Chapter 10
Eating Disorders
Chapter Outline
•
•
•
Clinical Description
Etiology of Eating Disorders
Treatments of Eating Disorders
Introduction of Eating Disorders To The DSM
•
Eating disorders appeared in the DSM for the first
time in 1980
•
•
one subcategory of disorders beginning in
childhood or adolescence.
In the DSM-IV, the eating disorders anorexia
nervosa and bulimia nervosa formed a distinct
category
•
reflecting the increased attention they had
received from clinicians and researchers
Eating Disorders In DSM-5
•
Binge eating disorder is a distinct diagnostic
category that is now included in DSM-5.
It was also said that there was improved
criteria for anorexia nervosa and bulimia
nervosa introduced.
•
Prevalence U.S. Data
•
•
Lifetime prevalence in the U.S. in 2001 and 2003
Anorexia nervosa (women 0.9%; men 0.3%)
Bulimia nervosa (women 1.5%; men 0.5%)
Binge eating disorder (women 3.5%; men 2.0%)
•
•
•
While there is a clear sex difference, it is still the case
overall that 1 in 3 or 1 in 4 cases involve boys or young
men.
•
International Prevalence
Prevalence of binge eating disorder around the world
(Kessler et al., 2013):
•
•
•
•
Lifetime prevalence of binge eating disorder was higher than
the rate for bulimia nervosa (1.4% vs. 0.8%).
The disorders were similar in terms of age of onset (late teen
years to early 20s) but it was slightly earlier for those with
bulimia nervosa.
Bulimia was also distinguished by having a longer
persistence (6.5 years vs. 4.3 years).
There are growing clinical accounts of eating
disorders appearing with greater prevalence among
younger people.
Canadian Prevalence
•
According to Statistics Canada ’s 2002 Mental Health and
Well-being Survey (Government of Canada, 2006)
0.5% of Canadians 15 years of age or older reported
an eating disorder diagnosis in the preceding 12
months.
Women were more likely than men to report an eating
disorder: 0.8% vs. 0.2%
Among young women aged 15 to 24, 1.5% reported
that they had an eating disorder.
1.7% of Canadians met 12-month criteria for an
eating attitude problem.
•
•
•
•
Do Those With Eating Disorders Get
Treatment?
•
Only a relatively small proportion of people who
require treatment actually sought treatment within
the past year (e.g., 15.6% of those with bulimia
nervosa) (Hudson et al., 2007)
•
treatment was obtained typically from the
general medical sector.
Clinical Description: The Most Common Eating Disorder
• There is great heterogeneity in eating disorder symptom
expression
•
•
•
The most common diagnosis (occurring in between 40 to 70% of
clients) is a category called eating disorder not otherwise
specified (EDNOS) (Thomas, Vartanian, & Brownell, 2009).
This general diagnostic category has been a “catch-all” category
that underscores problems inherent in the current diagnostic
system.
EDNOS is referred to as a “clinical condition” rather than a
category per se because more evidence is needed to elevate it to
the diagnostic category designation.
DSM-5
•
•
DSM-5 dropped the EDNOS description for new designations.
Unspecified Feeding Or Eating Disorder
•
•
•
can be used for any condition that causes clinically significant distress or impairment
but does not meet diagnostic thresholds.
can be used when there is insufficient information such as in hospital emergency room
situations.
The other broad category is “other specified feeding or eating disorder.”
•
•
•
•
applies to atypical, mixed, or subthreshold conditions
includes a variety of conditions, including subthreshold bulimia nervosa and
subthreshold binge eating disorder.
includes night eating syndrome, which is a repetitive tendency to wake up and eat
during the night and then get quite upset about it.
Includes purging disorder - this is a form of bulimia that involves self induced vomiting
or laxative use at least once a week for a minimum of six months.
Purging Disorder
•
People with purging disorder have levels of
disturbed eating and associated forms of
psychopathology that are comparable with patients
with other eating disorders
•
One clear feature of purging disorder is high
impulsivity.
Commonalities of Anorexia and Bulimia
•
The diagnoses of anorexia nervosa and
bulimia nervosa share several clinical
features
•
•
the most important being the intense fear of being
overweight
There are some indications that these may
not be distinct diagnoses but may be two
variants of a single disorder.
•
Co-twins of people diagnosed with anorexia nervosa, for
example, are themselves more likely than average to have
bulimia nervosa (Walters & Kendler, 1994).
Anorexia Nervosa (AN)
•
•
Anorexia—loss of appetite
Nervosa—appetite loss due to emotional reasons
Term a misnomer because most patients do not
lose their appetite or interest in food – they
become preoccupied with food
•
DSM Criteria For Anorexia Nervosa
•
DSM-IV: The person must refuse to maintain a normal body
weight and weighs less than 85% of what is considered
normal for that person’s age and height.
•
•
•
Weight loss is typically achieved through dieting, although purging (selfinduced vomiting, heavy use of laxatives or diuretics) and excessive exercise
can also be used.
DSM-5 has modified this criterion and no longer refers to the 85% guideline.
Instead, the revised criterion is restriction of energy intake resulting in
significantly low body weight within the context of a person ’s age, sex, and
physical health status.
The person has an intense fear of gaining weight and the
fear is not reduced by weight loss.
DSM Criteria For Anorexia
• They have a distorted sense of their body
shape.
