Tricks to Diagnosis Elusive Rashes
advertisement

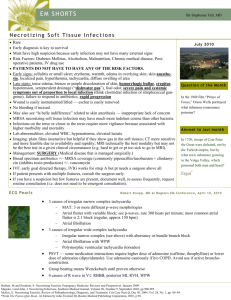
Practical Approach to Dermatology Richard P. Usatine, M.D. Director of Medical Student Education UTHSCSA Department of Family and Community Medicine Goals of lecture: • Demonstrate a practical approach to the diagnosis of skin conditions using pattern recognition • review dermatology patterns by: – viewing multiple images – distinguishing between common and uncommon patterns – observing local and regional morphology Primary Lesions • • • • Macule papule plaque nodule • • • • wheal (hive) pustule vesicle bulla TINEA VERSICOLOR DERMATOFIBROMA Secondary (Sequential) Lesions • • • • scale crusts erosion ulcer • • • • fissure atrophy excoriation lichenification Strategies for Diagnosis • • • • • Use magnification Feel lightly Palpate deeply Distribution Local patterns - groups, rings, lines Looking for clues beyond the rash • Look at nails, hair, mucus membranes, hands, feet – nail pitting for psoriasis – scalp may be clue to seborrhea elsewhere – lichen planus may show a white lacy pattern in the mouth – fungal infection on the feet with ID reaction on the hand Think Pathophysiology • Infections • Inflammatory Processes - dermatitis, seborrhea • Acne and related disorders • Immunologic • Benign and premalignant growths • Malignancies Infections • • • • bacterial viral fungal infestations Bacterial infections of skin • • • • • • Impetigo, cellulitis, abscess Folliculitis Furuncle, carbuncle, abscess Necrotizing fasciitis Erythrasma, pitted keratolysis Impetigo • superficial skin infection of the epidermis • characterized by translucent (“honey”) crusts • caused by S. aureus and strep. pyogenes (GABHS) • Cephalexin and Dicloxacillin • Bactroban topical Ecthyma and Bullous Impetigo • Two variations of impetigo • Ecthyma has a ulcerated “punched-out” base • Bullous impetigo is more often caused by S. aureus Erysipelas • • • • • • specific type of superficial cellulitis prominent lymphatic involvement. GABHS; H. flu in children face or leg admit if toxic or extensive involvement otherwise, oral Augmentin with close follow-up Flesh-Eating Bacteria • Necrotizing Fasciitis - Type 1 – Mixed anaerobes – Gram negative aerobic bacilli – Enterococci • Type 2 – Group A strep • Bisno, Stevens. Streptococcal Infections, NEJM, Jan 1996 Diagnosis of Necrotizing Fasciitis • diffuse swelling of arm or leg • follow by bullae with clear fluid which become violaceous in color • marked systemic symptoms • can lead to cutaneous gangrene, myonecrosis, and shock Cellulitis vs. Necrotizing Fasciitis • necrotizing fasciitis may look like cellulitis at first • cellulitis only requires antibiotics • necrotizing fasciitis requires surgical debridement along with antibiotics Viral • HPV • Herpes • Varicella/Zoster Burrow Infestations • scabies - Elimite • lice - Nix • Permethrin Fungal Infections • • • • • • Tinea pedis Tinea capitis Tinea corporis Tinea cruris Onychomycosis Tinea versicolor Granuloma annulare Common Types of Dermatitis (Inflammation) • • • • Hand Eczema Atopic Dermatitis Contact Dermatitis Seborrheic Dermatitis Cutaneous Anthrax MRI MRI Take home points • Learn the patterns • Look at nails, hair, mucus membranes, hands, feet for clues to diagnosis • Use understanding of patterns