Document
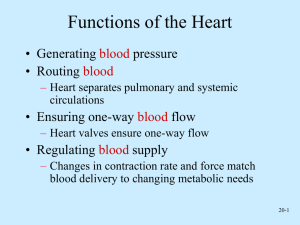
advertisement
I. It includes the heart and blood vessels. II. Heart structure and location A. Hollow, cone shaped muscle B. It lies slightly to the left side of the body and its base touches the diaphragm. C. The layered PERICARDIUM covers the heart. 1. The outer portion, FIBROUS PERICARDIUM, is a tough protective sac. It attaches to the center of the diaphragm. 2. The inner portion is a double layered membrane. a. The inner layer, VISCERAL PERICARDIUM, covers the heart. b. At the base of the heart the visceral pericardium turns back on itself to become the PARIETAL PERICARDIUM. 1. Between the visceral and parietal layers is a space, the PERICARDIAL CAVITY, that is filled with lubricating serous fluid. D. The wall of the heart is made of three layers. 1. The outer EPICARDIUM is a protective membrane. It has blood and lymph capillaries and nerve fibers. 2. The middle MYOCARDIUM is thick and made mostly of cardiac muscle. It functions to pump blood. 3. The inner ENDOCARDIUM lines all heart chambers and structures (like valves, etc.) E. Four heart chambers and valves 1. ATRIA (singular - atrium) two upper chambers that receive blood returning to the heart. a. Atria separated by INTERATRIAL SEPTUM. 2. VENTRICLES : two lower chambers that force blood into arteries leaving the heart. a. Ventricles separated by INTERVENTRICULAR septum. 3. An ATRIOVENTRICULAR orifice is a space that allows the atrium and ventricle to communicate. a. The right atrioventricular valve is called the TRICUSPID valve. It has three cusps that ensure that blood only moves from the atrium to the ventricle. b. The left atrioventricular valve is called the MITRIAL valve (or the BICUSPID). c. The PULMONARY valves are found at the base of the pulmonary arteries (take blood to lungs). They prevent blood from flowing back into the ventricles. 4. An AORTIC valve prevents blood from moving back into the ventricles from the aorta. a. The aortic and pulmonary valves are also called semilunar valves. III. Blood Vessels A. Arteries are strong, elastic vessels that are designed to carry blood away from the heart under high pressure. They branch into the smaller arterioles. 1. Three layered structure a. The inner layer is smooth surface so platelets and blood can flow through without being damaged. It also secretes chemicals that prevent clotting. b. The middle layer is elastic to accommodate changes in blood volume and strength to withstand the force of blood pressure. c. The outer layer is thin and attaches the artery to the surrounding tissues. 2. Artery walls are adapted for VASOCONSTRICTION and VASODILATION to control blood flow. B. Capillaries are the smallest blood vessels with thin semi-permeable walls(for gas exchange). They connect to small arterioles and veinules. 1. The openings in capillaries are slits of overlapping tissue. 2. Capillary networks are denser in areas with high metabolism, like muscle and nerve tissues. 3. Precapillary sphincters contract to cut off blood flow. They relax to restore flow when O2 and nutrients are low. C. Veinules emerge from capillaries and form veins that carry blood back to the heart. 1. Vein structure is similar to that of the arteries, except that the inner layers of vein walls are not as developed. 2. Veins have valves that keep blood flowing in one direction, back to the heart. IV. Path of blood flow A. The PULMONARY CIRCUIT consists of vessels that carry blood from the heart to the lungs, and back again. It functions to exchange CO2 and O2. Right Ventricle O2 poor blood Pulmonary trunk divides into right and left pulmonary artery In lung, artery leads to smaller arterioles, then capillaries. O2 gets picked up, then capillaries branch to larger veinules, then the pulmonary vein. O2 rich blood Pulmonary Veins Left Atrium V. Blood enters the SYSTEMIC CIRCUIT at the left ventricle. It leaves the heart through the aorta and travels to body tissues, then back to the heart to enter the pulmonary circuit. It’s function is to drop off oxygenated blood at the tissues and pick up CO2. Left Ventricle Aorta Arteries Tissues Veins Superior / Inferior Vena Cava VI. A cardiac cycle is a complete heartbeat A. Steps 1. Both Atria contract (atrial SYSTOLE) while both ventricles relax (ventricular DIASTOLE). 2. Both ventricles contract (ventricular systole) while both atria relax (atrial diastole). 3. The atria and ventricles both relax. B. The cardiac cycle depends on changes in pressure. 1. Early ventricular diastole: Pressure is lower than in the atria, causing the AV valves to open and ventricles to fill with about 70% of the blood. 2. Ventricular pressure increases. 3. The atria contracts and forces the remaining 30% of blood into the ventricles. 4. The ventricles contract, pressure rises and the AV valves close. 5. Pressure in the atria is now low, causing blood to flow into them from the veins. 6. Ventricular systole progresses and pressure is higher than it is in the aorta and pulmonary trunk. 7. Aortic and pulmonary valves open and eject blood into arteries. 8. Blood leaves the ventricles and pressure drops lower than it is in the aorta and pulmonary trunk. 9. Semilunar valves close. 10. When ventricular pressure is lower than atrial pressure, AV valves open and ventricles fill with blood. 11. For a moment, both the atria and ventricles are relaxed. 12. Ventricular systole begins again. VII.Heart sounds : Lubb-dupp A. Lubb occurs during ventriclular systole when the AV valves close. B. Dupp occurs during ventricular diastole when the pulmonary and aortic valves are closing. VIII. Cardiac conduction A. Electrical pulses in the heart are controlled by bundles of cells called nodes. B. The SINOATRIAL NODE (SA node) makes an electrical signal that causes the atria to contract. The SA node is also known as the pacemaker. C. The signal travels to the ATRIOVENTRICULAR NODE (AV node) and causes the ventricles to contract.