• They maintain that even when emaciated, they are overweight or that
•
certain parts of their bodies, particularly the abdomen, buttocks, and
thighs, are too fat.
To check on their body size, they typically weigh themselves
frequently, measure the size of different parts of the body, and gaze
critically at their reflections in mirrors.
• In females, the extreme emaciation causes
amenorrhea the loss of the menstrual
period.
• This criterion has been eliminated from DSM- 5
Linking Self-esteem And Self-evaluation With
Thinness
•
The self-esteem of people with anorexia nervosa is closely
linked to maintaining thinness. The tendency to link selfesteem and self-evaluation with thinness is known as over
evaluation of appearance.
•
•
among people with acute anorexia nervosa, lower body weight is
associated with increased self-esteem
Clients with anorexia nervosa overestimate their own body
size and choose a thin figure as their ideal.
Development Of Anorexia Nervosa
•
Typically begins in the early to middle teenage
years, often after an episode of dieting and exposure
to life stress.
•
•
the prevalence of anorexia among children and adolescents
is increasing.
Comorbidity is high.
•
•
men and women at risk for eating disorders are also prone
to depression, panic disorder, and social phobia (Gadalla,
2008).
Women were at substantially greater risk for mania,
agoraphobia, and substance dependence.
Comorbidity With Substance Use
• High rate of co-occurring eating
disorders and substance use disorders
•
a meta-analysis conducted in Spain found that there was
no link between anorexia nervosa and illicit drug use, but
there was a clear link evident between bulimia nervosa
and drug use (Calero-Elvira et al., 2009).
•
Canadian investigators have specifically tied drug use to
the bingeing and dieting cycle (see Gadalla & Piran,
2007).
Physical Changes with AN
•
•
•
•
•
•
•
blood pressure
heart rate
bone mass
Kidney and gastrointestinal problems dry skin
Nails become brittle
Hormone levels change
Mild anemia
Prognosis of Anorexia Nervosa
•
•
•
•
70% of patients recover
•
Recovery often takes six or seven years
Relapses are common
•
Changing distorted thoughts about thinness is difficult;
particularly, in cultures that value thinness
Death rates are 10 X > than general population
Death rates 2X > than patients with other psychological
disorders
•
There is no other disorder that matches the mortality risk
inherent in anorexia nervosa (Attia, 2010).
Mortality In Eating Disorders
•
A meta-analysis of 36 studies found that:
5.1 deaths per 1,000 person years for anorexia
3.0 deaths per 1,000 person years for eating disorders not otherwise
specified
.7 deaths per 1,000 person years for bulimia nervosa.
•
•
•
•
•
•
Predictors of death include lower BMI and older age at first presentation for
treatment and alcohol misuse (Arcelus et al., 2011).
Death most often results from physical complications of the illness or from
suicide (Birmingham et al., 2005; Katzman, 2005).
A BC survival analysis concluded that anorexia is associated with a 25-year
reduction in life expectancy (Harbottle, Birmingham, & Sayani, 2008).
Suicide in Eating Disorders
•
A review found that suicide rates are not elevated in
bulimia nervosa like they are in anorexia nervosa
(Franko & Keel, 2006)
•
•
people with bulimia nervosa are more likely to
have suicide ideation.
one in five deaths attributed to anorexia involved
suicides (Arcelus et al., 2011).
Bulimia Nervosa (BN)
• Bulimia is from a Greek word meaning “ox hunger.”
• Involves episodes of rapid consumption of a large amount of
food (binge), followed by compensatory behaviours (purge).
•
•
Binge = eating excessive amount of food in < 2 hours
Typically occur in secret
May be triggered by stress
Purge = vomiting, fasting, or excessive exercise
•
•
DSM-5
•
The DSM-5 defines a binge as eating an excessive amount of
food eating within a defined period (e.g., two hours).
•
•
•
The episode of binge eating must also include a sense of lack of
control over the behaviour.
DSM-5 stipulates that the binge eating and compensatory
behaviour must continue at least once a week for three
months.
Bulimia nervosa is not diagnosed if the bingeing and purging
occur only in the context of anorexia nervosa and its extreme
weight loss; the diagnosis in such a case is anorexia nervosa,
binge eating-purging type.
Characteristics of Binging
•
•
•
•
•
Binge episodes tend to be preceded by poorer than average
social experiences, self-concepts, and moods.
Stressors that involve negative social interactions may be
particularly potent elicitors of binges.
Bulimics have high levels of interpersonal sensitivity, as
reflected in large increases in self-criticism following negative
social interactions.
Continues until the person is uncomfortably full (Grilo, Shiff man,
& Carter-Campbell, 1994).
Binge episodes are often followed by deterioration in selfconcept, mood state, and social perception.
Loss Of Control
•
•
•
•
•
•
The person who is engaged in a binge often feels a loss of control
over the amount of food being consumed.
Foods that can be rapidly consumed, especially sweets such as ice
cream or cake, are usually part of a binge.
Some people with bulimia nervosa sometimes ingest an enormous quantity of
food during a binge, often more than what a normal person eats in an entire day
binges are not always as large as the DSM implies, and there may be wide
variation in the caloric content consumed by individuals with bulimia nervosa
during binges.
Bulimics are usually ashamed of their binges and try to conceal
them.
