Blood Loss
advertisement

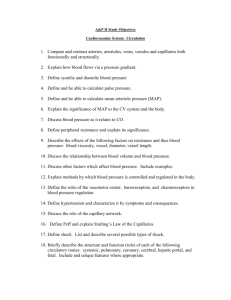
Lesson 6 Circulation, Hemorrhage, and Shock Circulatory System • A functioning circulatory system requires: – A heart that pumps adequately – Intact blood vessels to contain the fluids (blood) being pumped – Adequate amount of blood (fluid) to fill the vascular container Metabolism • All cells require energy to function • Energy is stored within the cell in the form of adenosine triphosphate (ATP) molecules • Aerobic metabolism – Oxygen is required for efficient production of ATP (energy) • Anaerobic metabolism – Inadequate oxygen results in decreased energy (ATP) production and accumulation of lactic acid Shock • Results from inadequate energy production to sustain life • Any condition that causes generalized cellular hypoperfusion • Leads to inadequate cellular oxygenation that does not meet metabolic needs Hypoperfusion (1 of 2) • Results from: – Loss of blood (either externally or internally) • Most common cause of shock in trauma – Impaired pumping of blood – Dilation of the blood vessels (increased vascular space) Hypoperfusion (2 of 2) • The end result is a decrease in circulating volume and red blood cells (RBCs) moving through the capillary beds to deliver oxygen to the cells • Lack of oxygen impairs metabolism • Impaired metabolism decreases energy production Shock in Trauma • Classifications – Hypovolemic – Distributive – Cardiogenic Hypovolemic Shock (1 of 2) • The most common cause of shock in the trauma patient – Due to hemorrhage • Loss of RBCs impairs oxygen transportation – In any trauma patient with shock, assume hemorrhage is the cause until proven otherwise Hypovolemic Shock (2 of 2) The values and descriptions for the criteria listed for these classes of shock should not be interpreted as absolute determinants of the class of shock, as significant overlap exists. Distributive Shock • Neurogenic “shock” – Decreased systemic vascular resistance due to vasodilation • Most common cause is spinal cord injury Cardiogenic Shock • Intrinsic – Blunt cardiac trauma leading to muscle damage and/or dysrhythmia – Valvular disruption • Extrinsic – Pericardial tamponade – Tension pneumothorax Assessment (1 of 7) Evaluate: – Hemorrhage – Level of consciousness – Skin – Pulse – Respiration – Blood pressure – Confounding factors Assessment (2 of 7) • Hemorrhage – If present must be controlled ASAP • External – Address in the prehospital setting • Internal – Transport to appropriate destination Assessment (3 of 7) • Level of consciousness (LOC) – Decreased cerebral perfusion results in altered LOC – Assume altered LOC is due to shock, and treat accordingly – Other causes of altered LOC will not kill as rapidly as shock Assessment (4 of 7) • Skin – Color – Temperature – Moisture – Capillary refill • Pulse – Rate – Quality – Location Assessment (5 of 7) • Respiration – Hypoxia, hypercarbia, and acidosis stimulate the respiratory center – Increasing ventilatory rate may be the earliest sign of shock – Intolerance of oxygen face mask suggests hypoxia Assessment (6 of 7) • Blood pressure (BP) – Not the determinant of shock • 30% blood loss before BP drops – Not part of the primary assessment – Trends are crucial – Adequate blood pressure does not equate to adequate tissue perfusion – Treatment is not aimed at returning BP to normal Assessment (7 of 7) Complicating factors – Patient age – Medications – Pregnancy – Pre-existing conditions Shock Without Obvious Cause (1 of 4) • Assume the patient is bleeding somewhere, even if you can’t see it – Internal hemorrhage – Fracture Shock Without Obvious Cause (2 of 4) • Internal hemorrhage – The chest and abdomen can hold large volumes of blood – The chest is usually associated with visible external signs of trauma; the abdomen often is not Shock Without Obvious Cause (3 of 4) • Internal hemorrhage (cont’d) – Abdominal trauma is a cause of significant hidden hemorrhage – Assume abdominal trauma if hypovolemic shock is not otherwise explainable Courtesy of Peter T. Pons, MD, FACEP Shock Without Obvious Cause (4 of 4) • Fractures – Multiple fractures – Blood loss into the surrounding soft tissues from a long-bone fracture, such as the femur, can be significant – Blood loss into the pelvic and abdominal spaces from a pelvis fracture can be massive Mechanism of Injury and Shock (1 of 3) • Penetrating injuries – Object traverses the chest, abdomen, or extremity – May injure organs, tissues, and blood vessels along its pathway Courtesy of Lance Stuke, MD, MPH Mechanism of Injury and Shock (2 of 3) • Blunt injuries – Path of injury is less visible – Force (energy) is applied to the trunk and extremities – Energy is transmitted to the thoracic and abdominal organs and bones causing damage Mechanism of Injury and Shock (3 of 3) • Blunt injuries (cont’d) – Compression, cavitation, and deceleration can tear and shear organs and blood vessels and fracture bones – Damaged organs, tissues, and blood vessels bleed into the surrounding cavities and tissue – As the amount of blood lost increases, signs of shock develop Injuries Commonly Associated With Hemorrhagic Shock Traumatic Aortic Rupture (Tear) • Usually occurs at the junction of the mobile and fixed portions of the aorta just beyond the left subclavian artery • 80% to 85% die prehospital from intrathoracic hemorrhage McSwain NE Jr, Paturas JL: The Basic EMT: Comprehensive Prehospital Patient Care, ed 2, St. Louis, 2001, Mosby – Of those who survive, 50% die within 48 hours if not treated. Hemothorax • Bleeding into the pleural cavity • Blunt or penetrating mechanism • Each hemithorax can hold up to 30% to 40% of a patient’s total blood volume Abdominal Organ Injury (1 of 2) • Results from a blunt or penetrating mechanism • Injury to: – Solid organs (liver, spleen, kidney, pancreas) • Results in hemorrhage that varies from mild to lifethreatening • May also be associated with leak of enzymes, bile, or urine into abdomen Abdominal Organ Injury (2 of 2) • Injury to (cont’d): – Hollow organs (small and large bowel) • Usually not a cause of major blood loss • Leak contents and cause peritonitis Fractures (1 of 2) • Major or multiple fractures can lead to significant blood loss • Femur or pelvic fractures are the most common cause • Do not underestimate blood loss due to multiple fractures Fractures (2 of 2) Fracture (Isolated) Single rib Radius or ulna Humerus Tibia or fibula Femur Pelvis Blood Loss (ml) 125 250–500 750 500–1000 1000–2000 Massive Courtesy Norman McSwain, MD, FACS, NREMT-P Rib Fractures • Most common thoracic injury • Usually in ribs 4–8, laterally • May be associated with injuries to intercostal blood vessels, liver, spleen, or lung Courtesy of Peter T. Pons, MD, FACEP. Injuries Commonly Associated With Distributive Shock Neurogenic “Shock” • