Hormones - Cloudfront.net
advertisement

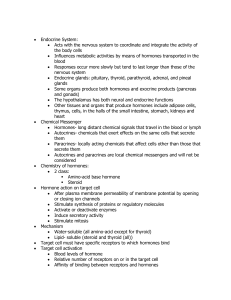
THE ENDOCRINE SYSTEM ENDOCRINE ORGANS AN OVERVIEW • Endocrine glands are ductless glands that produce and release hormones to the surrounding tissue, and they typically have a rich vascular (blood) and lymphatic (lymph) drainage that receives their hormones • Endocrine glands may be strictly endocrine, such as the pituitary, thyroid, parathyroid, adrenal, pineal and thymus; or they may be organs that have hormone production as one of many functions, such as the pancreas (exocrine) , gonads (exocrine), hypothalamus (neural), and others – Adipose cells: leptin – Cells of small intestine, stomach, kidneys, and heart AN OVERVIEW • Hormones: long-distance chemical signals that travel in blood or lymph throughout the body – Local hormones: • Autocrines: – Chemicals that exert their effects on the same cells that secrete them » Example: prostaglandins released by smooth muscle cells cause the smooth muscle cells to contract • Paracrines: – Also act locally but affect cell types other than those releasing the paracrine chemicals » Somatostatin released by one type of pancreatic cells inhibits the release of insulin by a different type of pancreatic cells • Study of hormones and the endocrine organs is called endocrinology HOMEOSTATIC IMBALANCE • Certain tumor cells, such as those of some cancers of the lungs or pancreas, synthesize hormones identical to those made in normal endocrine glands – However, they do so in an excessive and uncontrolled fashion HORMONES • Chemistry of Hormones: – Hormones are chemical messengers released into the blood to be transported throughout the body – Hormones are long-distance chemical signals that are secreted by the cells to the extracellular fluid and regulate the metabolic functions of other cells – Responses to hormones typically occur after a lag period of seconds or even days • Responses tend to be much more prolonged than those induced by the nervous system – Most hormones are amino acid bases, but gonadal and adrenocortical hormones are steroids, derived from cholesterol HORMONES • Hormones: – Amino acid based – Steroids – Eicosanoids: local hormones that are biologically active lipids released by nearly all cell membranes • Leukotrienes: signaling chemicals that mediate inflammation and some allergic reactions • Prostaglandins: have multiple targets and effects, ranging from raising blood pressure and increasing the expulsive uterine contractions of birth to enhancing blood clotting, pain, and inflammation HORMONES • Mechanisms of Hormone Action: – Even though all major hormones circulate to virtually all tissues, a given hormone influences the activity of only certain tissue cells, referred to as its target cells – Hormones bring about their characteristic effects on target cells by altering cell activity; that is, they increase or decrease the rates of normal cellular processes • Precise response depends on the target cell – Hormones typically produce: • Changes in membrane permeability or potential , or both, by opening or closing ion channels • Stimulate synthesis of proteins or regulatory molecules such as enzymes within the cell • Activate or deactivate enzymes • Induce secretory activity • Stimulate mitosis HORMONES • Mechanisms of Hormone Action: – Nearly all amino acid-based hormones exert their effects through an intracellular second messenger (G protein that is activated when a hormone binds to a membrane receptor) – Steroid hormones are lipid soluble and diffuse into the cell, where they bind to intracellular receptors, migrate to the nucleus, and activate specific target sequences of DNA • Involves direct gene activation by the hormone Amino Acid-Based Hormones and Second-messenger Systems • Because proteins and peptides cannot penetrate the plasma membranes of tissue cells, virtually all amino acidbased hormones exert their signaling effects through intracellular second messenger generated when a hormone binds to a receptor on the plasma membrane – Cyclic AMP is the best understood today Cyclic AMP Signaling Mechanism • Three plasma membrane components interact to determine intracellular levels of cyclic AMP (cAMP): – Hormone receptor – Signal transducer (G protein) – Effector enzyme (adenylate cyclase) Cyclic AMP Signaling Mechanism • 1. Hormone, acting as the first messenger, binds to its receptor: – Receptor changes shape and binds with a nearby inactive G protein • 2. G protein is activated – Guanosine diphosphate (GDP) bound to it is displaced by the high-energy compound guanosine triphosphate (GTP) – G protein behaves like a light switch • It is “off” when GDP is bound to it • It is “on” when GTP is bound to it Cyclic AMP Signaling Mechanism • 3. The activated G protein (moving along the membrane) binds to and activates the effector enzyme adenylate cyclase – At this point the GTP bound to the G protein is hydrolyzed to GDP and the G protein becomes inactive once again • 4. The activated adenylate cyclase generates the second-messenger cAMP from ATP Cyclic AMP Signaling Mechanism • 5. cAMP, which is free to diffuse throughout the cell, triggers a cascade of chemical reactions in which one or more enzymes (protein kinases) are activated – The protein kinases phosphorylate (add a phosphate group to) various proteins, many of which are other proteins – Because phosphorylation activates some of these proteins and inhibits others, a variety of reactions may occur in the same target cell at the same time Cyclic AMP Signaling Mechanism • This type of intracellular enzymatic cascade has a huge amplification effect. Each activated adenylate cyclase generates large numbers of cAMP molecules, and a single kinase enzyme can catalyze hundreds of reactions. Hence, as the reaction cascades through one enzyme intermediate after another, the number of product molecules increases dramatically at each step. Theoretically receptor binding of a single hormone molecule could generate millions of final product molecules Cyclic AMP Signaling Mechanism • The sequnce of reactions set into motion by cAMP depends on the: – Type of target cell (e.g thyroid, bone) – The specific protein kinases it contains – The hormone acting as first messenger (e.g. thyroid stimulating hormone, growth hormone) Cyclic AMP Signaling Mechanism • Notice that on the right side of this diagram that some G proteins inhibit rather than activate adenylate cyclase, thus reducing the cytoplasmic concentration of cAMP • Such opposing effects permit even slight changes in levels of antagonistic hormones to influence a target cell’s activity Cyclic AMP Signaling Mechanism • Because cAMP is rapidly degraded by the intracellular enzyme phosphodieterase, its action persists only briefly. This might seem a problem but because of the amplification effect, most hormones need to be present only briefly to cause the desired results. – Continued production of hormones then prompts continued cellular activity – No extracellular controls are necessary to stop the activity (self-limiting) Second-Messenger Mechanisms of Amino Acid-Based Hormones Second-Messenger Mechanisms of Amino Acid-Based Hormones • PIP-Calcium Signal Mechanism – Although cyclic AMP is the activating second messenger in some tissues for at least 10 amino acid-based hormones, some of the same hormones (.g., epinephrine) act through a different second-messenger system in other tissues – One such mechanism, called the PIPcalcium signal mechanism, intracellular calcium ions act as the final mediator PIP-Calcium Signal Mechanism • 1. Hormone docking on the receptor causes it to bind the nearby inactive G protein • 2. The protein is activated as GTP binds, displacing GDP • 3. The activated G protein then binds to and activates membrane-bound phospholipase (the effector enzyme) – The G protein then becomes inactive PIP-Calcium Signal Mechanism • 4. Phospholipase splits a plasma-membrane phospholipid called PIP2 (phosphatidyl inositol biphosphate) into diacylglycerol (DAG) and inositol triphosphate (IP3), and both these molecules act as second messangers • 5. DAG activates specific protein kinases, and IP3 triggers the release of Ca2+ from the endoplasmic reticulum and other intracellular storage sites PIP-Calcium Signal Mechanism • 6. The liberated Ca2+ takes on a second messenger role, either by directly altering the activity of specific enzymes and plasma membrane Ca2+ channels or by binding to the intracellular regulatory protein calmodulin – Once Ca2+ binds to calmodulin, enzymes are activated that amplify the cellular response Second-Messenger Mechanisms of Amino Acid-Based Hormones • Other hormones (not listed in the previous two diagrams) act on their target cells through different mechanisms – Some unknown – Insulin and other growth factors appear to work without second messengers • Insulin receptor is a tyrosine kinase enzyme that is activated by autophosphorylation (addition of phosphate to several of its own tyrosines) when insulin binds STEROID HORMONES and DIRECT GENE ACTIVATION • • • Being lipid soluble, steroid hormones (and, strangely, thyroid hormone, a small iodinated amine) can diffuse into their target cells Once inside, they bind to an intracellular receptor that is activated by the coupling The activated hormone-receptor complex then makes its way to the nuclear chromatin, where the hormone binds to a DNA associated receptor protein specific for it – Exception: thyroid hormone receptors are always bound to DNA even in the absence of thyroid hormone STEROID HORMONES and DIRECT GENE ACTIVATION • The interaction between DNA and hormonereceptor complex “turns on” a gene – Prompts transcription of DNA to produce a messenger RNA (mRNA) • mRNA is then translated on the cytoplasmic ribosomes, producing specific protein molecules (enzymes) Direct Gene Activation Mechanism of Steroid Hormones HORMONES • Target Cell Specificity – Cells must have specific membrane or intracellular receptors to which hormones can bind – Target cell response depends on three factors: • Blood levels of the hormone • Relative numbers of target cell receptors • Affinity (strength) of the receptor for the hormone – Target cells can change their sensitivity to a hormone by changing the number of receptors HORMONES • Target Cell Specificity – Up-regulation: phenomenon in which target cells form more receptors in response to rising blood levels of the specific hormones to which they respond – Down-regulation: phenomenon in which prolonged exposure to high hormone concentrations desensitizes the target cells, so that they respond less vigorously to hormonal stimulation • Involves loss of receptors • Prevents the target cells from overreacting to persistently high hormone levels HORMONES • Hormones influence the number and affinity not only of their own receptors but also of receptors that respond to other hormones – Example: • Progesterone induces a loss of estrogen receptors in the uterus, thus antagonizing estrogen’s actions • However, estrogen causes the same cells to produce more progesterone receptors, enhancing their ability to respond to progesterone HORMONES • Potent chemicals, and they exert profound effects on their target organs at very low concentrations • Circulate in the blood in two forms: – Free: most circulate unencumbered – Bound to a protein carrier • In general, lipid-soluble hormones (steroids and thyroid hormones) travel in the bloodstream attached to plasma proteins • The concentration of a hormone reflects its: – Rate of release – Rate of inactivation and removal from the body • Most are removed from the blood by the kidneys or liver, and their breakdown products are excreted from the body in urine or feces HALF-LIFE • Length of time a hormone remains in the blood • Duration of time a hormone remains in the blood – Usually brief • Fraction of a minute to 30 minutes • Shortest for water-soluble hormones ONSET • Time required for hormone effects to appear varies greatly • Some hormones provoke target organ responses almost immediately, while others, particularly the steroid hormones, require hours to days before their effects are seen • Some hormones are secreted in a relatively inactive form and must be activated in the target cells DURATION • Duration of hormone action varies from seconds to several hours, depending on the hormone • Because of these variations, hormonal blood levels must be precisely and individually controlled to meet the continuously changing needs of the body Interaction of Hormones at Target Cells • Understanding hormonal effects is a bit more complicated than you might expect because multiple hormones may act on the same target cells at the same time and in many cases the results of such an interaction is not predictable even when you know the effects of the individual hormones Interaction of Hormones at Target Cells Types of Hormone Interaction • Permissiveness occurs when one hormone cannot exert its full effect without another hormone being present – Example: Thyroid hormone is necessary for normal timely development of reproductive structure by reproductive hormones. Without thyroid hormone, reproductive system development is delayed • Synergism occurs when more than one hormone produces the same effects in a target cell, and their combined effects are amplified – Example: Glucagon (pancreas) and epinephrine (adrenal medulla) cause the liver to release glucose to the blood. When they act together, the amount of glucose released is about 150% of what is released when each hormone acts alone. • Antagonism occurs when one hormone opposes the action of another hormone – Example: Insulin, which lowers blood sugar levels, is antagonized by the action of glucagon, which acts to raise blood sugar levels – May compete for the same receptors – May act through different metabolic pathways – May cause down-regulation of the receptors for the antagonistic hormone HORMONES • Control of Hormone Release – Most hormone synthesis and release is regulated through negative feedback mechanisms • Endocrine gland stimuli may be: – Humoral – Neural – Hormonal Three Different Mechanisms of Endocrine Gland Stimuli HUMORAL STIMULI • • • Term humoral refers back to the ancient use of the term humor (viscous body fluids: blood, bile, etc.) Simplest of the endocrine control systems Endocrine glands that secrete their hormones in direct response to changing blood levels of certain ions and nutrients – These stimuli are called humoral stimuli to distinguish them from hormonal stimuli, which are also blood-borne chemicals – Examples: • Parathyroid: Ca2+ • Pancreas: glucose • Adrenal cortex: K, Cl-,HCO3- NEURAL STIMULI • In a few cases, nerve fibers stimulate hormone release – Example: • Sympathetic nervous system stimulation of the adrenal medulla to release catecholamines (norepinephrine and epinephrine) during periods of stress HORMONAL STIMULI • Many endocrine glands release their hormones in response to hormones produced by other endocrine organs, and the stimuli in these cases are called hormonal stimuli – Example: • Release of most anterior pituitary hormones is regulated by the releasing and inhibiting hormones produced by the hypothalamus • Many anterior pituitary hormones stimulate other endrocine glands to release their hormones • The hypothalamus-pituitarytarget endocrine organ feedback loop lies at the very core of endocrinology NEURAL SYSTEM MODULATION – Both “turn on” factors (humoral, neural, and hormonal stimuli) and “turn off” factors (feedback inhibition and others) may be modified by the nervous system • Endocrine system is NOT strictly like a thermostat • The endocrine system can make fine adjustments – Example: if someone in the house is cold, the thermostat will not adjust itself • The nervous system can, in certain cases, override normal endocrine controls as needed to maintain homeostasis – Allows hormone secretion to be modified by the nervous stimulation in response to changing body needs • Example: – The action of insulin and several other hormones normally keeps blood sugar levels in the range of 90-110 mg glucose per 100 ml of blood – Under stress, blood sugar levels rise because the hypothalamus and sympathetic nervous system centers are strongly activated ensuring that the body has sufficient fuel for vigorous activity ENDOCRINE ORGANS PITUITARY GLAND (HYPOPHYSIS) • Size an shape of a pea (pea on a stalk) – The stalk, funnelshaped infundibulum, connects the gland to the hypothalamus superiorly PITUITARY GLAND (HYPOPHYSIS) • Two major lobes (well-defined part of an organ separated by boundaries): – One is glandular tissue (anterior pituitary) – One is neural tissue (posterior pituitary) Pituitary-Hypothalamic Relationship • The contrasting histology of the two pituitary lobes reflects the dual origin of this organ – Posterior Lobe (neurohypophysis) actually is derive from a downgrowth of the hypothalamus and maintains its neural connection to the brain • Neurosecretory cells in the hypothalamus synthesize two neurohormones and transport them along their axons to the posterior pituitary storing them in capillary beds for distribution throughout the body – Anterior Lobe (glandular)(adenohypophysis) originates from a superior outpocketing of the oral mucosa and is formed from epithelial tissue • Releasing and inhibiting hormones (amino acid based) secreted by neurons in the ventral hypothalamus circulate to the adenohypophysis, where they regulate secretion of its hormones – No direct neural connection between the two, but there is vascular connection ANTERIOR PITUITARY • The Pituitary Gland (Hypophysis) – The pituitary gland is connected to the hypothalamus via a stalk, the infundibulum, and consists of two lobes: the anterior pituitary, or adenohypophysis, and the posterior pituitary, or neurohypophysis – Anterior Pituitary: There are six adenohypophyseal hormones (all protein) and one prohormone • Growth hormone (GH) stimulates body cells to increase in size and divide • Thyroid stimulating hormone (TSH) is a tropic hormone that stimulates normal development and secretion of the thyroid gland • Adrenocorticotropic hormone (ACTH) stimulates the adrenal cortex to release corticosteroid hormones • Follicle-stimulating hormone (FSH) stimulates gamete production • Leutinizing hormone (LH) promotes ovulation in females and production of gonadal hormones • Prolactin stimulates milk production in females, and may enhance testosterone in males • Pro-opiomelanocortin (POMC) is a prohormone that is the source of adrenocorticotropic hormone and two opiates (pain killing neurotransmitters)(enkephalin and beta endorphin which reduce our perception of pain under certain stressful conditions) – Enkephalin activity increases dramatically in pregnant women in labor – Endorphin release is enhanced when an athlete gets a so-called second wind and is probably responsible for the “runner’s high” ADENOHYPOPHYSEAL HORMONES • • • • When the adenohypophysis (anterior pituitary) receives an appropriate chemical stimulus from the hypothalamus, one or more of its hormone are released by certain cells. Although many different hormones pass from the hypothalamus to the anterior lobe, each target cell in the anterior lobe distinguishes the message directed to it and responds in kind—secreting the proper hormone in response to specific releasing hormones, and shutting off hormone release in response to specific inhibiting hormones The hypothalamic releasing hormones are far more important as regulatory factors because only very little hormone is stored by secretory cells of the anterior lobe 4 of the 6 are tropins (tropic hormones) which regulate the secretory action of other endocrine glands: – – – – • Thyroid-stimulating hormone Follicle-stimulating hormone Adrenocorticotropic hormone Luteinizing hormone All 6 hormones affect their target cells via a cyclic AMP second-messenger system GROWTH HORMONES (GH) • • • • • • • Produced by the somatotropic cells of the anterior lobe Stimulates most body cells to increase in size and divide Major targets are the bones and skeletal muscles Essentially an anabolic (tissue building) hormone Promotes protein synthesis Encourages the use of fats for fuel, thus conserving glucose Most growth-promoting effects of GH are mediated indirectly by insulin-like growth factors (IGFs)(somatomedins) – Family of growth-promoting proteins produced by the liver, skeletal muscle, bone, and other tissues • Stimulate uptake of amino acids from the blood and their incorporation into cellular proteins throughout the body • Stimulate uptake of sulfur into cartilage matrix GROWTH HORMONES (GH) • Mobilizes fats from fat depots for transport to cells, increasing blood levels of fatty acids • Decreases the rate of glucose uptake and metabolism: – Because these actions antagonize those of the pancreatic hormone insulin, they are referred to as anti-insulin actions • In the liver, it encourages glycogen breakdown and release of glucose to the blood – The elevation in blood sugar levels that occurs as a result of this glucose sparing is called the diabetogenic effect of GH, because it mimics the high blood sugar levels typical of diabetes mellitus GROWTH HORMONES (GH) • Secretion is regulated chiefly by two hypothalamic hormones with antagonistic effects – Growth hormone-releasing hormone (GHRH) stimulates GH release – Growth hormone-inhibiting hormone (GHIH), also called somatostatin, inhibits GH • GHIH release is (presumably) triggered by the feedback of GH and IGFs – Rising levels of GH also feed back to inhibit its own release GROWTH HORMONES (GH) • A number of secondary triggers also influence GH release • GH secretion has a daily cycle, with the highest levels occurring during evening sleep, but the total amount secreted daily peaks during adolescence and then declines with age GROWTH HORMONES HOMEOSTATIC IMBALANCE of GH • Hypersecretion: excessive amounts of GH secreted – Gigantism • Still-active epiphyseal (growth) plates are targeted – Acromegaly • After the epiphyseal (growth) plates close • Enlarged extremities – Overgrowth of bony areas still responsive to GH (hands, feet, and face) • Hyposecretion: low or no secretion of GH – In adults usually causes no problems – In children results in slowed long bone growth – Typically accompanied by other adenohypophyseal hormones • If thyroid-stimulating hormone and gonadotropins are lacking, the individual will be malproportioned and will fail to mature sexually • GH is produced commercial – Careful therapy can promote nearly normal somatic growthally by genetic engineering Thyroid-Stimulating Hormone (TSH) • • • Also called thyrotropin Tropic hormone that stimulates normal development and secretory activity of the thyroid gland TSH release from thyrotrope cells of the anterior pituitary is triggered by the hypothalamic peptide thyrotropin-releasing hormone (TRH) – Rising blood levels of thyroid hormones act on both the pituitary and the hypothalamus to inhibit TSH secretion – The hypothalamus, in response, releases GHIH, which reinforces the blockage of TSH release Adrenocorticotropic Hormone (ACTH) • • • • • Also called corticotropin Secreted by the corticotrope cells of the adenohypophysis Stimulates the adrenal cortex to release corticosteroid hormones, most importantly glucocorticoids that help the body to resist stressors (any stimulus that directly or indirectly causes the hypothalamus to initiate stress-reducing responses, such as the fight-or-flight response) Release elicited by hypothalamic corticotropin-releasing hormone (CRH) – Has a daily rhythm, with levels peaking in the morning, shortly after sunrise – Rising levels of glucocorticoids feed back and block secretion of CRH and consequently ACTH release Internal and external factors that alter the normal ACTH rhythm by triggering CRH release include fever, hypoglycemia, and stressors of all types Gonadotropins • • • Regulate the function of the gonads (ovaries and testes) Follicle-stimulating hormone (FSH) – In both sexes, stimulates gamete (egg and sperm) production Luteinizing Hormone (LH) – In both sexes, promotes production of gonadal hormones • Females: – LH works with FSH to cause maturation of an eggcontaining ovarian follicle – LH then independently triggers ovulation and promotes synthesis and release of ovarian hormones • Males: – LH stimulates the interstitial cells of the testes to produce the male hormone testosterone – Called interstitial cellstimulating hormone (ICSH) in males Gonadotropins • • • Virtually absent from the blood of prepubertal boys and girls During puberty, the gonadotrope cells of the adenohypophysis are activated and gonadotropin levels begin to rise, causing the gonads to mature In both sexes, gonadotropin release by the adenohypophysis is prompted by gonadotropin-releasing hormone (GnRH) produced by the hypothalamus – Gonadal hormones, produced in response to the gonadotropins, feedback to suppress FSH and LH release Prolactin (PRL) • Protein hormone structurally similar to GH • Produced by lactotropes • Stimulates the gonads of animals other than humans: – In humans, stimulates milk production in breast – In males, some evidence indicates that PRL enhances testosterone production • Release is controlled by the hypothalamic releasing and inhibiting hormones Prolactin (PRL) • Prolactin-releasing hormone (PRH) causes prolactin synthesis and release, whereas prolactin-inhibiting hormone (PIH), now known to be the neurotransmitter dopamine (DA), prevents prolactin secretion – In males, the influence of PIH predominates – In females, prolactin levels rise and fall in rhythm with estrogen blood levels • Low estrogen levels stimulate PIH release • High estrogen levels promote release of PRH and, thus prolactin: – A brief rise in prolactin levels just before the menstrual period partially accounts for the breast swelling and tenderness some women experience: » But because the prolactin stimulation is so brief, the breasts do not produce milk » In pregnant women, prolactin blood levels rise dramatically toward the end of pregnancy, and milk production becomes possible » After birth, the infant’s suckling stimulates PRH release in the mother, encouraging continued milk production HOMEOSTATIC IMBALANCE • Hypersecretion of prolactin: Hyperprolactinemia – Most frequent abnormality of adenohypophyseal tumors – Inappropriate lactation – Lack of menses (menstruation) – Breast enlargement – Impotence in males • Hyposecretion: – Not a problem in anyone except women who choose to nurse PITUITARY POSTERIOR PITUITARY • Composed largely of nerve fibers and supporting cells – Largely the axons of hypothalamus neurons • Releases neurohormones (hormones secreted by neurons) received readymade from the hypothalamus – Thus, this area is a hormone-storage area and not a true endocrine gland POSTERIOR PITUITARY • • Two neurohormones are synthesized by the hypothalamus and secreted by the posterior pituitary Antidiuretic hormone (ADH) and oxytocin are each composed of 9 amino acids (almost identical) – Differ in only 2 amino acids, yet have dramatically different physiological effects – Oxytocin acts on the smooth muscle of the uterus and breast to cause uterine contractions during childbirth and milk let-down during nursing – Antidiuretic hormone (ADH) acts on kidney tubules to promote increased water reabsorption (water balance) – Both hormones use the PIPcalcium second-messenger mechanism OXYTOCIN • Strong stimulant of uterine contraction • Released in significantly higher amounts during childbirth and in nursing women • Stretching of the uterus and cervix as birth nears dispatches afferent impulses to the hypothalamus, which responds by synthesizing oxytocin and triggering its release from the neurohypophysis (posterior pituitary) – As blood levels rise, the expulsive contraction of labor gain momentum and finally end in birth OXYTOCIN • Positive feedback mechanism: – Acts as a hormonal trigger for milk ejection in women whose breast are producing milk in response to prolactin – Suckling causes a reflex-initiated release of oxytocin, which targets specialized myoepithelial cells surrounding the milk-producing glands. As these cells contract, milk is forced from the breast into the infant’s mouth • Natural and synthetic oxytocin drugs used to induce labor OXYTOCIN • Until recently, oxytocin’s role in males and nonpregnant, nonlactating females was unknown, but new studies reveal that this potent peptide plays a role in sexual arousal and orgasm when the body is already primed for reproduction by sex hormones. • Then, it is responsible for the feeling of sexual satisfaction that results from that interaction • In nonsexual relationships, it is thought to promote nurturing and affectionate behavior, that is, it acts as a “cuddle hormone” PITUITARY GLAND ANTIDIURETIC HORMONE (ADH) • Prevents wide swings in water balance, helping the body avoid dehydration and water overload • Diuresis is urine production: – An antidiuretic is a substance that inhibits or prevents urine formation • Hypothalamic neurons, called osmoreceptors, continually monitor the solute concentration (and thus the water concentration) of the blood – When solutes threaten to become too concentrated (as might follow excessive perspiration or inadequate fluid intake), the osmoreceptors transmit excitatory impulses to the hypothalamus neurons, which synthesize and release ADH • Liberated into the blood by the neurohypophysis, ADH targets the kidney tubules • Tubule cells respond by reabsorbing more water from the forming urine and returning it to the bloodstream • Less urine is produced and blood volume increases – As the solute concentration of the blood declines, the osmoreceptors stop depolarization, effectively ending ADH release ANTIDIURETIC HORMONE (ADH) • Other stimuli triggering ADH release: – Pain – Low blood pressure – Nicotine – Morphine – Barbiturates • Other stimuli inhibiting ADH – Alcohol – Excess water HOMEOSTATIC IMBALANCE • ADH deficiency: – Diabetes insipidus • Production of large amounts of urine and intense thrist • Diabetes (overflow) / insipidus (tasteless) • Diabetes (overflow) / mellitus (honey) – Blood sugar lost in urine THYROID • Butterfly-shaped • Located in the anterior neck, on the trachea just inferior to the larynx • Its two lobes are connected by a median tissue mass called the isthmus • Largest pure endocrine gland in the body • Its prodigious (enormous) blood supply makes thyroid surgery a painstaking endeavor THYROID • • • • The thyroid gland consists of hollow spherical follicles The walls of each follicle contain large epithelial cells called follicle cells that produce the glycoprotein thyroglobulin The central cavity (lumen) of the follicle stores colloid sticky material consisting of thyroglobulin molecules with attached iodine atoms – Thyroid hormone is derived from this iodinated thyroglobulin The parafollicular cells – Lie in the follicular epithelium but protrude into the soft connective tissue that separates and surrounds the thyroid follicles – Produce calcitonin hormone THYROID HORMONE TH • Body’s major metabolic hormone • Thyroid hormone consists of two amine hormones: – They act on all body cells to increase basal metabolic rate and body heat production – Both are constructed from two linked tyrosine amino acids – The principal difference is that T4 has four bound iodine atoms, and T3 has three • Thyroxine (T4) – Major hormone secreted by the thyroid follicles • Triiodothyronine (T3) – Most id formed at the target tissue by conversion of T4 to T3 THYROID HORMONE TH • Except for the adult brain, spleen, testes, uterus, and the thyroid gland itself, TH affects virtually every cell in the body • By stimulating enzymes concerned with glucose oxidation, it increases basal metabolic rate and body heat production – Calorigenic effect THYROID HORMONE TH • Because TH provokes an increase in the number of adrenergic receptors (alpha/beta receptors that respond to NE or epinephrine) in blood vessels, it plays an important role in maintaining blood pressure • It is an important regulator of tissue growth and development • It is critical for normal skeletal and nervous system development, maturation, and for reproductive capabilities Synthesis of Thyroid Hormone • Begins when TSH (thyroid stimulating hormone) secreted by the anterior pituitary binds to follicle cell receptors Synthesis of Thyroid Hormone • 1.Formation and storage of thyroglobulin: – After being synthesized on the ribosomes, thyroglobulin is transported to the Golgi apparatus, where sugar residues are attached and the molecules are packed into vesicles – These transport vesicles move to the apex of the follicle cell, where their contents are discharged into the follicle lumen and become part of the stored colloid Synthesis of Thyroid Hormone • 2. Iodide trapping and oxidation to iodine – To produce the functional iodinated hormones, the following cells must accumulate iodides (anions of iodine I-) from the blood – Because the intracellular concentration of I- is over 30 times higher than that in blood, iodide trapping depends on active transport – Once they enter the follicle cell, iodides are oxidized (loss electrons) and converted to iodine I2 Synthesis of Thyroid Hormone • 3. Iodination: – Once formed, iodine is attached to tyrosine amino acids that form part of the thyroglobulin colloid – This iodination reaction occurs at the apical follicle cellcolloid junction and is mediated by peroxidase enzymes Synthesis of Thyroid Hormone • 4. Coupling of T2 and T1: – Attachment of one iodine to a tyrosine produces monoiodotyrosine (MIT or T1) – Attachment of two iodines produces diiodotyrosine (DIT or T2) – Then, enzymes in the colloid link T1 and T2 together – Two linked DITs result in T4 – Linking MIT and DIT produces T3 – At this point, the hormones are still part of the thyroglobulin colloid Synthesis of Thyroid Hormone • 5. Colloid endocytosis: – Hormone secretion requires that the follicle cells reclaim iodinated thyroglobulin by endocytosis and combine the vesicles with lysosomes • 6.Cleavage of the hormone for release: – In the lysosomes, the hormones are cleaved out of the colloid by lysosomal enzymes – The hormones then diffuse from the follicle cells into the bloodstream – The main hormonal product secreted is T4 – Some T4 is converted to T3 before secretion, but most T3 is generated in the peripheral tissues THYROID HORMONES Synthesis of Thyroid Hormone • The initial response to TSH binding is secretion of thyroid hormone • Then more colloid is synthesized to “restock” the follicle lumen • As a general rule, TSH levels are lower during the day, peak just before sleep, and remain high during the night Thyroid Hormone Transport and Regulation • Most released T4 and T3 immediately bind to transport proteins, most importantly thyroxine-binding globulins (TBGs) produced by the liver • Both T4 and T3 bind to target tissue receptors, but T3 binds much more avidly and is about 10X more active – Most peripheral tissues have the enzymes needed to convert T4 to T3,, a process that entails enzymatic removal of one iodine group • T3 seems to enter a target cell and binds to intracellular receptors within the cell’s nucleus and initiates transcription of mRNA • Falling T4 blood levels trigger release of thyroid-stimulating hormone (TSH), and ultimately of more T4 • Rising T4 levels feed back to inhibit the hypothalamicadenhypophyseal axis, temporarily shutting off the stimulus for TSH release – At times of stress (pregnancy, prolonged cold), the hypothalamus can secrete thyrotropin-releasing hormone (TRH), which triggers TSH release overcoming the negative feedback controls HOMEOSTATIC IMBALANCE • Hypothyroid disorders: a (left) – Myxedema: mucous swelling • Low metabolic rate • Chilled • Constipation • Thick, dry skin puffy eyes • Lethargy • If due to lack of iodine a goiter develops (a) – Follicle cells produce colloid but cannot iodinate it HOMEOSTATIC IMBALANCE • Hypothyroid disorders: – Cretinism: severe hypothyroidism in infants • Mentally retarded • Short, disproportionately size body and a thick tongue and neck • Preventable if diagnosed early with iodine or hormone supplements but once damage is done it is irreversible HOMEOSTATIC IMBALANCE • Graves’ disease: b (right) – – – – – – Most common Serum often contains abnormal antibodies that mimic TSH and continuously stimulate TH release Believed to be an auto-immune disease Elevated metabolic rate; sweating; rapid, irregular heartbeat; weight loss despite adequate food intake Exophthalmos , protrusion of the eyeballs, may occur Treatment: surgical removal of the thyroid gland or ingestion of radioactive iodine (131I), which selectively destroys the most active thyroid cells THYROID GLAND • Calcitonin: – Polypeptide hormone produced by the parafollicular, or C, cells of the thyroid gland – Targets the skeleton – Lowers blood calcium by inhibiting osteoclast (cells that reabsorb or break down bone matrix) activity (hence bone resorption), and stimulates Ca2+ uptake and incorporation into the bone matrix • Bone-sparing effect – Excessive blood levels of Ca2+ act as a humoral stimulus for calcitonin release, whereas declining blood Ca2+ levels inhibit calcitonin cell secretory activity • Calcitonin regulation of blood Ca2+ levels is short-lived but extremely rapid – Direct antagonist of parathyroid hormone, produced by the parathyroid glands – Appears to be important only in childhood, when the skeleton grows quickly • In adults, a weak hypocalcemic ( low blood calcium) agent THYROID GLAND PARATHYROID GLAND • In the posterior region of the thyroid gland • Usually 4 of these glands, but can vary – As many as 8 have been observed, and some may be located in other regions of the neck • Two major types of cells: – Oxyphil cells: • Function unclear – Chief cells: • Secrete parathyroid hormone (PTH) , or parathormone PARATHYROID GLAND • Discovered by accident due to the deaths of people whose thyroid gland was removed PARATHYROID GLAND PTH • • • • • Parathyroid hormone (parathormone) Protein hormone Single most important hormone controlling the calcium balance of the blood Triggered by falling blood Ca2+ levels and inhibited by hypercalcemia (excessive amounts of calcium in the blood) Increases Ca2+ levels in the blood by stimulating three target organs: – Skeleton (calcium salts in matrix) – Kidneys – intestine PTH RELEASE • 1. Stimulates osteoclasts (boneresorbing cells) to digest some of the bony matrix and release ionic calcium and phosphates to the blood PTH RELEASE • • 2. Enhances reabsorption of Ca2+ (and excretion of PO43-) by the kidneys 3. Increases absorption of Ca2+ by the intestinal mucosal cells – Calcium absorption by the intestine is enhanced indirectly by PTH’s effect on Vitamin D activation – Vitamin D is required for absorption of Ca2+ from ingested food, but the form in which it is ingested or produced by the skin is relatively inactive – It must be converted by the kidneys to its active vitamin D3 form, calcitriol (1,25dihydroxycholecalciferol), a transformation stimulated by PTH CALCIUM ION HOMEOSTASIS • Essential for so many functions, including transmission of nerve impulses, muscle contraction, and blood clotting, precise control of Ca2+ levels is critical PARATHYROID HORMONES EFFECTS HOMEOSTATIC IMBALANCE • Hyperparathyroidism: – Rare and usually result of tumor – Calcium is leached from the bones, and the bones soften and deform as their mineral salts are replaced by fibrous connective tissue – Osteitis cystica fibrosa: – Bones tend to fracture spontaneously – Hypercalcemia: abnormally high blood Ca2+ levels • Depression of the nervous system leading to abnormal reflexes and weakness of the skeletal muscles • Formation of kidney stones as excess calcium salts precipitate in the kidney tubules • Calcium deposits may also form in soft tissues throughout the body and severely impair vital organ functions (metastatic calcification) HOMEOSTATIC IMBALANCE • Hypoparathyroidism: – PTH deficiency – Results from: • Trauma • Thyroid surgery • Deficiency of magnesium ( required for PTH secretion) – Hypocalcemia (low calcium) • Increases the excitability of neurons and accounts for the classic symptoms of tetany such as loss of sensation, muscle twitches, and convulsions • Untreated: respiratory paralysis and death ADRENAL (SUPRARENAL) GLANDS • • • The adrenal glands, or suprarenal glands, consist of two regions: – An inner adrenal medulla: • More like a knot of nervous tissue than a gland • Part of the sympathetic nervous system – An outer adrenal cortex: • Encapsulating the medullary region • Forms bulk of the gland • Glandular tissue derived from embryonic mesoderm Perched on top of the kidneys Each region produces its own set of hormones, but all help us to cope with stressful situations ADRENAL CORTEX • • Produces corticosteroids (well over 2 dozen steroid hormones) from three distinct regions: the zona glomerulosa, the zona fasciculata, and the zona reticularis synthesized from cholesterol – Pathway is multistep and involves varying intermediates depending on the hormone being formed Unlike the amino acid based hormones, steroid hormones are not stored in cells – Therefore, their rate of release in response to stimulation depends on their rate of synthesis ADRENAL CORTEX • Zona glomerulosa: mainly produces mineralocorticoids hormones – Hormones that help control the balance of minerals and water in the blood • Zona fasciculata: produces the metabolic hormones called glucocorticoids • Zona reticularis: – Abuts the adrenal medulla – Mainly produces small amounts of adrenal sex hormones (gonadocorticoids) MINERALOCORTICOIDS • Essential function is regulation of the electrolyte (mineral salt) concentrations in extracellular fluids, particularly of Na+ and K+ – The single most abundant cation in extracellular fluid is Na+, and although this ion is vital to homeostasis, excessive sodium intake and retention may promote high blood pressure (hypertension) in susceptible individuals MINERALOCORTICOIDS • Although there are several mineralocorticoids, aldosterone is the most potent and accounts for more than 95% of the mineralocorticoids produced – Maintaining sodium ion balance is aldosterone’s primary job • Performs this job by stimulating transcription of the Na+, K+-ATPase, the sodium pump that exchanges K+ for Na+ • Reduces excretion of Na+ from the body • Primary target is the distal parts of the kidney tubules, where it stimulates Na+ reabsorption from the forming urine and its return to the bloodstream • Also enhances Na+ reabsorption from perspiration, saliva, and gastric juice • Regulation of a number of other ions, including K+, H+, HCO3(bicarbonate), Cl- (chloride), is coupled to that of Na+; and where Na+ goes, water follows—an event that leads to changes in blood volume and blood pressure – Hence, Na+ regulation is crucial to overall body homeostasis MINERALOCORTICOIDS • Aldosterone is also secreted by cardiovascular organs, where it is a paracrine (secretion of a hormone from a source other than an endocrine gland) and plays a completely different role in cardiac regulation ALDOSTERONE • Secretion is stimulated by rising blood levels of K+, low blood levels of Na+, and decreasing blood volume and blood pressure – Rising blood levels of Na+ and lowering blood levels of K+ inhibit aldosterone secretion Mechanisms Regulating Aldosterone Secretion • 1. Renin-angiotensin mechanism – Major regulator – Influences both the electrolytewater balance of the blood and blood pressure – Special cells of the juxtaglomerular apparatus in the kidneys become excited when blood pressure (or low volume) declines or plasma osmolarity (solute concentration) drops • These cells respond by releasing renin into the blood which initiates an enzymatic cascade leading to the formation of angiotensin II, a potent stimulator of aldosterone release by the glomerulosa – Effects are ultimately involved in raising blood pressure Mechanisms Regulating Aldosterone Secretion • 2. Plasma concentration of sodium and potassium ions: – Fluctuating blood concentrations of sodium and potassium ions directly influence the zona glomerulosa cells – Increased K+ and decreased Na+ are stimulatory – Decreased K+ and increased Na+ are inhibitory Mechanisms Regulating Aldosterone Secretion • 3.ACTH – Under normal circumstances, ACTH (adrenocorticotropic hormone) released by the anterior pituitary has little or no effect on aldosterone release – However, when a person is severely stressed, the hypothalamus secretes more corticotropin-releasing hormone (CRH), and the rise in ACTH blood levels that follows steps up the rate of aldosterone secretion to a small extent – The increase in blood volume and blood pressure that results helps ensure adequate delivery of nutrients and respiratory gases during the stressful period Mechanisms Regulating Aldosterone Secretion • 4. Atrial natriuretic peptide (ANP) – Hormone secreted by the heart when blood pressure rises – Fine tunes blood pressure and sodium-water balance of the body – Major effect is to inhibit the reninangiotensin mechanism • Blocks renin and aldosterone secretion and inhibits other angiotensin-induced mechanisms that enhance water and Na+ reabsorption • Decreases blood pressure by allowing Na+ (and water) to flow out of the body in urine (natriuretic=producing salty water) HOMEOSTATIC IMBALANCE • Aldosteronism: – Hypersecretion of aldosterone – Results from adrenal neoplasms (abnormal formation of tissue) – Hypertension and edema (excessive amount of fluid) due to excessive Na+ and water retention – Accelerated excretion of potassium ions • If extreme, neurons become nonresponsive and muscle weakness (eventually paralysis) occurs • Addison’s disease: – Hyposecretory disease of the adrenal cortex – Involves a deficient output of both mineralocorticoids and glucocorticoids Adrenal Cortex Zona Fasciculata • Glucocorticoids: – Essential to life – Influences the energy metabolism of most body cells – Helps to resist stressors – Keeps blood sugar level constant – Maintains blood volume by preventing the shift of water into body tissue cells – Hemorrhage, infections, physical or emotional trauma evokes a dramatically higher output Adrenal Cortex Glucocorticoids • Types: steroid hormones – Cortisol (hydrocortisone) – Cortisone – Corticosterone • • • Basic mechanism of activity on target cells is to modify gene activity Regulated by negative feedback Cortisol release is promoted by ACTH, triggered in turn by the hypothalamus releasing hormone CRH (corticotropin-releasing hormone) – Rising cortisol levels feed back to act on both the hypothalamus and the anterior pituitary, preventing CRH release and shutting off ACTH and cortisol secretion Adrenal Cortex Glucocorticoids • The normal cortisol rhythm is interrupted by acute stress of any variety as the sympathetic nervous system overrides the (usually) inhibitory effects of elevated cortisol levels and triggers CRH release • The resulting increase in ACTH blood levels causes an outpouring of cortisol from the adrenal cortex • Stress results in a dramatic rise in blood levels of glucose, fatty acids, and amino acids, all provoked by cortisol – – – – Provokes gluconeogenesis: formation of glucose from fats and proteins Encourages use of fats for energy Stored proteins are broken down for enzyme synthesis Enhances epinephrine’s vasoconstrictive effects raising blood pressure and circulatory efficiency helping ensure that nutrients are quickly distributed to cells Adrenal Cortex Glucocorticoids • Cortisol excess: – Depress cartilage and bone formation – Inhibit inflammation by stabilizing lysosomal membranes and preventing vasodilation – Depress the immune system – Promote changes in cardiovascular, neural, and gastrointestinal function • Drug use: – Used to control many chronic inflammatory disorders • Rheumatoid arthritis • Allergic responses – However: double-edged sword • Although they relieve some of the symptoms of these disorders, they also cause the undesirable effects of excessive levels of these hormones HOMEOSTATIC IMBALANCE • Cushing’s disease (syndrome): – Excess Glucocorticoid • Hyperglycemia (steroid diabetes): increased blood sugar – Dramatic losses in muscle and bone protein – Water and salt retention – Hypertension and edema – Redistribution of fat (note back of neck) – Because of enhanced antiinflammatory effects • Tendency to bruise • Poor wound healing • Infections may become severe before producing recognizable symptoms – Treatment: • Surgical removal of tumor • Discontinuation of drug HOMEOSTATIC IMBALANCE • Addison’s disease: – Hyposecretory disorder of adrenal cortex – Deficits in both glucocorticoids and mineralocoticoids – Lose weight – Plasma glucose and sodium levels drop – Potassium levels rise – Severe dehydration and hypotension Adrenal Cortex Gonadocorticoids • Sex hormones • Bulk secreted by adrenal cortex • Are mostly weak androgens (male sex hormones) – Androstenedione – Dehydropiandrosterone (DEHA) • Converted to the more potent male hormone, testosterone, in the tissue cells to estrogen (female sex hormones) in females • Adrenal cortex also makes small amounts of female hormones (estradiol and other estrogens) • Amounts are insignificant compared with the amounts made by the gonads during late puberty and adulthood • Contribute to the onset of puberty and appearance of axillary and pubic hair • Female: thought to be important in sex drive – May account for production of estrogen after menopause HOMEOSTATIC IMBALANCE Gonadocorticoids • Hypersecretion: – Androgenital syndrome: masculinization • In adult males: no major effect since testicular testosterone has already produced virilization • In prepubertal males and females, the results can be dramatic – Male: maturation of the reproductive organs and appearance of the secondary sex characteristics occur rapidly, and the sex drive emerges with a vengeance – Female: develop a beard and a masculine pattern of body hair distribution, and the clitoris grows to resemble a small penis ADRENAL MEDULLA • Part of the autonomic nervous system • The adrenal medulla contains chromaffin (modified ganglionic cells) cells that synthesize the catecholamines epinephrine and norepinephrine via a molecular sequence from tyrosine to dopamine to NE to epinephrine ADRENAL MEDULLA • When the body is activated to fight-or-flight status by some short-term stressor, the sympathetic nervous system is mobilized – Blood sugar levels rise – Blood vessels constrict – Heart beats faster raising the blood pressure – Blood is diverted from temporarily nonessential organs to the brain, heart, and skeletal muscles – Preganglionic sympathetic nerve endings signal for release of catecholamines, which reinforce and prolong the fight-or-flight response ADRENAL MEDULLA • Unequal amounts of the two hormones are stored and released (approximately 80 % is epinephrine and 20 % norepinephrine) • With a few exceptions, the two hormones exert the same effects – Norepinephrine: chiefly a vasoconstrictor with little effect on cardiac output except with beta receptors (increase heart rate) • Epinephrine is the more potent stimulator of the heart and metabolic activities • Norepinephrine has the greatest influence on peripheral vasoconstriction and blood pressure