They report that they lose control during a binge, even to the point of
experiencing something akin to a dissociative state, perhaps losing awareness of
what they are doing or feeling that it is not really they who are bingeing.
DSM-5 And Binging
•
the DSM-IV diagnosis of bulimia nervosa
required that the episodes of bingeing
and purging occur at least twice a week
for three months.
•
•
This wasn’t a well-established cut-off point.
in DSM-5, once a week for binging now
sufficient to meet the criterion.
Bulimia Nervosa And Fear Of
Gaining Weight
•
Garfinkel (2002) observed that “a morbid fear of
fat” is an essential diagnostic criterion for bulimia
nervosa because
•
•
•
(1) it covers what clinicians and researchers view as the
“core psychopathology” of bulimia nervosa;
(2) it makes the diagnosis more restrictive
(3) it makes the syndrome more closely resemble the
related disorder of anorexia nervosa.
Bulimia Nervosa And Fear Of Gaining Weight
•
This focus on fear of becoming fat and negative appraisals of
the self for being fat are involved in a relatively new line of
research on a phenomenon known as fat talk.
Fat talk refers to the tendency for friends, particularly
female friends, to take turns disparaging their bodies to
each other.
Both average weight and overweight target people were
seen as more likeable if they were depicted engaging in fat
talk (Barwick et al., 2012)
Fat talk seems to reflect a highly defensive and negative
sense of self.
•
•
•
Development of Bulimia
•
•
Bulimia nervosa typically begins in late adolescence or early
adulthood.
Extreme body dissatisfaction was found among 7–8% of both
girls and boys in Nova Scotia
these children were only in Grade 5
these data suggest that children particularly at risk can be
identified at a fairly young age (Austin, Haines, &
Veugelers, 2009).
It was found among only girls that as their body mass
index increased, their body satisfaction decreased.
•
•
•
Development of Bulimia Nervosa
•
•
•
many people with bulimia nervosa are somewhat
overweight before the onset of the disorder and that the
binge eating often starts during a dieting episode.
Long-term follow-ups of bulimia nervosa clients reveal
that about 70% recover, although about 10% remain fully
symptomatic (Keel et al., 1999).
Temporal studies also identify diagnostic crossover.
•
More than 18% with AN eventually develop BN, while
approximately 7% of those with BN eventually develop AN (see
Keel, Brown, Holland, & Bodell, 2012).
Other Features of Bulimia Nervosa
•
•
•
•
•
•
•
•
•
Physical side effects
Potassium depletion
Diarrhea
Changes in electrolytes
Irregularities in the heartbeat
Tearing of tissue in the stomach and throat
Loss of dental enamel
Swollen salivary glands
Mortality appears to be much less common in bulimia
nervosa than in anorexia nervosa (Keel & Mitchell, 1997).
•
•
•
Binge Eating Disorder
BED is included in DSM-5 .
This disorder includes recurrent binges (at least once per week
for at least three months), lack of control during the bingeing
episode, and distress about bingeing, as well as other
characteristics.
Binge eating episodes must involve at least three of the
following:
• eating more rapidly than normal
• eating until feeling uncomfortably full
• eating alone due to feelings of embarrassment
• eating large amounts of food when not feeling hungry
• feeling disgusted with oneself or depressed or very guilty.
Binge Eating Disorder
•
It is distinguished from anorexia by the absence of
weight loss and from bulimia by the absence of
compensatory behaviours (purging, fasting, or
excessive exercise).
•
Binge Eating Disorder seems more treatment
responsive than anorexia nervosa or bulimia nervosa.
•
Frequent binge eating among 1 in 25 women
Binge Eating Disorder
•
•
•
Is linked with impaired work and social functioning, depression, low selfesteem, substance abuse, and dissatisfaction with body shape (Spitzer
et al., 1993; Striegel-Moore et al., 1998).
Risk factors for developing BED include:
•
•
•
•
•
childhood obesity,
critical comments regarding being overweight,
low self-concept,
depression,
childhood physical or sexual abuse (Fairburn et al., 1998).
The average life-term duration of BED (14.4 years) may be greater than the
duration of AN (5.9 years) or BN (5.8) years (see Pope et al., 2006).
Aetiology: Genetics
•
The role of genetic factors in eating disorders has been largely
ignored, relative to other types of disorders, because of a prevailing
emphasis on socio-cultural factors
•
Both anorexia nervosa and bulimia nervosa run in families.
• First-degree relatives of young women with anorexia nervosa are about four times
•
•
•
more likely than average to have the disorder themselves (Strober et al., 1990).
Twin studies of eating disorders also suggest a genetic influence.
Most studies of both anorexia and bulimia report higher identical than fraternal
concordance rates.
Research has also shown that key features of the eating disorders,
such as dissatisfaction with one ’s body and a strong desire to be thin,
appear to be heritable (Rutherford et al., 1993).
Eating Disorders And The Brain
•
•
•
•
The hypothalamus is a key brain centre in regulating hunger and
eating (see de Krom et al., 2009).
Research on animals with lesions to the lateral hypothalamus indicates that
they lose weight and have no appetite (Hoebel & Teitelbaum, 1966).
The paraventricular nucleus has also been implicated (Connan &
Stanley, 2003).
