Chapter 61
advertisement

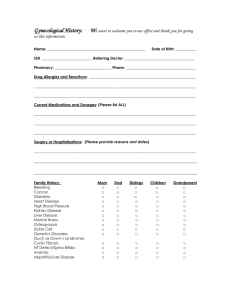
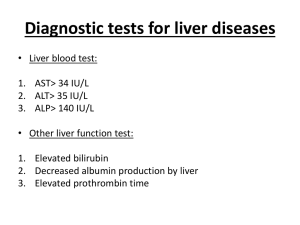
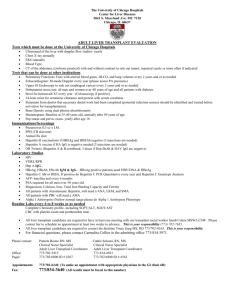
Care of Patients with Liver Problems Chapter 61 Mrs. Kreisel MSN, RN NU130 Adult Health Summer 2011 Cirrhosis • Cirrhosis is extensive scarring of the liver, usually caused by a chronic reaction to hepatic inflammation and necrosis. • Complications depend on the amount of damage sustained by the liver. • In compensated cirrhosis, the liver has significant scarring but performs essential functions without causing significant symptoms. Complications • • • • • • Portal hypertension Ascites Bleeding esophageal varices Coagulation defects Jaundice Portal-systemic encephalopathy with hepatic coma • Hepatorenal syndrome • Spontaneous bacterial peritonitis Esophageal Varices Etiology • Known causes of liver disease include: • Alcohol • Viral hepatitis • Autoimmune hepatitis • Steatohepatitis • Drugs and toxins • Biliary disease • Metabolic/genetic causes • Cardiovascular disease Clinical Manifestations • In early stages, signs of liver disease include: • Fatigue • Significant change in weight • GI symptoms • Abdominal pain and liver tenderness • Pruritus Clinical Manifestations (Cont’d) • In late stages, the signs vary: • Jaundice and icterus (pigmentation of tissue, membranes and secreations with bile pigments) • Dry skin • Rashes • Petechiae, or ecchymoses (lesions) • Warm, bright red palms of the hands • Spider angiomas: associated with cirrhosis of the liver, branched growth of dilated capillaries on the skin looking like a spider • Peripheral dependent edema of the extremities and sacrum Abdominal Assessment • • • • Massive ascites Umbilicus protrusion Caput medusae (dilated abdominal veins) Hepatomegaly (liver enlargement) Liver Dysfunction Other Physical Assessments • Assess nasogastric drainage, vomitus, and stool for presence of blood • Fetor hepaticus (breath odor) • Amenorrhea • Gynecomastia, testicular atrophy, impotence • Bruising, petechiae, enlarged spleen • Neurologic changes • Asterixis ( also known as liver flap or liver tremors: abnormal involuntary jerking muscles) Laboratory Assessment • Aminotransferase serum levels and lactate dehydrogenase may be elevated. • Alkaline phosphatase levels may increase. • Total serum bilirubin and urobilinogen levels may rise. • Total serum protein and albumin levels decrease. Laboratory Assessment (Cont’d) • Prothrombin time is prolonged; platelet count is low. • Hemoglobin and hematocrit values and white blood cell count are decreased. • Ammonia levels are elevated. • Serum creatinine level is possibly elevated. Excess Fluid Volume • Interventions: • Nutrition therapy consists of low sodium diet, limited fluid intake, vitamin supplements. • Drug therapy includes a diuretic like Lasix, electrolyte replacement. • Paracentesis is the insertion of a trocar catheter into the abdomen to remove and drain ascitic fluid from the peritoneal cavity. • Observe for possibility of impending shock. Comfort Measures • For dyspnea, elevate the head of the bed at least 30 degrees, or as high as the patient wishes to help minimize shortness of breath. • Patient is encouraged to sit in a chair. • Weigh patient in standing position, because supine position can aggravate dyspnea. Fluid and Electrolyte Management • Interventions: • Fluid and electrolyte imbalances are common as a result of the disease or treatment; test for: • Blood urea nitrogen level • Serum protein level, if low may order albumin (protein) • Hematocrit level • Electrolytes Surgical Interventions • Peritoneovenous shunt & Portocaval shunt are rarely done today because of serious complications. They are shunts that divert fluid away from the diseased liver into the venous system. • Transjugular intrahepatic portosystemic shunt is a nonsurgical procedure done in interventional radiology. Thread a balloon through the jugular to the liver into the portal vein. Enlarge it with a balloon and insert a stent to keep it open Potential for Hemorrhage • Interventions include: • Identifying the source of bleeding and initiating measures to halt it • Massive esophageal bleeding • Esophageal varices Potential for Hemorrhage (Cont’d) • Nonsurgical management includes: • Drug therapy—possibly nonselective beta blocker • Gastric intubation • Esophagogastric balloon tamponade: catheter surround3d by a balloon used in the esophagus to arrest bleeding from varices. 3 lumens, one for fluids, one balloon, control of the balloon Esophageal Gastric Tamponade Management of Hemorrhage • • • • • • Blood transfusions Esophagogastric balloon tamponade Vasoactive therapy Endoscopic procedures Transjugular intrahepatic portal-systemic shunt Surgical management Potential for Portal-Systemic Encephalopathy • Interventions include: • Role of ammonia: it is converted into urea in the liver and along with CO2 it becomes the final product of protein metabolism • Reduction of ammonia levels High levels indicate Liver Failure • Nutrition therapy using simple and brief guidelines • Drug therapy: • Lactulose: Empty the bowel of ammonia • Neomycin sulfate • Metronidazole Hepatitis • Widespread viral inflammation of liver cells can lead to Hepatic Encephalopathy (brain dysfunction due to high ammonia levels or orther liver problems. Can lead to a coma. • Hepatitis A • Hepatitis B • Hepatitis C • Hepatitis D • Hepatitis E Hepatitis A • Similar to that of a typical viral syndrome; often goes unrecognized • Spread via the fecal-oral route by oral ingestion of fecal contaminants • Contaminated water, shellfish from contaminated water, food contaminated by handlers infected with hepatitis A • Also spread by oral-anal sexual activity • Incubation period for hepatitis A is 15 to 50 days. • Disease is usually not life threatening. • Disease may be more severe in individuals older than 40 years. • Many people who have hepatitis A do not know it; symptoms are similar to a GI illness. Hepatitis B • Spread is via unprotected sexual intercourse with an infected partner, sharing needles, accidental needle sticks, blood transfusions, hemodialysis, maternal-fetal route. • Symptoms occur in 25 to 180 days after exposure; symptoms include anorexia, nausea and vomiting, fever, fatigue, right upper quadrant pain, dark urine, light stool, joint pain, and jaundice. • Hepatitis carriers can infect others, even if they are without symptoms. Hepatitis C • Spread is by sharing needles, blood, blood products, or organ transplants (before 1992), needle stick injury, tattoos, intranasal cocaine use. • Incubation period is 21 to 140 days. • Most individuals are asymptomatic; damage occurs over decades. • Hepatitis C is the leading indication for liver transplantation in the United States. Hepatitis D • Transmitted primarily by parenteral routes • Incubation period 14 to 56 days Hepatitis E • Present in endemic areas where waterborne epidemics occur and in travelers to those areas • Transmitted via fecal-oral route • Resembles hepatitis A • Incubation period 15 to 64 days Clinical Manifestations • • • • • • • • • • Abdominal pain Changes in skin or eye color (Jaundice) Arthralgia (joint pain) Myalgia (muscle pain) Diarrhea/constipation Fever Lethargy Malaise Nausea/vomiting Pruritus (itching) Nonsurgical Management • • • • Physical rest Psychological rest Diet therapy Drug therapy includes: • Antiemetics • Antiviral medications • Immunomodulators • AVOID DRUGS METABOLISED BY THE LIVER SUCH AS TYLENOL Fatty Liver (Steatohepatitis) • Fatty liver is caused by the accumulation of fats in and around the hepatic cells. • Causes include: • Diabetes mellitus • Obesity • Elevated lipid profile • Alcohol abuse • Many patients are asymptomatic. Hepatic Abscess • Liver invaded by bacteria or protozoa causing abscess • Pyrogenic liver abscess; amebic hepatic abscess • Treatment usually involves: • Drainage with ultrasound guidance • Antibiotic therapy Liver Trauma • The liver is one of the most common organs to be injured in patients with abdominal trauma. • Clinical manifestations include abdominal tenderness, distention, guarding, rigidity. • Treatment involves surgery, multiple blood products. Cancer of the Liver • One of the most common tumors in the world • Most common complaint—abdominal discomfort • Treatment includes: • Chemotherapy • Hepatic artery embolization • Hepatic arterial infusion (HAI) • Surgery Liver Transplantation • Used in the treatment of end-stage liver disease, primary malignant neoplasm of the liver • Donor livers obtained primarily from trauma victims who have not had liver damage • Donor liver transported to the surgery center in a cooled saline solution that preserves the organ for up to 8 hours Complications • • • • • • • • Acute, chronic graft rejection Infection Hemorrhage Hepatic artery thrombosis Fluid and electrolyte imbalances Pulmonary atelectasis Acute renal failure Psychological maladjustment •NCLEX TIME Question 1 These laboratory results are expected with which type of jaundice? Indirect serum bilirubin: Increased Direct serum bilirubin: Normal Stool urobilinogen: Increased Urine urobilinogen: Increased A. B. C. D. Intrahepatic Hemolytic Obstructive Hepatocellular Question 2 A possible outcome for the patient receiving a liver transplant because of hepatitis C–induced cirrhosis is that the newly transplanted liver may A. Be a likely site for cancer growth in the future B. Make the patient more likely to develop obstructive jaundice in the future C. Become re-infected with the hepatitis C virus D. Make the patient more susceptible to develop other forms of hepatitis Question 3 Which assessment parameter requires immediate intervention in a patient with severe ascites? A. B. C. D. Shallow respirations, rate 36 breaths/min Low-grade fever Confusion Tachycardia, rate 110 beats/min Question 4 A priority intervention in the management of a patient with decompensated cirrhosis would be: A. B. C. D. Limit protein intake. Monitor fluid intake and output. Manage nausea and vomiting Elevate head of bed >30 degrees Question 5 Which racial group is at the highest risk for developing liver cancer? A. B. C. D. Caucasian African American Asian Hispanic/Latino