EAR DISCHARGE
advertisement

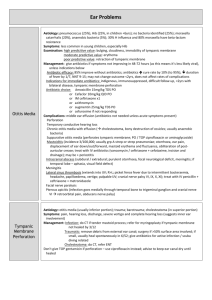
EAR DISCHARGE Calma.Capili.Coruña.Dagang. Datukon.Dayrit.De Castro.De La Llana Ear Discharge • Drainage of fluid, blood, cerumen, or pus from the ear • May be caused by a minor ear irritation or an infection • Also called OTORRHEA Types/Quality of Ear Discharge Color Viscosity Odor Serous (clear/watery) Bloody Purulent (yellow-brown) Thick Foul smelling Thin Odorless Associated Signs and Symptoms SIGNS and SYMPTOMS Ear pain or otalgia Ear swelling Ear pruritus Vertigo Tinnitus Hearing loss Differential Diagnoses • Is it acute or chronic? – Acute: < 6 weeks – Chronic: ≥ 6 weeks ACUTE EAR DISCHARGE Cause Suggestive Findings Acute otitis media with perforated TM Chronic otitis media Severe pain, with relief on appearance of purulent discharge Otorrhea in patients with chronic perforation, sometimes with cholesteatoma Can also manifest as chronic discharge Diagnostic Approach Clinical evaluation Clinical evaluation; sometimes high-resolution temporal bone CT Pathophysiology: Otitis Media • Obstruction of the eustachian tube appears to be the most important antecedent event associated with AOM • Physiologic functions of the eustachian are as follows: – Ventilation or pressure regulation of the middle ear – Protection of the middle ear from nasopharyngeal secretions and sound pressures – Clearance or drainage of middle ear secretions into the nasopharynx Otitis Media URTI Inflammation of the nasopharynx extending to the eustachian tube Stasis and inflammation within the eustachian tube Altered pressures within the middle ear (negative, related to ambient pressure) Acute inflammatory reaction: vasodilatation, exudation, leukocyte invasion, phagocytosis, and local immunological responses within the middle ear cleft ACUTE EAR DISCHARGE Cause Suggestive Findings Diagnostic Approach CSF leak from Significant, clinically obvious Cranial CT, head trauma head injury or recent surgery including skull base Fluid ranges from crystal clear to pure blood PostAfter tympanostomy tube Clinical tympanostomy placement evaluation tube May occur with water exposure ACUTE EAR DISCHARGE Cause Otitis externa (infectious or allergic) Suggestive Findings Infectious: Often after swimming, local trauma; marked pain, worse with ear traction Often a history of chronic ear dermatitis with itching and skin changes Allergic: Often after use of ear drops; more itching, erythema, less pain than infectious Typically involvement of earlobe, where drops trickled out of ear canal Both: Canal very edematous, inflamed, with debris; normal TM Diagnostic Approach Clinical evaluation CHRONIC EAR DISCHARGE Cause Suggestive Findings Diagnostic Approach Cancer of ear Discharge often bloody, mild Biopsy, CT scan, canal pain MRI in selected cases Sometimes visible lesion in canal Easy to confuse with otitis externa early on Cholesteatoma History of TM perforation CT scan, culture, MRI if Flaky debris in ear canal, intracranial pocket in TM filled with extension caseous debris, sometimes suspected polypoid mass CHRONIC EAR DISCHARGE Cause Suggestive Findings Diagnostic Approach Chronic Long history of ear infections Clinical purulent otitis or other ear disorders evaluation media Less pain than with external Usually culture otitis Canal macerated, granulation tissue, TM immobile, distorted, usually visible perforation CHRONIC EAR DISCHARGE Cause Suggestive Findings Foreign body Usually in children Drainage foul-smelling, purulent Foreign body often visible on examination unless marked edema or drainage Mastoiditis Fever, history of untreated or unresolved otitis media Redness, tenderness over mastoid Diagnostic Approach Clinical evaluation Clinical evaluation, culture, sometimes CT CHRONIC EAR DISCHARGE Cause Necrotizing otitis externa Suggestive Findings Usually history of immune deficiency or diabetes Chronic severe pain Periauricular swelling and tenderness, granulation tissue in ear canal Sometimes facial nerve paralysis Diagnostic Approach CT scan or MRI Culture CHRONIC EAR DISCHARGE Cause Wegener’s granulomatosis Suggestive Findings Often with respiratory tract symptoms, chronic rhinorrhea, arthralgias, and oral ulcers Diagnostic Approach Urinalysis Chest x-ray Antineutrophilic cytoplasmic antibody testing Biopsy Causes of Otorrhea Causes of Otorrhea Diagnostics Otitis Media • The diagnosis is made otoscopically revealing an opaque, thickened, erythematous and sometimes bulging tympanic membrane. • The tympanic membrane is immobile by pneumatic