The levels of some hormones regulated by the hypothalamus, such
as cortisol, are indeed abnormal in people with anorexia; rather
than causing the disorder, however, these hormonal abnormalities
occur as a result of self-starvation, and levels return to normal
following weight gain (Doerr et al., 1980).
Problems With Biological Explanations
• The weight loss of animals with hypothalamic lesions does not
parallel what is known about anorexia
•
•
these animals appear to have no hunger and become indifferent to
food,
clients with anorexia continue to starve themselves despite being
hungry and having an interest in food.
• The hypothalamic model does not account for body-image
disturbance or fear of becoming fat.
• A dysfunctional hypothalamus thus does not seem a highly
likely factor in anorexia nervosa.
Endogenous Opioids And Eating Disorders
•
Endogenous opioids are substances produced by the body that
reduce pain sensations, enhance mood, and suppress appetite,
at least among those with low body weight.
Starvation may increase the levels of endogenous opioids,
resulting in a positively reinforcing euphoric state (Marrazzi
& Luby, 1986)
excessive exercise would increase opioids and thus be
reinforcing (Davis, 1996; Epling & Pierce, 1992).
•
•
•
Hardy and Waller (1988) hypothesized that bulimia is mediated
by low levels of endogenous opioids, which are thought to
promote craving; a euphoric state is then produced by the
ingestion of food, thus reinforcing bingeing.
Neurotransmitters Related To Eating
Disorders
•
•
•
•
Low levels of serotonin metabolites and serotonin in people with bulimia
Serotonin metabolites have been linked with the negative mood and selfconcept changes that precipitate binge episodes (Steiger et al., 2005).
Hildebrandt et al. (2010) have advanced a development model that links
serotonin and estrogen in bulimia nervosa.
Key premises of this model are that genetic polymorphisms at birth limit the serotonergic
system, and associated genes may be further limited by exposure to harsh environments in
the form of maladaptive parenting styles. Subsequent environmental estrogens predispose
female adolescents to weight gain, thus increasing the perceived need to engage in dieting
that may become excessive.
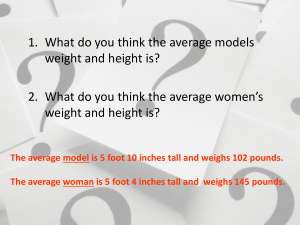
Socio-Cultural Variables
•
Throughout history, the standards societies have set for the ideal body,
especially the ideal female body, have varied greatly.
The famous nudes painted by Rubens in the seventeenth century;
according to modern standards, these women are chubby.
In recent times in our culture, there has been a steady progression
toward increasing thinness as the ideal.
•
•
•
•
•
Playboy magazine centrefolds became thinner between 1959 and 1978
(Garner, Garfinkel, Schwartz, & Thompson, 1980).
A follow-up investigation of Playboy centrefolds found the trend toward portrayals of
increasing thinness has levelled off and may even be reversing somewhat (Sypeck et
al., 2006).
While the images have suggested increasing heaviness, the normative
weight displayed is still considerably lower than is healthy.
Socio-Cultural Variables: Barbie
•
•
•
When it comes to the promotion of unrealistic images,
females consistently feel more pressure than males.
To achieve the same figure as the Barbie doll, the average
American woman would have to increase her bust by 12
inches, reduce her waist by 10, and grow to over seven feet
in height (Moser, 1989).
The insidious effects of exposing young girls to Barbie dolls
with unrealistic body images was shown in an experiment
(see Dittmar, Halliwell, & Ive, 2006).
•
Five- and six-year-old girls exposed to Barbie images suffered lower
body esteem and greater desire to achieve the thin ideal.
Socio-cultural Variables: Do
They Apply To Men?
•
•
•
There is an increasing focus in the research literature on how many
of the same issues that have been focused on among females also
tend to apply to males as well.
There is growing evidence of the role of body dissatisfaction and how
the idealization of a hyper-mesomorphic lean and muscular body
ideal for males is providing the kind of pressure and dissatisfaction
that underscores problems in body image, eating behaviours, and
associated problems in health and well-being (see McFarland &
Petrie, 2012).
A male body dissatisfaction has been created recently (McFarland &
Petrie, 2012).
Scarlett O’Hara Effect
•
•
•
•
Women respond to socio-cultural pressures by eating lightly
in an attempt to project images of femininity.
Research has confirmed that women who are portrayed as eating
heavily are indeed seen as less feminine and more masculine than
women who are portrayed as eating light meals.
Pliner and Chaiken have coined the term the Scarlett
O’Hara effect to refer to this phenomenon of eating lightly to
project femininity.
In Gone with the Wind, Mammy admonishes Scarlett to eat
a meal prior to going to a barbecue so that she would
appear dainty by eating very little.
Overweight?
• While cultural standards and pressures to be thin were
•
increasing, more and more people were becoming overweight.
The prevalence of obesity has doubled since 1900; currently 20 to 30% of
North Americans are overweight and there are continuing references to an
obesity epidemic.
• Pinel, Assanand, and Lehman (2000) attribute the increasing
•
prevalence of obesity to an evolutionary tendency for humans to
eat to excess to store energy in their bodies for a time when food
may be less plentiful.
If so, this tendency to over consume is clearly at odds with unrealistic pressures
to maintain ideal body weights.
