocin STIMULATED BY: • Pregnancy • childbirth PRIMARY FUNCTION: • Facilitate milk ejection during lactation • Increase force of uterine contractions during L&D POSTERIOR PITUITARY: QUICK SUMMARY • DI (Diabetes Insipidus) ADH urine • SIADH (syndrome of inappropriate antidiuretic hormone) ADH – Dilute urine – Water retained – Low sodium ANTERIOR PITUITARY HORMONES SECRETED control growth, metabolic activity and sexual development: • FSH – Follicle Stimulating Hormone • LH – Luteinizing Hormone • Prolactin • ACTH - Adrenocorticotropic hormone • TSH – Thyroid stimulating hormone • GH – Growth hormone,or somatotropin • MSH - Melanocyte stimulating hormone PITUITARY: QUICK SUMMARY ANTERIOR PITUITARY: • Hypopituitarism: deficiency of one or more hormones resulting in metabolic and sexual dysfunction • Panhypopituitarism: decreased production of all anterior pituitary hormones • Hyperpituitarism: hormone oversecretion – ACTH secretion of MSH – PRL(prolactin) inhibits secretion of gonadotropins and sex hormones galactorrhea , amenorrhea, infertility – GH gigantism and acromegaly ADRENAL GLANDS There are two glands Each has two parts • Adrenal medulla • Adrenal cortex HORMONE SECRETION: is regulated by the pituitary ACTH ADRENAL GLANDS Adrenal medulla at the center of the gland secretes catecholamines Catecholamines regulate metabolic pathways to promote catabolism of stored fuels to meet caloric needs • (dopamine, epinephrine, and norepinephrine) • EPINEPHRINE: fight or flight response ADRENAL GLANDS Adrenal cortex at the outer portion of the gland secretes steroids and sex hormones: STEROIDS: • Glucocorticoids (cortisol) • Mineralocorticoids (aldosterone) PURPOSE OF STEROIDS: • Regulate body’s response to physical and psychological stress ADRENAL CORTEX HORMONES AND WHAT THEY DO GLUCOCORTICOIDS: important to glucose metabolism • Eg: increased secretion results in elevated blood glucose Glucocorticoids are often administered to patients to reduce inflammatory response to tissue injury and to suppress allergic manifestations • SE: diabetes, osteoporosis, peptic ulcer, poor wound healing ADRENAL CORTEX HORMONES AND WHAT THEY DO MINERALOCORTICOIDS (aldosterone): • Acts on the kidney and GI tract to increase Na absorption in exchange for excretion of K or hydrogen ions • Secretion occurs in the presence of angiotensin II ADRENAL CORTEX HORMONES AND WHAT THEY DO SECRETION OF ADRENAL SEX HORMONES are controlled by ACTH ANDROGENS: Exerts effects similar to those of male sex hormones ESTROGEN: Adrenal gland secretes small amounts of female sex hormones ADRENAL GLAND: QUICK SUMMARY OF DYSFUNCTION ADRENAL CORTEX • function adrenal insufficiency adrenal crisis, Addison’s crisis loss of aldosterone and cortisol • function cortisol (hypercortisolism or Cushings) – Mineralocorticoids hyperaldosteronism – androgens ADRENAL MEDULLA – Pheochromocytoma: catecholamines PHEOCHROMOCYTOMA • Tumor, usually benign on the adrenal medulla, unknown cause • Affects men and women equally, runs in families • Causes *****hypertension • Severity of symptoms depends on the amount of epinephrine and nor-epinephrine secretion PHEOCHROMOCYTOMA S&S • • • • • • Tremor Headache Flushing Anxiety Hyperglycemia palpitations • • • • • Profuse diaphoresis Chest pain N&V Heat intolerance Wgt loss DRUGS WHICH PROMOTE HYPERTENSIVE CRISIS IN PHEOCROMOCYTOMA • • • • • • • Trycyclic antidepressants droperidol (Inapsine): sedative/hypnotic glucagon (GlucaGen) metoclopramide (Clopra): antiemetic phenothiazines (Melloril): antipsychotic Naloxone (Narcan): opiod antagonist Foods high in tyramine PREPARE FOR