The Red Leg - Dermatology
advertisement

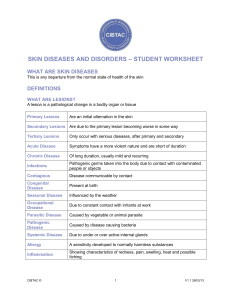
The Red Leg Module Instructions The following module contains hyperlinked information which serves to offer more information on topics you may or may not be familiar with. We encourage that you read all the hyperlinked information. Case 1 Case 1: History HPI: A 65 year old female complains of one week of worsening right lower extremity pain. She states that she has also had a fever and chills since she returned from a camping trip last week. She states that her leg does not itch. PMH: none All: none Meds: none FH: non-remarkable SH: lives in the city with her husband. Denies alcohol, smoking, IV drug use ROS: +fever, chills Case 1: Exam How would you describe these skin findings? Case 1: Exam On exam, VS: T-101.4, HR-80, BP-110/70, RR-14, O2sat 100% Ext: +inguinal LAD Skin: erythematous plaque with ill-defined borders over the right medial malleolus. The lesion is tender to palpation. LABS: WBC-12, Hct 44, Plt 335 Case 1: Question 1 Which of the following are important things to look for on exam of this patient with a red leg? a. Fever b. Elevated white blood cell count c. Lymphadenopathy d. Streaking e. All of the above Case 1: Question 1 Answer: e Which of the following are important things to look for on exam of this patient with a red leg? a. Fever b. Elevated white blood cell count c. Lymphadenopathy d. Streaking e. All of the above What is Lymphatic Streaking? Lymphatic Streaking Lymphatic streaking is seen when the lymphatic vessels are involved and inflamed! Case 1: Question 2 What is the most likely diagnosis? a. cellulitis b. tinea corporis c. stasis dermatitis d. hemophilia Case 1: Question 2 Answer: a What is the most likely diagnosis? a. cellulitis b. tinea corporis (less likely to have a fever and would expect to see scale) c. stasis dermatitis (would not expect lymphadenopathy, likely would see some pruritus) d. hemophilia (would not see fever or lymphadenopathy and bleeding is typically deeper and into joint spaces) Diagnosis: Cellulitis Cellulitis is a very common infection occurring in up to 3% of people per year and is most commonly found in middle aged men Cellulitis results from an infection of the dermis that often begins following either a wound or fungal infection Remember to inquire about IV drug use in the area! Group A beta hemolytic strep and Staph aureus are the most common causal pathogens It is important to recognize and treat cellulitis early as it may lead to SEPSIS or NECROTIZING FASCIITIS! Cellulitis: Clinical Presentation Cellulitis typically presents as a rapidly spreading erythematous, non-fluctuant tender plaque The lower leg is most commonly involved There is often lymphatic streaking The patient may be febrile and toxic There may be an elevated WBC count Lymphadenopathy may be present Cellulitis: Pearls Cellulitis is almost always UNILATERAL! Bilateral lower extremity cellulitis almost never happens, so resist making this diagnosis in patients with bilateral painful red legs with NO fever, white count, LAD, or streaking Tinea pedis serves as a common portal of entry for bacteria, especially in cases of recurrent cellulitis It is important to always look for and treat tinea pedis in cellulitis patients! Erysipelas Erysipelas is a superficial cellulitis that extensively involves the lymphatics Often caused by group A strep and affects older adults There are raised, firm, shiny plaques on exam These plaques may develop overlying blisters (bullae) It often involves the face or lower extremities It is often associated with white count >20,000 It is often preceded by chills, fever, headache, vomiting, and joint pain Erysipelas on Exam On exam, there is a large, shiny erythematous plaque with ill defined borders located on the posterior thigh Cellultis and Erysipelas: Treatment Cellulitis and erysipelas are similar diseases and are treated similarly with: Empiric IV antibiotics to cover Strep and Staph If there is no response, one may consider MRSA as the possible cause and change antibiotics appropriately Draw blood cultures to assess for sepsis Elevation on the involved area Treat tinea pedis if present as it may be the portal of entry for >80% of cellulitis cases 17 Case 2 Case 2: History HPI: A 58 yo male who had a total hip replacement 2 days ago and is now on the surgery floor recovering is found to have redness of his left leg. He states that the leg is painful but does not itch. PMH: left hip replacement 2 days ago All: none Meds: lisinopril, atenolol, glyburide FH: non-remarkable SH: lives in the city with his wife and children. Patient denies alcohol, smoking, or IV drug use ROS: +fever Case 2: Exam On exam, VS: T-102.1, HR-110, BP90/50, RR-18, O2sat 98% Gen: ill appearing Skin: large erythematous plaque with central patches of dusky blue discoloration 20 Case 2: Question 1 What is the most likely diagnosis? a. cellulitis b. tinea corporis c. necrotizing fasciitis d. erysipelas Case 2: Question 1 Answer: c What is the most likely diagnosis? a. cellulitis (would expect more erythema and less dusky blue discoloration) b. tinea corporis (would not expect patient to be so systemically ill and would expect pruritus) c. necrotizing fasciitis d. erysipelas (would expect more erythema and less dusky blue discoloration) Diagnosis: Necrotizing Fasciitis Necrotizing fasciitis is a serious infection of the fascia just above the muscle It progresses rapidly over the course of days and may follow surgery or trauma, or have no preceding visible lesion It can be caused by group A strep, staph or a variety of other organisms At times, it can be associated with Toxic Shock It is considered a MEDICAL/SURGICAL EMERGENCY with up to a 20% fatality rate! Necrotizing Fasciitis on Exam On exam, one sees an expanding dusky, swollen, red plaque with blue discoloration It may turn purple and blister Anesthesia may develop on the skin of the affected area The infection typically spreads rapidly over the course of hours to days Poor prognostic factors include: age>50, diabetes, atherosclerosis, 7 day delay in diagnosis, infection involving the trunk Necrotizing Fasciitis: Work up and Treatment In cases of necrotizing fasciitis, it is most important to diagnose and treat IMMEDIATELY! An MRI can assist in diagnosing necrotizing fasciitis Diagnosis is confirmed by a deep biopsy in the OR TREATMENT: WIDESPREAD DEBRIDEMENT AND IV ANTIBIOTICS Case 3 Case 3: History HPI: 74 yo woman presents with a rash on her leg that has been present for 3 months. She does not have any pain in her legs but does not some itch. She has not used any medications for this rash. PMH: diabetes, HTN All: none Meds: lisinopril, metoprolol, glyburide FH: non-remarkable SH: lives with her husband in the city. Has been overweight throughout her life ROS: +pruritus Case 3: Exam On exam, VS: non-remarkable Gen: well appearing, overweight woman in NAD Skin: erythematous brown hyperpigmented plaque with fine fissuring and scale located above the medial malleolus on the left lower leg Case 3: Question 1 What is the most likely diagnosis? a. cellulitis b. erysipelas c. stasis dermatitis d. tinea corporis e. atopic dermatitis Case 3: Question 1 Answer: c What is the most likely diagnosis? a. cellulitis (would expect fever without scale or pruritus) b. erysipelas (see above) c. stasis dermatitis d. tinea corporis (would have a more defined border and be erythematous) e. atopic dermatitis (incorrect distribution and age group) Diagnosis: Stasis Dermatitis Stasis dermatitis is the most commonly missed diagnosis when evaluating a patient with a red leg! It results from inadequate function of the venous system due to anatomic abnormalities (loss of valves, perforators, congenital abnormalities) Over time, valves age and for this reason older patients tend to have stasis dermatitis more commonly. Stasis Dermatitis on Exam Stasis dermatitis typically presents as erythematous plaques with fine fissuring and a yellowish or light brown hyperpigmentation located superior to the medial malleolus May have an associated dermatitis with weeping, scale, or lichenification Patient may have a red, hot, swollen leg in the ABSENCE of fever, leukocytosis, LAD, or streaking On exam, edema is often present, as well as varicose veins and hemosiderin deposits Hemosiderin: Pinpoint yellow-brown macules and papules Stasis Dermatitis on Exam On exam, There is a large erythematous plaque with fine fissuring and scale as well as interspersed brown macular hyperpigmentation Pinpoint brown macule (hemosiderin) Stasis Dermatitis: Complications Stasis dermatitis can be complicated by a number of conditions: Cellulitis Ulceration Contact dermatitis Eczematous dermatitis It can also lead to to fat necrosis (sclerotic panniculitis/ lipodermatosclerosis) with the end stage being permanent sclerosis (lipodermatosclerosis) with “inverted champagne bottle” legs as seen here Stasis Dermatitis: Complications Stasis dermatitis is a chronic condition and may result in many bouts of cellulitis. This may result in lymphatic insufficiency. The recurrent infection, usually in the setting of obesity, results in edema that becomes firm (nonpitting) The overlying skin becomes pebbly, hyperkeratotic and rough (elephantiasis verrucosa nostra = lymphostasis verrucosa cutis) Ulceration in this setting (with lymphatic and venous insufficiency) is significantly harder to treat and heal Stasis Dermatitis: Diagnosis Venous Rheography is a non-invasive study using light reflection to assess for venous insufficiency. It is often helpful Visual inspection is a very poor indicator of venous competence of the lower leg If peripheral pulses are diminished or leg hair is absent this may suggest underlying arterial insufficiency making ABI (ankle/brachial index) an important study ABI = systolic blood pressure of the leg/systolic blood pressure of the arm (put in normal range) which indicates the degree of limb ischemia Normal Range: 1-1.3 (greater than 1.3 suggests arterial calcification) Claudication Range: 0.5-0.9 (pain from ischemia with activity) Severe Range: <0.5 is referred to surgery (<0.3 can result in rest ischemia and gangrene) Stasis Dermatitis: Treatment When considering the treatment of stasis dermatitis it is important to treat both the eczematous symptoms as well as the underlying venous insufficiency Application of super-high and high potency steroids to area of dermatitis under the wrap Elevation (to reduce edema) Unna boot wrapping with Coban or Profore (4 layer wrap) Unna boot is a special gauze used for stasis dermatitis and ulcers Ace bandage compression Change wraps weekly, or more often if the lesion is very weepy Compression Therapy is Effective! PRIOR TO TREATMENT FOLLOWING TREATMENT Case 4 Case 4: History HPI: A 65 year old female complains of one week of a itchy rash on her right leg. She states that she otherwise feels well. She returned from a camping trip two weeks ago. She has never had anything like this before. PMH: none All: none Meds: none FH: non-remarkable SH: lives in the city with her husband. Denies alcohol, smoking, IV drug use ROS: negative Case 4: Exam On exam, VS: afebrile Gen: well appearing in NAD Skin: erythematous plaque located on the medial right leg with erosions. Case 4: Question 1 What is the most likely diagnosis? a. cellulitis b. necrotizing fasciitis c. vasculitis d. contact dermatitis Case 4: Question 1 Answer: d What is the most likely diagnosis? a. cellulitis (would expect fever) b. necrotizing fasciitis (would expect fever and systemic illness) c. vasculitis (would expect purpura) d. contact dermatitis Contact Dermatitis Contact dermatitis comes in two varieties Irritant dermatitis – will cause symptoms in most people. Symptoms occur without previous exposure. More common than allergic contact dermatitis and can result from a variety of chemicals Allergic contact dermatitis – will only affect those with a sensitivity. Symptoms are delayed for hours-days after exposure. CHARACTERIZED BY ITCH In this case, the patient had allergic contact dermatitis as evidenced by her symptoms taking time to develop following her exposure (camping trip) Allergic Contact Dermatitis: Presentation In allergic contact dermatitis, the lesion appears erythematous, edematous, and often blistered The initial outbreak typically occurs 7-10 days after exposure Subsequent outbreaks may appear within hours of exposure and usually within 2 days The patient typically appears well with no fever or elevated WBC count Allergic Contact Dermatitis: Causes There are a number of causes of allergic contact dermatitis including: Rhus dermatitis (poison oak, poison ivy, poison sumac all contain urushiol) Topical medications neomycin and bacitracin (reason to use polysporin) Nickel Rubber Gold Formaldehyde Thimerosal Contact Dermatitis Treatment Treatment involves both the removal of the causal agent as well as topical corticosteroids Case 5 Case 5: History HPI: 58 yo woman is in the hospital after having had a kidney transplant two months ago. Over the past few weeks she notes a worsening itchy rash on her legs. She has never had anything like it before PMH: diabetes, renal failure All: hay fever Meds: cyclosporine, oral prednisone, insulin FH: non-remarkable SH: lives at home with her husband and 2 children ROS: negative Case 5: Exam On exam, VS: afebrile Gen: well appearing, NAD Skin: large erythematous annular plaque with a raised scaly border Case 5: Question 1 Which is the most appropriate study to perform at this point? a. deep punch biopsy b. debridement c. IV antibiotics d. KOH prep e. MRI to assess for depth of involvement Case 5: Question 1 Answer: d Which is the most appropriate study to perform at this point? a. deep punch biopsy b. debridement c. IV antibiotics d. KOH prep e. MRI to assess for depth of involvement Case 5: KOH Results Hyphae seen on KOH prep KOH FINDINGS CONFIRM THAT THE DIAGNOSIS IS A FUNGAL INFECTION IN THIS CASE TINEA CORPORIS Diagnosis: Tinea Corporis Tinea corporis is an infection caused by a dermatophyte and diagnosed by +KOH Fungal infections are named based on their location on the body. In this case tinea corporis as the infection is involving the body Other locations are tinea pedis (foot) and tinea capitis (head) Tinea corporis often takes weeks or months to develop and when found on the leg as in this case it may originate from tinea pedis or tinea cruris (groin) In this case, the patient’s immunosuppression allowed for a more severe case Tinea Corporis: Clinical Features The following are typical findings as demonstrated by the image on the left Annular erythematous plaques Edges of plaques are often serpiginous Overlying scale Advancing scaly border Clearing in the center of the plaques Tinea Corporis: Treatment The mainstay of treatment is topical antifungal medications However, in severe cases such as the one in Case 5, systemic anti-fungals become necessary Other Causes of Red Leg Pigmented Purpuric Eruption 1-3 cm patch/plaques on the lower leg Confluent tiny papules with hemorrhage Brown-yellow hyperpigmentation due to iron deposition Location: Pretibial Chronic, benign condition Favors elderly men May be pruritic or asymptomatic Starts distally, with slow, chronic proximal progression Asteatotic Dermatitis (Xerotic Eczema) Caused by the loss of the epidermal water barrier More common in the elderly Worsened by hot showers, deodorant soaps Worse in the winter (dry, heated air) Worse after ski trips (altitude, cold) Asteatotic Dermatitis (Xerotic Eczema) Affects lower legs, flanks, arms Spares armpits, groin, face First stage: Second stage: flaking of the skin, pruritic cracking of the skin looking like the bed of a dry lake itchy and stings Third stage: Weepy dermatitis, ITCHY Asteatotic Dermatitis on Exam Erythematous patch with dry scaling and cracking as well as scattered excoriated papules Asteatotic Dermatitis: Diagnosis Diagnostic Pearl: Itching is relieved by prolonged submersion in bath (20-30 minutes) The itching then begins again 5-30 minutes after getting out of the water Asteatotic Dermatitis: Treatment Moisturize Soap to the axillae, groin, scalp only Medium potency topical steroid (TAC) ointment to the areas of redness and itch Severe cases, soak in tub 20 minutes, apply TAC ointment, cover with Saran Wrap and sleep in it Summary: Causes of a Red Leg Cellulitis/erysipelas Necrotizing fasciitis Stasis dermatitis Vasculitis Pigmented purpuric dermatosis Asteatotic dermatitis Tinea Corporis Contact dermatitis Take Home Point: Distinguishing Cellulitis Fever Pain Warmth Bilateral Streaking Lymphadenopathy Elevated WBC Cellulitis Yes Yes Yes Almost never Yes Yes Yes Consider another diagnosis No +/- +/- often No No No END OF MODULE