Perceptions of Children of Being Overweight
•
•
•
•
•
•
According to the World Health Organization’s 2002 Health
Behaviour in School-aged Children (HBSC) Canadian Survey
(see Government of Canada, 2006), 31% of Canadian young
women from grades 6 to 10 thought that they were too fat.
The proportion increased with age and, by Grade 10, 44% indicated that
they were too fat.
The number of dieters increased from 1950 to 1999
Men 7% to 29%
Women 14% to 44%
An Ontario study found that among more than 2,000 girls aged
10 to 14, 29.3% were dieting and 1 in 10 had maladaptive eating
attitudes, suggesting the presence of an eating disorder (McVey,
Tweed, & Blackmore, 2004).
The Impact of Media
• The contemporary research focus has shifted to an analysis of the
relative impact of various media (e.g., television vs. magazines) on
body image ideals and dissatisfaction.
•
•
•
A study of 12-year-olds in Western Canada found that increases in eating disorder
symptoms were associated with increased exposure to fashion magazines and these
increases were not associated with the amount of television viewed (Vaughan &
Fouts, 2003).
An Australian study also found that the amount of television watched was unrelated
to body image variables for either girls or boys (Tiggemann, 2005).
However, watching soap operas was associated with increased drive for thinness in
girls and boys.
• The reasons for watching television mattered:
• there was a negative impact on body image variables if television
was watched for reasons of social learning or as a diversion from
negative mood states.
Culture
•
•
•
•
•
•
•
•
Excessive body fat has negative connotations, such as being unsuccessful and
having little self-control.
Obese people are viewed by others as less smart and are stereotyped as being
lazy.
Investigations suggest this anti-fat bias is pervasive so that even the most obese
people tend to endorse these views; however, the bias seems more automatic
among thinner people, according to measures of implicit cognitive processing
(Schwartz et al., 2006).
the media promotes these stereotypes.
A content analysis of 18 primetime television situation comedies conducted by
researchers in Calgary found that
females with below average weights were overrepresented in these shows
the heavier the female character, the more likely she was to have negative comments
directed toward her (Fouts & Burggraf, 2000).
these negative comments were especially likely to be reinforced by audience laughter.
Pro-Ana Websites
• “pro-ana” websites glorify starvation and reinforce
•
•
irrational beliefs about the importance of thinness and
the perceived rewards of being dangerously thin.
While some people seem to turn to these websites in a
desperate search for coping advice, others may simply
be looking for tips and techniques to help become more
anorexic (see Mulveen & Hepworth, 2006).
A common theme among people viewing the sites is that
they equated thinness with happiness (Rodgers,
Skowron, & Chabrol, 2012).
Activity Anorexia
• Epling and Pierce from the University of Alberta have suggested
•
•
•
that some people become anorexic because of a pursuit of
fitness rather than a pursuit of thinness.
Activity anorexia refers to the loss of appetite when engaged in
physical activity.
dancers, relative to models, had higher rates of anorexia and more disturbed eating
attitudes (Garner & Garfi nkel, 1980).
Models and dancers share a pressure to maintain ideal appearance, but dancers
also engage in much more strenuous physical activity.
• Pierce and Epling suggest that two interrelated motivational
•
•
factors account for activity anorexia:
food deprivation increases the reinforcement effectiveness of physical activity
physical activity decreases the reinforcement effectiveness of food.
Gender Influences
• The primary reason for the greater prevalence of eating disorders
among women than among men is that women appear to have been
more heavily influenced by the cultural ideal of thinness.
•
Women are typically valued more for their appearance, whereas men gain esteem
more for their accomplishments.
• Women apparently are more concerned than men about being thin, are
more likely to diet, and are thus more vulnerable to eating disorders.
• There is a growing belief that appearance pressures are increasing on
young males as well.
•
These increasing pressures are reflected by a heightened drive for muscularity, which
can take the extreme form of muscle dysmorphia (i.e., an obsession about not being as
muscular as desired).
Cross-Cultural Studies
•
•
•
•
Eating disorders are far more common in industrialized
societies, such as the United States, Canada, Australia, and
Europe, than in non-industrialized nations
Eating disorders are more evident in Western cultures (Keel &
Klump, 2003).
However, it is also generally concluded that the gap is closing, with rising
levels of eating disorder in non-Western cultures as well as rising levels of
research interest, as reflected by an increasing number of publications
(Soh & Walter, 2013).
Young women who immigrate to industrialized Western cultures
may be especially prone to developing eating disorders owing to
the experience of rapid cultural changes and pressures (Geller
& Thomas, 1999)
Cognitive-Behavioural Views
• Cognitive-behavioural theories of anorexia nervosa emphasize fear of
fatness and body-image disturbance as the motivating factors that make
self-starvation and weight loss powerful reinforcers.
• Behaviours that achieve or maintain thinness are negatively reinforced
by the reduction of anxiety about becoming fat.
• Dieting and weight loss may be positively reinforced by the sense of
mastery or self-control they create (Fairburn, Shafran, & Cooper, 1999;
Garner, Vitousek, & Pike, 1997).
• Some theories also include personality and socio-cultural variables to
explain how fear of fatness and body-image disturbances develop.
The Effects On Cognition When Exposed to
Media
•
•
•
•
The media’s portrayal of thinness as an ideal, being overweight, and a tendency
to compare oneself with especially attractive others all contribute to
dissatisfaction with one’s body (Stormer & Thompson, 1996).
