Skin pathology, infectious, autoimmune diseases
advertisement

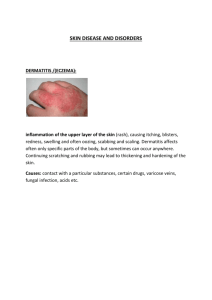
SKIN-II Dr.Ashraf Abdelfatah Deyab Assistant Professor NORMAL SKIN, with labels Lecture 37: Pathology of skin II • At the end of session student should be able to : • 1- enlist and describe etiology, morphology and clinical features of infectious dermatoses (bacterial, fungal and warts) • 2- Enlist blistering (Bullous) disorders • 3- Briefly discuss pathogenesis, morphology and clinical features of pemiphigus , Bullous pemiphigoid • Robbins and Cortan 8th edition (843-847) Blistering (Bullous) Diseases = Vesiculobullous or Blistering bullous diseases = Groups of disease chr. by “bullous” & “acantholysis” = Bullous : epidermal separation levels: A)Subepidermal bulla B) Intraepidermal bulla. = Intraepidermal type has two types: 1) Subcorneal) 2) Suprabasal - What is a bulla? What is acantholysis? - Bulla: Fluid-filled raised lesion greater than 5 mm across. Acantholysis: Loss of intercellular connections resulting in loss of cohesion between keratinocytes. BLISTERING DISEASES • Subcorneal • Suprabasal • Subepidermal Blister Formation BULLOUS DISEASES • Subepidermal bullous dermatoses: 1-Dermatitis herpetiformis. • 2- Bullous pemphigoid. • 3- Erythema multiforme. • 4- Porphyria cutanea tarda • 5- Epidermolysis bullosa, • • Intraepidermal bullous dermatoses: • 1- Pemphigus vulgaris • 2- Pemphigus vegetans Pemphigis Vulgaris Bullous pemiphigoid Pemphigus • Pemphigus is a “life threatining” blistering disorder caused by autoantibodies that result in the dissolution of intercellular attachments within the epidermis and mucosal epithelium. • Pemphigus vulgaris-most common type, including multiple variants. • Age: fourth to sixth decades of life,40-60 ]yrs • Sex: men and women are affected equally Pemphigus vulgaris- PV • Commonest Chronic autoimmune Bullous disease (Suprabasal acantholytic) Painful + rarely pruritic. • Site: mucosa, skin, scalp, face, axilla, groin, trunk, and points of pressure, oral ulcers • Etiopathogenesis: • Autoantibodies -IgG against epidermis& mucosa (adehesion desmogleins1&3)&linkage to specific HLA types (net-like pattern)>>Directly disrupting +Activate protease • Morphologic features: 1- Superficial vesicles\bullae, rupture easily>> leaving shallow erosions covered with dried serum and crusts. 2-superficial dermal infiltration by lymphocytes, histiocytes, and eosinophils • The mainstay of treatment • Immunosuppressive agents>> decrease the titers of the Abs Pemphigis Vulgaris- morphology Clinical : skin with varying sizes blisters in skin, Transudative fluid The surfaces are glistening, transparent thin roof. The blisters content is clear serum. Nikolsky’s sign) is positive*** According to the duration: rupture, crust, errosions Pemphigus, fresh bullae Pemphigus, ruptured, scabbed bullae Eroded plaques are formed on rupture of confluent, thin-roofed bullae, “suprabasal acantholytic blister” Acantholysis – stratum spinosum,- cells lysis adhesions- keratinocytes change to round suprabasal acantholytic blister” IF test of skin biopsy: Fish net pattern , indicate immunoglobulin (IgG) deposition BULLOUS PEMPHIGOID • Acute or chronic autoimmune skin disease, involving the formation of large blisters\bulla, age: in elderly • Sizes: up to 2 cm ,also may reach 4 to 8 cm • Clinically: tense large blister\bullae, filled with clear fluid, in normal or erythematous skin. Not rupture easily. • - If not secondarily infected, heal without scarring • - Can present as urticarial plaques &pruritus. • Site: skin (locally or generally), mucosa. Inner aspects of the thighs, flexor of the forearms, axillae, groin,&lower abdomen. • Microscopic: 1) Subepidermal, nonacantholytic bulla. 