ADRENAL GLAND ADRENAL GLAND • Unlike the adrenocortical hormones, which promote long-lasting body responses to stressors, catecholamines cause fairly brief responses STRESS and THE ADRENAL GLAND HOMEOSTATIC IMBALANCE ADRENAL MEDULLA • Hyposecretion: – Because hormones of the adrenal medulla merely intensify activities set into motion by the sympathetic nervous system neurons, a deficiency of these hormones is not a problem – Adrenal catecholamines are not essential for life • Hypersectretion: – Produces symptoms of uncontrolled sympathetic nervous system activity • Hyperglycemia: increased blood sugar • Increased metabolic rate • Rapid heartbeat and palpitations (sensation of rapid or irregular beating of the heart) • Hypertension: high blood pressure • Intense nervousness • Sweating PANCREAS • Located partially behind the stomach in the abdomen • The pancreas is a mixed gland that contains both endocrine and exocrine gland cells • Exocrine function: produces an enzyme-rich juice that is ducted into the small intestine during food digestion PANCREAS • • • Endocrine function: pancreatic islets called the islets of Langerhans that produce pancreatic hormones Islets contain two types of hormone-producing cells: – Alpha cells produce glucagon – Beta cells produce insulin Some islet cells also synthesize other peptides in small amounts: – Somatostatin • Inhibits gastric mobility • Blocks exocrine and endocrine function of pancreas – Pancreatic polypeptide (PP) PANCREAS • The effects of glucagon and insulin are antagonistic: – Glucagon is hyperglycemic – Insulin is hypoglycemic GLUCAGON – A 29-amino acid polypeptide – Extremely potent hyperglycemic agent • One molecule can cause the release of 100 million molecules of glucose into the blood – Targets the liver where it promotes: • Breakdown of glycogen to glucose (glycogenolysis) • Synthesis of glucose from lactic acid and from noncarbohydrate molecules (gluconeogenesis) • Release of glucose to the blood by liver cells, which causes blood sugar to rise • A secondary effect is a fall in the amino acid concentration in the blood as the liver cells sequester these molecules to make new glucose molecules GLUCAGON • Secretion by the alpha cells is prompted by humoral stimuli, mainly falling blood sugar levels • Sympathetic nervous system stimulation and rising amino acid levels (after rich protein meal) are also stimulatory • Suppressed by rising blood sugar levels and somatostatin INSULIN • A small 51-amino acid protein consisting of two amino acid chains linked by disulfide (-S—S--) bonds • Synthesized as part of a larger polypeptide chain called proinsulin – Middle portion is excise by enzymes, releasing functional insulin • Occurs in the secretory vesicles just before insulin is released from the beta cells INSULIN • Main effect is to lower blood sugar levels by enhancing membrane transport of glucose into body cells – Especially muscle and fat cells – Does not accelerate glucose entry into liver, kidney, and brain tissue (cerebral cortex and hippocampus are well supplied with insulin receptors), all of which have easy access to blood glucose regardless of insulin levels • Also influences protein and fat metabolism INSULIN • Inhibits the breakdown of glycogen to glucose and the conversion of amino acids or fats to glucose – Counters any metabolic activity that would increase plasma levels of glucose INSULIN • After glucose enters a target cell, insulin binding triggers enzymatic activities that: – 1. Catalyze the oxidation of glucose for ATP production – 2. Join glucose molecules together to form glycogen – 3. Convert glucose to fat (particularly in adipose tissue) INSULIN • As a rule, energy needs are met first, followed by glycogen formation • Finally, if excess glucose is still available, it is converted to fat • Insulin also stimulates amino acid uptake and protein synthesis in muscle tissue • Insulin sweeps glucose out of the blood, causing it to be used for energy or converted to other forms (glycogen or fats), and it promotes protein synthesis and fat storage INSULIN • Pancreatic beta cells are stimulated to secrete insulin chiefly by: – Elevated blood sugar levels – Rising plasma levels of amino acids and fatty acids – Release of acetylcholine by parasympathetic nerve fibers – Hyperglycemic hormone (glucagon, epinephrine, growth hormone, thyroxine, glucocorticoids) called into as blood sugar levels drop indirectly stimulates insulin release by promoting glucose entry into the blood-stream PANCREAS PANCREAS INSULIN • As body cells take up sugar and other nutrients, and plasma levels of these substances drop, insulin secretion is suppressed • Somatostatin depresses insulin release INSULIN • Thus, blood sugar levels represent a balance of humoral and hormonal influences • Insulin and (indirectly) somatostatin are the hypoglycemic factors that counterbalance the many hyperglycemic hormones REGULATION OF BLOOD SUGAR LEVELS HOMEOSTATIC IMBALANCE PANCREAS • Diabetes mellitus (DM) – Results from either hyposecretion or hypoactivity of insulin – Hypoactivity: • Insulin is absent or deficient • Blood sugar levels remain high after a meal because glucose is unable to enter most tissue cells • Ordinarily , when blood sugar levels rise, hyperglycemic hormones are not released BUT: – When hyperglycemia becomes excessive, the person begins to feel nauseated, which precipitates the fight-or-flight response – This results, inappropriately, in all the reactions that normally occur in the hypoglycemic (fasting) state to make glucose available—that is, glycogenolysis (glycogen breakdown), lipolysis (breakdown of fat), and gluconeogenesis (synthesis of glucose from noncarbohydrate molecules) – Thus, the already high blood sugar levels soar even higher, and excesses of glucose begin to be lost from the body in the urine (glycosuria) HOMEOSTATIC IMBALANCE PANCREAS • Lipidemia (lipemia): – When sugars cannot be used as cellular fuel, more fats are mobilized, resulting in high fatty acid levels in the blood – In severe cases of diabetes mellitus, blood levels of fatty acids and their metabolites (collectively called ketones) rise dramatically • Ketones are organic acids (e.g.: acetone) – When they accumulate in the blood, the blood pH drops, resulting in ketoacidosis – Ketones show in the urine (ketonuria) – Life threatening – Nervous responds by initiating rapid deep breathing to blow off CO2 from the blood and increase blood pH – If untreated, disrupts heart activity and oxygen transport – Severe depression of the nervous system leads to coma and death HOMEOSTATIC IMBALANCE PANCREAS • Excessive glucose in the kidney filtrate acts as an osmotic diuretic, that is, it inhibits water reabsorption by the kidney tubules • Result: Three cardinal sins of diabetes mellitus – Polyuria: huge urine output that leads to decreased blood volume and dehydration • Serious electrolyte losses – Ketones are negatively charged and carry positive ions out with them (Na+, K+) – Because of the electrolyte imbalance, the person getsa abdominal pains and may vomit, and the stress reaction spirals even higher – Polydipsia: excessive thrist • Hypothalamic thirst stimulated by dehydration – Polyphagia: excessive hunger and food consumption • Final sign • Sign that the person is “starving in the land of plenty” – Although plenty of glucose is available, it cannot be used, and the body starts to utilize its fat and protein stores for energy metabolism HOMEOSTATIC IMBALANCE PANCREAS • • Excessive glucose in the kidney filtrate acts as an osmotic diuretic, that is, it inhibits water reabsorption by the kidney tubules Result: Three cardinal sins of diabetes mellitus – Polyuria: huge urine output that leads to decreased blood volume and dehydration • Serious electrolyte losses – Ketones are negatively charged and carry positive ions out with them (Na+, K+) – Because of the electrolyte imbalance, the person getsa abdominal pains and may vomit, and the stress reaction spirals even higher – Polydipsia: excessive thrist • Hypothalamic thirst stimulated by dehydration – Polyphagia: excessive hunger and food consumption • Final sign • Sign that the person is “starving in the land of plenty” – Although plenty of glucose is available, it cannot be used, and the body starts to utilize its fat and protein stores for energy metabolism SYMPTOMATIC RESULTS OF INSULIN DEFICIT (DIABETES MELLITUS) Diabetes Mellitus • Type I: – Insulin dependent – Asymptomatic period during which the beta cells are systemically destroyed by an autoimmune response – Genes have been