Even brief exposure to pictures of fashion models can instill negative moods in
young women and women who are dissatisfied with their bodies seem especially
vulnerable when exposed to these images (Pinhas et al., 1999).
Exception:
The thinspiration effect:
• Chronic dieters actually feel thinner after looking at idealized images of
the thin body and this motivates them to diet (Mills, Polivy, Herman, &
Tiggemann, 2002).
• This can begin a process of dieting that can ultimately lead to distress
among dieters unable to attain unrealistic body-image standards.
The Timing Of Binging
•
It is known that bingeing results frequently when diets are broken
(Polivy & Herman, 1985).
•
•
•
a lapse that occurs in the strict dieting of a person with anorexia nervosa is
likely to escalate into a binge.
The purging following an episode of binge eating can again be
seen as motivated by the fear of weight gain that the binge elicited.
Clients with anorexia who do not have episodes of binging and
purging may have a more intense preoccupation with and fear of
weight gain (Schlundt & Johnson, 1990) or may be more able to
exercise self-control.
Psychodynamic Views
•
•
Most propose that the core cause lies in disturbed parent–child
relationships and agree that certain core personality traits,
such as low self-esteem and perfectionism, are found among
individuals with eating disorders.
Psychodynamic theories propose that the symptoms of an
eating disorder fulfill some need, such as the need to increase
one’s sense of personal effectiveness (the person succeeds in
maintaining a strict diet) or to avoid growing up sexually (by
being very thin, the person does not achieve the usual female
shape) (Goodsitt, 1997).
Psychodynamic Views
• Some focus on family relationships.
• Hilde Bruch (1980) - anorexia nervosa is an attempt by
•
•
•
children who have been raised to feel ineffectual to gain
competence and respect and to ward off feelings of
helplessness, ineffectiveness, and powerlessness.
This sense of ineffectiveness is created by a parenting style in which the
parents’ wishes are imposed on the child without considering the child’s
needs or wishes.
Children reared in this way do not learn to identify their own internal states
and do not become self-reliant.
When faced with the demands of adolescence, the child seizes on the
societal emphasis on thinness and turns dieting into a means of acquiring
control and identity.
Minuchin: Family Systems Theory
•
•
•
The symptoms of an eating disorder are best understood by
considering both the afflicted person and how the symptoms
are embedded in a dysfunctional family structure.
The child is seen as physiologically vulnerable (although the
precise nature of this vulnerability is unspecified) and the
child’s family has several characteristics that promote the
development of an eating disorder.
The child’s eating disorder plays an important role in helping
the family avoid other conflicts. Thus, the child ’s symptoms
are a substitute for other conflicts within the family.
Minuchin: Family Systems Theory
• According to Minuchin et al. (1975), the families of children with
•
eating disorders exhibit the following characteristics:
Enmeshment
•
Families have an extreme form of overinvolvement and intimacy in which
parents may speak for their children because they believe they know
exactly how they feel.
• Overprotectiveness
•
Family members have an extreme level of concern for one another’s
welfare.
• Rigidity
•
Families have a tendency to try to maintain the status quo and avoid dealing
effectively with events that require change (e.g., the demand that
adolescence creates for increased autonomy).
• Lack of conflict resolution
•
Families either avoid conflict or are in a state of chronic conflict.
Characteristics Of Families
•
•
•
•
Self-reports consistently reveal high levels of conflict in the
family among people with eating disorders (e.g., Hodges,
Cochrane, & Brewerton, 1998).
However, reports of parents do not necessarily indicate high levels of
family problems.
Disturbed family relationships do seem to characterize some
families; however, the characteristics that have been
observed, such as low levels of support, only loosely fit the
family systems theory.
These family characteristics could be a result of the eating
disorder and not a cause of it.
The Need For Observational Studies Of
Families
• In one of the few observational studies conducted,
parents of children with eating disorders did not appear to
be very different from control parents.
• Baker, Whisman, and Brownell (2000) studied eating
attitudes in university students and their parents and
found that the students’ attitudes and behaviours were
tied more closely to perceived parental characteristics
(i.e., criticism from parents) than to actual parental
characteristics.
Childhood Abuse and Eating Disorders
• Some studies have indicated that self-reports of childhood sexual abuse
are higher than normal among people with eating disorders, especially
those with bulimia nervosa (Steiger & Zanko, 1990).
• A study conducted in Toronto found that 25% of women with eating
disorders reported the experience of previous sexual abuse; it also
correlated a history of sexual abuse with greater psychological disturbance
(DeGroot, Kennedy, Rodin, & McVey, 1992).
• Bulimic women, relative to normal eaters, had higher levels of childhood
abuse and that the presence and the severity of abuse predicted more
extreme psychopathology (Leonard, Steiger, & Kao, 2003).
Poor Record of Ethics
• Hunger and malnutrition experiments were conducted in aboriginal
communities in the 1940’s and 1950’s by leading nutritional experts
employed by the Government of Canada.
• According to Mosby (2013), unethical, controlled experiments involving lack
of informed consent were conducted in various regions, including research
on the Northern Cree people in Northern Manitoba.
• It is alleged that researchers identified people, both young and old, who
were starving and denied some of them food and nutrients so they could
study them.
• Up to one thousand children were kept malnourished and sometimes
starved because it suited research purposes.
Retrospective Reports Of Personality
• This research described clients with anorexia as having been
perfectionistic, shy, and compliant before the onset of the
disorder.
• It described people with bulimia as having the additional
characteristics of histrionic features, affective instability, and an
outgoing social disposition (Vitousek & Manke, 1994).
• It is important to remember, however, that retrospective reports
that involve recalling what the person was like before diagnosis
can be inaccurate and biased by awareness of the person ’s
current problem.
High in Neuroticism
•
People with anorexia and people with bulimia are
high in neuroticism and anxiety and low in selfesteem (Bulik et al., 2000).
•
•
The role of neuroticism as a long-term predictor of
anorexia was also confirmed in a recent twin study
(Bulik et al., 2006).
Those people with AN or BN also score high on a
measure of traditionalism, indicating strong
endorsement of family and social standards (Bulik et
al., 2000).
Narcissism/Perfectionism and Eating
Disorders
•
•
•
AN and BN clients are characterized by high levels of
narcissism that persist even when the eating disorder is in
remission (Lehoux, Steiger, & Jabalpurlawa, 2000;
Steiger et al., 1997).
The use of a narcissistic defensive “poor me” style has
treatment implications because it predicts greater
treatment dropout (Campbell, Waller, & Pistrang, 2009).
Eating disorders have been related to increased
perfectionism
Perfectionism and Eating Disorders
•
Hewitt and Flett (1991b) created a multidimensional
perfectionism scale that assesses:
•
•
•
•
•
•
self-oriented perfectionism (setting high standards for oneself)
other-oriented perfectionism (setting high standards for others)
socially prescribed perfectionism (the perception that high standards
are imposed on the self by others)
Weight-restored and underweight anorexics had elevated
scores on self-oriented perfectionism.
Underweight anorexics had higher scores on socially
prescribed perfectionism
Anorexic individuals who engage in excessive exercise are
distinguished by remarkably high levels of self-oriented
perfectionism (Davis, Kaptein, Kaplan, Olmsted, &
Woodside, 1998).
An Interactive Model
• Bulimic symptoms are elevated among females who are characterized not
•
only by perfectionism, but also by body dissatisfaction and low selfesteem.
They have exceptionally high standards yet recognize a sense of self-dissatisfaction for not
attaining these impossible standards.
• Perfectionistic self-presentation
• these individuals try to create an image of perfection and are highly focused on
minimizing the mistakes they make in front of other people (see Hewitt, Flett, &
Ediger, 1995; Hewitt et al., 2003).
• One significant limitation of this work is that the causal role of these
dimensions of perfectionism has yet to be firmly established by
longitudinal, prospective research on the role of these dimensions in the
onset of eating disorders.
Treatment Of Eating
Disorders
• It is often difficult to get a person with an eating disorder into treatment
•
because the person typically denies that he or she has a problem.
the majority of people with eating disorders, up to 90% of them, are not in treatment (Fairburn et al.,
1996) and those who are in treatment are often resentful.
• Some people with bulimia only wind up in treatment because their dentist has
spotted one key indicator: the erosion of teeth enamel as a result of the
stomach acid coming into contact with the teeth during vomiting.
• Hospitalization is required frequently to treat people with anorexia so that their
•
•
ingestion of food can be gradually increased and carefully monitored.
Weight loss can be so severe that intravenous feeding is necessary to save the person’s life.
Weight restoration is the immediate primary goal in the treatment of anorexia (for a discussion, see
Attia, 2010).
Relapse Rates
•
One vexing problem is a high rate of relapse in the treatment of
eating disorder.
•
•
a recent study of 100 anorexia nervosa patients in Toronto who were
treated successfully found that 41% of them relapsed during the one-year
follow-up period (Carter et al., 2012).
Carter et al. (2012) found in their study that relapse was more
likely for those clients who:
•
•
•
Binge-purge anorexia subtype
Had more OCD-like checking behaviours.
Lower motivation to recover predicted subsequent relapse.
Medications
•
Interest has focused on fluoxetine (Prozac) (e.g., Fluoxetine Bulimia Nervosa
Collaborative Study Group, 1992).
•
•
•
•
•
Fluoxetine was shown to be superior to a placebo in reducing binge eating and vomiting; it also
decreased depression and lessened distorted attitudes toward food and eating.
Optimism about the use of fluoxetine in treatment was reduced substantially by a
well-designed study conducted jointly in Toronto and New York City; this
investigation of patients with anorexia found no benefits following weight
restoration (Walsh et al., 2006).
Fluoxetine is not consistently effective.
More patients drop out of drug therapy in studies on bulimia than drop out of the
kind of cognitive-behavioural interventions (Fairburn, Agras, & Wilson, 1992).
No drugs have been found effective in treating anorexia nervosa.
Psychological Treatment Of
Anorexia Nervosa
• Therapy for anorexia is generally believed to be a two tiered
•
•
•
process.
immediate goal
Help each person gain weight in order to avoid medical complications and the
possibility of death.
Operant-conditioning behaviour therapy programs have been somewhat successful in
achieving weight gain in the short term (Hsu, 1990). In these programs, the
hospitalized patient is isolated as much as possible and then rewarded for eating and
gaining weight with mealtime company; access to a television set, radio, or stereo;
walks with a student nurse; mail; and visitors.