2) Superficial& deep perivascular infiltrate of lymphocytes and variable numbers of eosinophils, occ. Neutrophils. 3)Superficial dermal edema, with basal cell layer vacuolization Bullous Pemphigoid Pathogenesis • Pathogenesis: • 1) Deposition of Auto-antibodies Igs &complement in the basement membrane, featuring linear deposition “plaques” . • 2) Inflammatory mediated-tissue injury associated with recruited neutrophils and eosinophils. Bullous Pemphigoid • Older Pts • Multiple Bullae • (Nikolsky’s sign) is negative*** because there is no acantholysis. Bullous Pemphigoid • Sub-epidermal bulla with serum and degenerating eosinophils. Note bulla is non-acantholytic, Vcuolated dermis- mixed inflammatory cells Bullous Pemphigoid • Linear deposition of IgG & C3 in the basement membrane as seen in this IF image is typical of bullous pemphigoid. Dermatoses- Infections 1- Bacterial infection (impetigo) 2- Fungal infection(superficial- Tinea) 3- Viral infection (e.g. Warts) 4- Parasitic infection 5- Insects Factors affecting clinical presentation: Host immunity + infectious agents Viral dermatoses- WARTS - Warts: Most common skin viral infection, define as cutaneous or mucosal VERRUCAE = wart = papilloma-like squamous lesion, caused by HPV (DNA virus)= > 100 variants, precancerous - Etiology: several types of HPV, members papova. Age: common in children& adolescents or any age Transmission: direct contact (sexual),auto- inoculation. Clinical course: generally self-limited, regressing spontaneously within 6 months to 2 years. HPV lead to cancer (penis, cervix, vagina, anus, orophyrnx) Viral WARTS classification : - Classification: based on appearance and location Warts are classified: - 1-Verruca vulgaris: most common type of wart, anywhere, on hand, dorsal surfcae periungual - 2-Verruca plana,(flat wart), common on face or the dorsal surfaces of the hands - 3-Verruca plantaris - soles and palms, - 4- Verruca palmaris - soles and palms. - 5- Condyloma acuminatum (venereal wart) the penis, female genitalia, urethra, perianal areas, and rectum Viral WARTS-morphology Gross: color-(gray-white to tan), shape-(“VV” flat to convex, papules with a rough, pebble-like surface, “CA” cauliflower-like, scaly ), size- (varying 0.1- to 1-cm, up2cm) The histologic characteristics: 1) - Focal epidermal hyperplasia. 2) - Verrucous or papillomatous 3) - Hyperkeratosis and parakeratosis. 4) - Acanthosis varying degrees. 5) - Cells cytoplasmic vacuolization (koilocytosis) 6) = perinuclear hallo\zones. - EM- clear zone reveal numerous keratohyaline Verruca vulgaris- Cutaneous Warts • Common wart (verruca vulgaris): typically occur on hands, face anywhere as elevated, hard, rough, peeled off, leaving a pink . • Caused by infection with various strains of the human papillomavirus (HPV) Bacterial dermatoses- Impetigo - Impetigo - common superficial bacterial infection of skin. (strept. & staph) -- Age: more in children than adult -Sites: involves exposed skin, the face and hands. -Transmission - It is highly contagious and is frequently seen in children and in adults in poor health. - classification: classically Two forms exist, referred to as: 1) Impetigo contagiosa caused by group A β-hemolytic streptococci (non-bullous) 2) Impetigo bullosa; by Staphylococcus aureus (bullous) they differ from each other by the size of the pustules Now: both are usually caused by Staphylococcus aureus. Impetigo-clinical appearance 1) Non-bullous impetigo: 1) Erythematous small red sores rapidly evolve to >> breaks >> Shallow erosions with leaking pus or serum, featuring honey-colored crust. - - If the crust is not removed>> adjacent extensive epidermal damage . - 2) A bullous form of impetigo mainly occurs in - children< 2yrs, fluid-filled blisters > break,> form yellow scabs Complications: 1- Strept. impetigo is a major cause of post-strept. acute glomerular nephritis (AGN). 2- Develop skin scar if not treated Impetigo Bacterial Infection- Impetigo • Risk: factors as warm, humidity, crowded conditions, and poor hygiene increase the chance of spread rapidly among large groups. • Clinically: induces allergic and inflammatory eczematous response in the host • Morphology: • The characteristic microscopic feature of impetigo: • 1) In Blistering lesions- accumulation of fluid and neutrophils beneath the stratum corneum >> TO produce Subcorneal pustule. • • • • 2) Crusts- rupture pustules. 3) presence of bacteria 4) Nonspecific, reactive epidermal alterations. 4) Superficial dermal inflammation . SUPERFICIAL FUNGAL INFECTIONS- Dermatophytoses - -commonest superficial fungal skin infection (confined to the stratum corneum), in human, domestic animals. Ringworm is misnomer used to refer this infection. - The etiology: number of different species of fungi. Dermatophytes of the genera Trichophyton and Microsporum are - Transmission: - contact with infected soil animals and - Predisposing factors: - Excessive heat ,humidity, exposure to animals, soil. - Morphologic features- Tinea- has different clinical presentations& types depend on the infected sites of the body- annular, reddish, scaly - The fungal colonized in form of hyphae& arthospore are found in the stratum corneum and in hair shafts. Dermatophytoses disease patterns • Dermatophytosis = (tinea or ringworm) • Tinea Capitis (Scalp) • Tinea Barbae (facial hair) • Tinea Corporis (arm, leg, trunk) • Tinea Cruris (groin- Jock itch) • Tinea Pedis (Feet- Athlete’s foot) • Tinea unguium ( fingernails and toenails) • Tinea Manuum (hand and palm area) • Tinea Faciei (face fungus) laboratory diagnosis: Skin Scrapings,nail scrapings, hairs Direct Microscopy\ Culture\ Serology Fungal Infections - Dermatophytes • Scaly patches and plaques, often annular in configuration Tinea capitis (scalp dermatophytosis) • Age: usually in children, rarely in infants& adults. • Clinically: It is characterized by: • • • • 1) Asymptomatic, often hairless patches of skin . 2) Associated with mild erythema, 3) Crust formation, 4) Scaling. Ringworm of scalp, Tinea capitis Tinea barbae Tinea barbae is infection of the beard area that affects adult men; it is uncommon disorder Ringworm of the body, Tinea corporis common fungal infection of the body surface that affects all ages, but particularly children Tinea cruris, or jock itch Frequently in the inguinal areas of obese men during warm weather. Infected moist, red patches, scaling borders Athlete’s foot, or tinea pedis. Diffuse erythema and scaling, occasional bacterial superinfection Onychomycosis (Note the LACK of the word tinea) Dermatophytes primary infection or spread to the nails is referred to as onychomycosis Tinea - morphology Gross: Characteristic reddish plaque or ring worm, annular or lack of ring shaped Histologically: 1- Inflammation of dermal and subcutaneous tissue. intraepidermal neutrophils 2- Fungal colonies (viable arthrospores or hyphae) in the anucleate cornified layer of lesional skin, etc.. 3- Pseudoepitheliomatous hyperplasia. 4- Features of Bacterial superinfections+\- Cellulitis, abscesses. PAS stain of hyphae, probably scrap PAS stain of hyphae, histologic section

![Occupational Health - Zoonotic Disease Fact Sheets #15 DERMATOMYCOSES Foot)]](http://s2.studylib.net/store/data/013216770_1-db2cdf56a16f26d122fecafe6758caad-300x300.png)