otoscopy Otitis Media with Effusion • Otoscopically, the tympanic membrane often appears opaque, thickened and occasionally retracted • Color may be pale, reddish, yellowish or bluish depending on the effusion • Tympanogram – A graphic record of tympanic membrane mobility will show a flat curve (type B) or occasionally a negative-pressure peak (type C) in mild and acute cases Chronic Suppurative Otitis Media • Otoscopic examination will reveal a central perforation in the tympanic membrane that does not involve the fibrocartilaginous ring – Often appreciated only in a dry ear – Valsalva maneuver may cause air bubbles to appear in the secretions • Smear , culture and sensitivity – Not routinely done except for severely resistant infections • Imaging studies – Not routinely done – May be useful for diagnosing mastoiditis Management Otitis Externa • Acidification of ear canal with drops – Reduced pH retards antibiotic growth – Acetic acid • +/- topical antibiotics – Treats bacterial infection and reduces edema – Polymyxin B, neomycin and hydrocortisone; ciprofloxacin; ofloxacin (bacterial growth) – Nystatin powder (fungal infections) Otitis Externa • EarSol HC, VoSoL HC, Acetasol HC – Treats superficial bacterial infections of the EAC • Neomycin, polymyxin B, and hydrocortisone – for steroid-responsive inflammatory condition for which a corticosteroid is indicated and where bacterial infection or a risk of bacterial infection exists. • Ciprofloxacin / Ofloxacin – Inhibits bacterial growth by inhibiting DNA gyrase • Nystatin powder – Fungicidal and fungistatic antibiotic Administer until 48 H after disappearance of symptoms. – 1-2 puffs from handheld nebulizer for 1 wk administered by treating physician Otitis Externa • Further Outpatient Care Suctioning of the external auditory canal on a weekly basis until debris has been removed. Topical eardrops are the mainstay of both inpatient and outpatient treatment. Oral antibiotics or antifungal agents are usually reserved for refractory cases. • Prevention Otitis externa can be prevented by avoiding use of cotton-tipped swabs or objects such as bobby pins to clean ears. Use of cotton-tipped swabs or bobby pins can cause excoriation of the canal skin that can lead to otitis externa. CSOM • Medical Treatment – aim is to eliminate infection and to control otorrhea – topical liquid agents used in the treatment of chronic middle ear disease include (combination of antibiotics, antifungals, antiseptics, solvents, and steroids) – The most commonly used topical antibiotics for CSOM include quinolones and aminoglycosides – Oral antibiotics should be prescribed to patients with severe infections & to those who are systemically ill CSOM • Medical treatment should be accompanied by aural toilet. • Principal aim of surgery for chronic suppurative otitis media – to clear out the disease – if possible, to reconstruct the patient's hearing • General indications for surgery are as follows: – Perforation that persists beyond 6 weeks – Otorrhea that persists for longer than 6 weeks despite antibiotic use – Cholesteatoma formation – Radiographic evidence of chronic mastoiditis, such as coalescent mastoiditis – Conductive hearing loss CSOM • Tympanoplasty – Goal: to eradicate disease from the middle ear and to reconstruct the hearing mechanism, with or without grafting of the tympanic membrane – 2 primary types: • lateral graft technique - the graft material is laid laterally to the annulus after the remnant of squamous tissue is denuded. • medial grafting - the annulus is raised and the graft slipped medially CSOM w/o Cholesteatoma • Myringoplasty - operation specifically designed to close tympanic membrane defects. • Tympanoplasty • Mastoidectomy – removal of the outer wall of the mastoid cortex and the exteriorization of all the mastoid air cells. This may be performed immediately in coalescent mastoiditis, in which case a drain may be left postoperatively. Canal wall-up mastoidectomy - removal of mastoid air cells while retaining the posterior canal wall. This is also the common approach for cochlear implantation. CSOM w/ Cholesteatoma • Mastoidectomy Modified radical mastoidectomy - the ossicles and the tympanic membrane remnants are preserved for possible hearing reconstruction Radical mastoidectomy - eradication of all disease from the middle ear and the mastoid and exteriorization of these structures into a single cavity; includes removing the entire tympanic membrane and the ossicles (except the stapes footplate) and closing the eustachian tube opening. AOM • Medical Management – Mostly viral in origin, especially those that accompany coryza. Most common: RSV, influenza viruses, adenovirus, and parainfluenza – Treatment is purely symptomatic and supportive – High doses of amoxicillin - result in middle ear fluid levels that exceed the minimum inhibitory concentration of all S pneumoniae AOM • Erythromycin – Has an antibacterial spectrum similar but not identical to that of penicillin; alternative for patients who are allergic to penicillin. • Penicillin G benzathine – Remains a useful antibiotic but is inactivated by bacterial beta-lactamases. Parenteral therapy with benzylpenicillin is used initially in severe infections, followed by 3-7 days of oral Penicillin V AOM • Gentamicin with hydrocortisone – Aminoglycosides although commonly used topical antibiotics, controversy surrounds topical therapy because of its potential for ototoxicity. Literature contains sporadic reports of sensorineural hearing loss associated w/ use • Ciprofloxacin – Quinolone derivatives have excellent antipseudomonal activity. Inhibits bacterial DNA synthesis & growth. Also available as ototopical preparations, w/ little demonstrable systemic effects. AOM • Medical Management – Pain control is essential to treatment, especially in the first 24 hours after diagnosis, since pediatric population is often undertreated for pain. In addition to ibuprofen and acetaminophen, topical benzocaine can also be given for pain control. Guidelines also include the use of narcotic analgesia with codeine for severe pain. AOM • Surgical Management – Myringotomy - an incision is made in the tympanic membrane to adequately drain the middle ear; reserved for AOM associated with severe otalgia or high fever in patients who have had a poor response to antibiotics. – Recurrent AOM in children may be due to chronic sinus infections, nasopharyngeal obstruction, or cleft palate. Surgically treating these conditions may decrease the number of ear infections. Foreign Body • Irrigation - simplest method, provided the tympanic membrane is not perforated. Irrigation w/ water is contraindicated for soft objects, organic matter, or seeds, w/c may swell • Suction - sometimes a useful. Suction the ear with a small catheter held in contact with the object. Grasp the object with alligator forceps. Place a right-angled hook behind the object and pull it out. Form a hook with a 25-gauge needle to snag and remove a large, soft object such as an eraser. • Avoid any interventions that push the object in deeper. Foreign Body • Cyanoacrylate adhesives (eg, Superglue) may be removed manually within 24-48 hours once desquamation occurs. If adhesive touches the tympanic membrane, remove it carefully and reevaluate • Remove batteries immediately to prevent corrosion or burns. Do not crush battery during removal Cancer of the Ear Canal • Medical Management – Primary radiation is ineffective for curative treatment – For cases in which contraindications to surgery are serious deterrents to surgery, palliative radiation and chemotherapy may be offered – Most authors advocate full course postoperative radiation to stage T3 or T4 tumors as defined by the University of Pittsburgh staging system – Literature supports a beneficial effect of postoperative radiation on survival. The temporal bone and neck should be treated with 50-60 Gy for tumors staged T3 and T4. Radiation may also be indicated for smaller lesions. Cancer of the Ear Canal • Surgical – all patients who are medically able should undergo surgical treatment – optimal surgery removes all of the cancer en bloc because positive margins are associated with poor survival rates – The resection procedures that can be performed for the temporal bone include: modified lateral temporal bone resection lateral temporal bone resection subtotal temporal bone resection total temporal bone resection. Cancer of the Ear Canal • Surgical – Adjunctive surgical procedures - neck dissection, parotidectomy, and craniotomy, should be performed when indicated – Advanced tumors with intracranial invasion - palliation with less extensive (and less morbid) surgical procedures. Wegener’s Granulomatosis • Manage the primary condition – Immunosuppression – IVIG – Plasmapheresis • wTucci, D. Otorrhea in http://ww.merck.com/mmpe/sec08/ch084/ch 084c.html. January 2009. Accessed September 16, 2009. • Causes of Otorrhea in http://www.ncbi.nlm.nih.gov/bookshelf/br.fcg i?book=cm&part=A3683&rendertype=table&i d=A3692. 1990. Accessed September 16, 2009.