• The second goal of treatment
•
long-term maintenance of weight gain has not yet been reliably achieved by medical,
behavioural, or traditional psychodynamic interventions (Wilson, 1995).
Effectiveness of CBT
•
CBT resulted in significant improvements and it was
significantly better at preventing relapse (Carter et al., 2009).
•
•
CBT has promise as a means of treating anorexia and this was supported
in more recent research comparing CBT with interpersonal therapy using
a RCT design in this investigation, both kinds of treatment were quite
effective (see Carter et al., 2011).
According to Wilson, Grilo, and Vitousek (2007), CBT is
regarded as the treatment of choice for bulimia nervosa and
binge eating disorder, while a specific version of family therapy
is most favoured for treating anorexia nervosa
Family Therapy and Anorexia
•
•
Family therapy is the principal mode of treatment for anorexia.
•
One report, however, suggests that as many as 86% of 50 anorexic
daughters treated with their families were still functioning well when
assessed at times ranging from three months to four years after treatment
(Rosman, Minuchin, & Liebman, 1976).
•
•
has not yet been sufficiently studied for its long-term effects.
A better-controlled follow-up study of psychodynamically oriented family therapy
confirmed these findings.
Patients with early-onset anorexia and a short history of it maintained
their weight gains from family therapy for five years following treatment
termination (Eisler et al., 1997).
The Maudsley Approach
• Labour-intensive method that recruits parents and requires them
•
•
to find creative ways to feed their children and restore them to a
healthy weight.
Parents are taught that they are not to blame, but at the same
time, they are taught to be supportive and not critical.
Lock et al. (2010) in a RCT comparing family therapy and
individual therapy found that both were effective, but family
therapy was slightly superior in terms of achieving full remission
of anorexia.
•
However, a re-analysis of original data supporting the Maudsley model
yielded an important caveat. Treasure and Russell (2011) reported that fiveyear follow-up data showed the clear superiority of family therapy vs.
individual therapy in the treatment of anorexia, but neither treatment
approach was very useful for those adolescents who had anorexia for three
years of more.
Psychological Treatment Of
Bulimia Nervosa
•
•
The cognitive-behavioural therapy (CBT) approach of Fairburn (1985;
Fairburn, Marcus, & Wilson, 1993) is the best validated and current
standard for the treatment of bulimia.
In Fairburn ’s therapy, the client is encouraged to question society’s
standards for physical attractiveness.
•
•
•
•
•
They must also uncover and then change beliefs that encourage them to starve
themselves to avoid becoming overweight.
They must be helped to see that normal body weight can be maintained without severe
dieting and that unrealistic restriction of food intake can often trigger a binge.
They are taught that all is not lost with just one bite of high-calorie food and that snacking
need not trigger a binge that would be followed by induced vomiting or taking laxatives.
Altering this all-or-nothing thinking can help patients begin to eat more moderately.
They are also taught assertion skills to help them cope with unreasonable demands
placed on them by others, and they learn more satisfying ways of relating to people, as
well.
The CBT Approach
•
This CBT approach has the patient bring small amounts
of forbidden food to eat in the session. Relaxation is
employed to control the urge to induce vomiting.
Unrealistic demands and other cognitive distortions—
such as the belief that eating a small amount of highcalorie food means that the person is an utter failure and
doomed never to improve—are continually challenged.
Treating Body Image Disturbance
• A 2006 review concluded that CBT is the most commonly used
•
and empirically supported treatment for body image disturbance
in the normal population (Farrell, Shafran, & Lee, 2006).
These data and other recent developments have led some
authors to conclude that no other treatment has greater efficacy
than CBT (see Mitchell, Agras, & Wonderlich, 2007).
•
•
almost half of the clients relapse after four months (Halmi et al.,
2002).
Predictors of relapse include less initial motivation for change and
higher initial levels of food and eating preoccupation (Halmi et al.,
2002).
•
At least half of the clients in some controlled
studies do not recover
•
•
May be that significant numbers of the patients in these
studies have psychological disorders in addition to eating
disorders, such as borderline personality disorder,
depression, anxiety, and marital distress (Wilson, 1995).
Another possibility is suggested by data indicating that those
people who begin with negative self-efficacy judgements
about their ability to recover actually tend to be the ones
who are more treatment resistant and do indeed take longer
to recover (Pinto et al., 2008).
Prevention of ED in Canada
• Stice and Shaw (2004) conducted a meta-analysis of 23
•
•
prevention studies and confirmed that the intervention effects
have varied widely and have ranged from no effect to significant
effects.
The overall effect of prevention was deemed to range from small
to medium in magnitude.
larger effects occurred when:
•
•
•
•
the prevention was aimed at high risk participants vs. all participants
an interactive program as opposed to a didactic.
Multiple sessions also increased the effect
if only females were targeted and females were 15 years or older.
Copyright
•
Copyright © 2014 John Wiley & Sons Canada, Ltd. All rights
reserved. Reproduction or translation of this work beyond
that permitted by Access Copyright (The Canadian Copyright
Licensing Agency) is unlawful.
Requests for further
information should be addressed to the Permissions
Department, John Wiley & Sons Canada, Ltd.
The
purchaser may make back-up copies for his or her own use
only and not for distribution or resale. The author and the
publisher assume no responsibility for errors, omissions, or
damages caused by the use of these programs or from the
use of the information contained herein.