SURGERY • Stabalize BP with IV antihypertensives of long acting alpha adrenergic blockers: phenoxybenzamine (Dibenzyline) • Control tachycardia and dysrhythmias: propanolol (Inderal) • Suppress catecholamine synthesis: calcium channel blockers: nicardipine (Cardene) DIAGNOSTIC EVALUATIONS FOR PHEOCROMOCYTOMA • Measurement of urine and plasma levels of catecholamines: elevated with pheochromocytoma 24 hour urine for – VMA (vanillylmandelic acid - product of catecholamine metabolism) – Metanephrine – Catecholamines All are elevated with pheochromocytoma PREP FOR 24 HOUR URINE TEST FOR VMA: Avoid for 2-3 days: coffee,tea,cola,cocoa,bananas,citrus fruits, chocolate, vanilla,licorice,aspirin,antihypertensives prior to the VMA test SURGICAL REMOVAL OF PHEOCROMOCYTOMA TUMOR REMOVAL OF TUMOR WITH ADRENALECTOMY • Anesthesia and Manipulation of the tumor during surgery may cause release of stored epinephrine and norepinephrine hypertensive crisis and changes of HR • If both adrenal glands are removed: corticosteroids replacement is necessary POSTOP AFTER REMOVAL OF PHEOCHROMOCYTOMA • Hypotension, hypoglycemia may occur because of the sudden withdrawal of excessive amounts of catecholamines • Urine and plasma levels of catecholamines are measured to determine whether surgery has been successful • Receive volumn expanders for possible hypovolemia, hemorrhage and shock ADDISON’S DISEASE • Adrenocortical insufficiency • Results when adrenal cortex function is inadequate to meet the patient’s need for cortical hormones CAUSED BY: • Decrease secretion of ACTH • Dysfunction of hypothalamic-pituitary control • Dysfunction of adrenal gland tissue • Removal of both adrenal glands STEROIDS AND ADRENAL INSUFFICIENCY • MOST COMMONLY CAUSED BY therapeutic use of corticosteroids • Corticosteroids therapy suppresses production of glucocorticoids through negative feedback by causing atrophy of the adrenal cortex • Glucocorticoids MUST BE WITHDRAWN gradually to allow for pituitary production of ACTH and activation of adrenal cells to produce cortisol WHAT HAPPENS WITH ADDISON’S DISEASE? • Insufficiency of adrenocortical steroids causes problems through loss of aldosterone and cortisol WHAT HAPPENS WITH CORTISOL IN ADDISONS Cortisol – gluconeogenesis (making of glucose from proteins) hypoglycemia – depletion of liver and muscle glycogen WHAT HAPPENS WITH DECREASED ALDOSTERONE? • ALDOSTERONE – K EXCRETION HYPERKALEMIA DYSRRHYTMIAS AND CARDIAC ARREST – Na and water excretion • Hyponatremia; craves salt, low BP • Hypovolemia – Hyperkalemia reabsorption of hydrogen ions acidosis S&S OF ADDISON’S DISEASE • ****Muscular weakness, fatigue, emaciation • Anorexia, GI symptoms(N,V,D) dehydration/wgt loss • melanocyte stimulating hormone – Dark pigmentation of skin, knuckles, knees, elbows and mucous membranes • c/o BEING TIRED AND WEAK (CARDINAL SYMPTOM) – increased during stress from hypoglycemia LABORATORY EVAL FOR ADDISON’S DISEASE • • • • • Low blood glucose Low serum sodium elevated serum potassium High WBC (leukocytosis) ***low levels of adrenocortical hormones in bld/urine • Low serum cortisol levels TEACHING PT WITH ADDISON’S DISEASE • Teach increase Na to prevent hyponatremia: illness/heat/stress • Lifelong hormone replacement • Teach to prevent stress, prevent fatigue • Teach to increase CHO and protein to prevent hypoglycemia • Lifelong problem ADDISONIAN CRISIS Disease at it’s worst • Severe hypotension and shock • Fever • N/V, abdominal pain, diarrhea WITH SLIGHT OVEREXERTION, EXPOSURE TO COLD, INFECTIONS OR DECREASE IN SALT: leads to circulatory collapse, shock, death