localized on several chromosomes • Multigene autoimmune response – Some investigation has indicated that in certain circumstances a virus that mimics the beta cells invades the body • Immune system attacks both – Totally lack insulin – Long term vascular and neural problems – Insulin injections • Artificial pancreas with pump and glucose sensor inserted into a large vein near the heart – Two month supply of insulin – Computer programmed • Transplants (immunosuppression problem) • Today there might be insulin mist inhalers Diabetes Mellitus • Type II: – 90% of known diabetes mellitus – Non-insulin dependent – Grows increasing common with age – Hereditary predisposition • 30% carry a gene that predisposes them – Produce insulin but for some reason the insulin receptors are unresponsive • Membrane protein (PC-1) inhibits the insulin receptor tyrosine kinase Diabetes Mellitus TYPE II – Lifestyle factors • Overweight – Overproduce a hormonelike chemical called tumor necrosis factor-alpha » depresses synthesis of a translocation protein (glut4) which enables glucose to pass through insulin-primed plasma membranes » Cells cannot take up glucose in its (glut4) absence • Sedentary • Weight loss and exercise can lower the risk of type II diabetes, even for people at high risk – Ketoacidosis is not a major problem – Treatment: • Oral medication (orinase) can be taken – But if severe injection of insulin needed (produced by recombinant DNA) • Drugs to increase the sensitivity of receptors • Blood testing – – – – Lance Infrared beam Electric current ultrasound HOMEOSTATIC IMBALANCE • Hyperinsulinism: – Excessive insulin secretion – Results in hypoglycemia: low blood sugar levels • Triggers the release of hyperglycemic hormones, which cause anxiety, nervousness, tremors, and weakness • Insufficient glucose delivery to the brain causes disorientation, progressing to convulsions, unconsciousness, and even death – Cause: • Tumor • Overdose of insulin – Treated by ingesting some sugar GONADS GONADS • Produce steroid sex hormones, identical to those produced by adrenal cortical cells – The major distinction is the source and relative amounts produced GONADS • Female: paired ovaries are small, oval organs located in the abdominopelvic cavity – Produces: • Ova (eggs) • Hormones: – Estrogen (most important) » Maturation of the reproductive organs » Appearance of secondary sex characteristics at puberty » Acting with progesterone, promotes breast development » Initial cyclic changes in the uterine mucosa (menstrual cycle) preparatory to implantation of the blastocyst – Progesterone » Produced in the corpus luteum (endocrine structure that develops within a ruptured ovarian follicle) and placenta » Responsible for changes in the endometrium in the second half of the menstrual cycle preparatory to implantation of the blastocyst – Inhibin » Produced in the corpus luteum » Inhibits the secretion of gonadotropin-releasing hormone GONADS • Male: testes, located in an extra-abdominal skin pouch (scrotum) – Produces: • Sperm • Hormones: – Testosterone » Initiates the maturation of the male reproductive organs and the appearance of secondary sex characteristics during puberty » Responsible for the sex drive » Necessary for normal sperm production » Maintains the reproductive organs in their mature functional state in adult males – Inhibin » Inhibits the secretion of gonadotropin-releasing hormone HOMEOSTATIC IMBALANCE • Male: – Prostatic hyperplasia: • Inhibin levels high – Cancer of the prostate: • Inhibin levels low – Testes: in addition these conditions could be related to anterior pituitary problems • Hyperfunction (hypergonadism) – Early maturity such as large sexual organs with early functional activity and increased growth of hair • Hypofunction (hypogonadism) – – – – – – Indicated by undeveloped testes Absence of body hair High pitched voice Loss of sexual desire Low metabolism Eunuchoid (eunuch): retarded development of sex organs HOMEOSTATIC IMBALANCE • Female: in addition these conditions could be related to anterior pituitary problems • Hyperfunction (hypergonadism): – Early maturity such as large sexual organs with early functional activity • Hypofunction (hypogonadism): – – – – Indicated by undeveloped ovaries Loss of sexual desire Low metabolism Eunuchoid (eunuch): retarded development of sex organs PINEAL GLAND PINEAL GLAND • • • Tiny, pine cone-shaped gland Hangs from the roof of the third ventricle in the diencephalon of the brain Secretory cells called pinealocytes – Between these cells are dense particles containing calcium salts (brain sand or pineal sand) • These salts are radiopaque (impenetrable to X-rays or other forms of radiation) – Hence, the pineal gland is a handy landmark for determining brain orientation in X rays – Secrets melatonin, a hormone derived from serotonin • Concentrations in blood rise and fall in a diurnal cycle – Peak levels occur during the night and make us drowsy – Lowest levels occur around noon • Indirectly receives input from the visual pathways in order to determine the timing of day and night • In some animals, mating behavior and gonadal size vary with changes in the relative lengths of light and dark periods, and melatonin mediates these effects • In children, melatonin may have an antigonadotropic effect, that is, it may inhibit precocious (too early) sexual maturation and thus affect the timing of puberty PINEAL GLAND • Suprachiasmatic nucleus of the hypothalamus (biological clock) is richly supplied with melatonin receptors – Exposure to bright light (known to suppress melatonin secretion) can reset the clock timing – Hence, changing melatonin levels may also be a means by which the day/night cycles influence physiological processes that show rhythmic variations • Such as body temperature, sleep, and appetite THYMUS THYMUS • Located deep to the sternum in the thorax • Large and conspicuous in infants and children • Diminishes in size throughout adulthood – By old age, it is composed largely of adipose and fibrous connective tissue • Produces a family of peptide hormones: – thymopoietin, thymic factor, and thymosin, which are essential for the development of T lymphocytes and the immune response OTHER HORMONE-PRODUCING STRUCTURES • Heart: The atria of the heart contain specialized cardiac muscle cells that secrete atria natriuretic peptide – Signals the kidneys to increase their production of salty urine – Inhibits aldosterone release by the adrenal cortex – resulting in decreased blood volume, blood pressure, and blood sodium concentration OTHER HORMONE-PRODUCING STRUCTURES • Gastrointestinal tract: – Enteroendocrine cells are hormonesecreting cells sprinkled in the mucosa of the gastrointestinal (GI) tract • Secrete amine and peptide hormones to regulate digestive functions – Many of these hormones are chemically identical to neurotransmitters: » They act as paracrines (secretion of a hormone from a source other than an endocrine gland) OTHER HORMONE-PRODUCING STRUCTURES • Placenta: – Besides sustaining the fetus during pregnancy, the placenta secretes several steroid and protein hormones that influence the course of pregnancy • Estrogens, progesterone, and human chorionic gonadotropin, which act on the uterus to influence pregnancy • Kidneys: – The kidneys produce erythropoietin, which signals the bone marrow to produce red blood cells OTHER HORMONE-PRODUCING STRUCTURES • SKIN: – Produces cholecalciferol, an inactive form of vitamin D3, when modified cholesterol molecules in epidermal cells are exposed to ultraviolet radiation • This compound then enters the blood via the dermal capillaries, is modified in the liver, and becomes fully activated in the kidney. – The active form of vitamin D3, calcitriol, is an essential part of the carrier system that intestinal cells use to absorb Ca2+ from ingested food – Without this vitamin, the bones become weak and soft • Adipose tissue: – Produces leptin, following their uptake of glucose and lipids, which they store as fat • Binds to CNS neurons concerned with appetite control, producing a feeling of satiety – Produces resistin, an insulin antagonist DEVELOPMENTAL ASPECTS OF THE ENDOCRINE SYSTEM • Endocrine glands derived from mesoderm produce steroid hormones; those derived from ectoderm or endoderm produce amines, peptides, or protein hormones • Environmental pollutants have been demonstrated to have effects on sex hormones, thyroid hormone, and glucocorticoids • Old age may bring about changes in rate of hormone secretion, breakdown, excretion, and target cell sensitivity