TO PREVENT CRISIS • Must replace corticosteroids • No salt restriction - leads to crisis • No diuretics - leads to crisis MANAGEMENT OF ADDISON’S CRISIS • IV fluids, glucose and electrolytes and sodium for dehydration • Replace missing cortisol and aldosterone deficiency: hydrocortisone • For Na and K imbalance give mineralocorticoids hormone: fludrocortisone (Florinef) • Glucagon for hypoglycemia CUSHINGS SYNDROME (Hypercortisolism) Increased production of ACTH DISEASE RESULTS from too much corticosteroids being secreted by the adrenal cortex CAUSE; adrenocortical tumors, or pituitary tumor secreting ACTH causing increased secretion of glucocortiocoids IF CAUSE OF CUSHINGS IS PITUITARY TUMOR • Pituitary tumor causes increased production of ACTH • treatment of choice is removal of pituitary gland WHAT IS HAPPENING IN CUSHINGS? • Problems with nitrogen, CHO, mineral metabolism • Slow turnover of fatty acids: – – – – – total body fat Truncal obesity, thin arms and legs Buffalo hump: fat pads on neck, back, shoulders Moon face Pendulous abdomen PROBLEMS IN CUSHINGS • BREAKDOWN OF TISSUE PROTEIN urine nitrogen excretion 1. muscle mass (muscle wasting, weakness), edema 2. Thin skin 3. Bone density loss PROBLEMS IN CUSHINGS: • levels corticosteroids 1. killing of lymphocytes 2. Shrinks organs 3. eosinophils and macrophages ALL IMMUNE RESPONSE; leading to increased infections PROBLEMS IN CUSHINGS: • 1. 2. 3. 4. 5. ANDROGEN PRODUCTION Acne Hirsuitism ( hair growth) Masculination of women Oligomenorrhea Decreased libido PROBLEMS IN CUSHINGS: • 1. 2. 3. 4. SKIN CHANGES FROM BLOOD VESSEL FRAGILITY: Bruises Thin skin Wound won’t heal Reddish striae on abdomen, thighs, and upper arms from degrading effect of cortisol on collagen PROBLEMS IN CUSHINGS: PSYCHOSOCIAL: • Emotional lability PROBLEMS IN CUSHINGS: • Hypertension from water and sodium retention DIAGNOSIS OF CUSHINGS SYNDROME • Cortisol levels • Hypernatremia – increased Na leads to fluid retention • Hypokalemia – leads to arrhythmias • Hyperglycemia from cortisol • 24 hour urine test measure cortisol levels: NURSING CARE PT WITH CUSHINGS • • • • • • • Protect from infection Skin care Decrease stress ROM VS check for hypertension Check for edema I&O, daily wgts, fluid restriction • Low cal, low Na, high protein, high potassium, high calcium and high vit D • Accuchecks: insulin prn • Sores won’t heal because of increased sugar NON-SURGICAL MANAGEMENT: DRUG THERAPY: • mitotane (Lysodren): adrenal cytotoxic agent used to interfere with ACTH production • aminoglutethimide (Elipten): decreases cortisol production RADIATION THERAPY: tx pituitary tumor if that is the cause SURGERY: remove the pituitary tumor causing the adrenal hyperfunction total hypophysectomy (removal of the pituitary gland) HYPER-ALDOSTERONISM (CONN’S SYNDROME) • secretion of aldosterone mineralocorticoid CAUSED BY: secretion of aldosterone from one or both adrenal glands caused by a tumor RESULT: aldosterone affects the renal tubules hypernatremia, hypokalemia, metabolic acidosis: Hydrogen ion excretion Conn’s syndrome continued • Hypernatremia blood volume BP PITUITARY GLAND • Master gland of endocrine system • Secretes hormones that control the secretion of hormones by other endocrine glands • Pituitary controlled by the hypothalmus HYPOPITUITARISM RESULTS from disease of pituitary gland or of the hypothalamus, tumor, trauma, radiation RESULTS in deficiencies of 1 or more anterior pituitary hormones to metabolic problems Sexual dysfunction TX: replacement of deficient hormones: corticosteroids, thyroid hormone, sex hormones, gonadotropins DX: skull xray, CT scan (pituitary tumor) CHANGES IN OTHER HORMONES • ACTH and TSH are the most life threatening because they lead to in secretion of hormones from the adrenal and thyroid gland • gonadotropins (LH and FSH) changes sex function in men and women (sterility and infertility) CHANGES IN OTHER HORMONES • GH in children • GH in adults (osteoporosis) growth retardation bone destruction SURGICAL TX FOR PITUITARY TUMOR HYPOPHYSECTOMY (partial or complete removal of pituitary gland) TWO APPROACHES: • Craniotomy • Transphenoidal (through the nose and into the floor of sinuses TRANSPHENOIDAL POSTOP CARE • HOB up to decrease headache • Look for CSF leak: clear drainage from nose or postnasal drip (constant swallowing); check for glucose in drainage. If + then means CSF • Leak usually resolves in 72 hours • May need spinal tap to decrease CSF pressure • Antibiotics to prevent meningitis POSTOP TEACHING FOR REMOVAL OF PITUITARY GLAND • No bending • No straining at stool for 2 mo postop • No toothbrushing until sutures removed and incision heals; 10 days • If gland removed client has permanent diabetis insipidis ABSENCE OF PITUITARY GLAND Alters function of many body systems: • Menstruation ceases • Infertility occurs REPLACEMENT THERAPY WITH STEROIDS AND THYROID HORMONE NECESSARY • Replacement hormones: cortisone and thyroid hormones, testosterone for impotence in men and estrogen for women for atrophy of vagina, human pituitary gonadotropin may restore fertility in women FUNCTION OF POSTERIOR PITUITARY: ADH DIABETES INSIPIDUS HYPOFUNCTION OF THE POSTERIOR PITUITARY of ADH or vasopressin • Water metabolism problem caused by an ADH • polyuria, dilute urine, dehydration, increased thirst, low specific gravity (less than 1.005) • Tx: lifelong aqueous vasopressin (Pitressin) therapy TREATMENT TX: fluid and electrolytes, I&O, wgts, IV’s to replace losses Administer hormone replacement: vasopressin (Pitressin) and vasopressin tannate IM; Lypressin nasal spray POSTERIOR PITUITARY: ADH SIADH: syndrome of inappropriate antidiuretic hormone • SIADH involves hypersecretion of ADH from the posterior pituitary gland • With continual secretion of ADH the body retains water leading to water intoxication • CAUSE: bronchogenic carcinoma (malignant lung cells synthesize and release ADH • ALSO occurs following brain surgery, brain tumors, infection PROBLEMS: • • • • • • elevated urine specific gravity Decreased urinary output (retaining fluids) Serum Na decreases (dilutional problem) May have respiratory/cardiac problems May develop cerebral edema which leads to seizures Limbs are small (no edema) gaining wgt only in body SIADH SYMPTOMS AND TREATMENT TX: • lithium carbonate (Lithobid) uncommon use , demeclocycline (Declomycin) commonly used • diuretics, • restrict fluids to promote fluid loss and gradual increase in serum sodium NURSING CARE • • • • I&O Wgt Blood chemistries Keep HOB flat or slightly up to decrease the secretion of ADH • Neuro checks • CONSIDER THIS SERIOUS PROBLEM HYPERPITUITARISM • Hormone oversecretion that occurs with pituitary tumors • Tumors occur most often in the anterior pituitary cells that produce GH, Prolactin (PRL) and ACTH OF GH GIGANTISM • Slow progression • If dx early changes preventable • If not dx early changes in soft tissue, face, hands, feet, skin are irreversible • After tx changes in all but skeletal ones • If occurs before puberty causes rapid growth in length of all bones GH ACROMEGALY • CAUSES: – skeletal thickness, – hypertrophy of skin – Enlargement of visceral organs – GH blocks action of insulin Hyperglycemia: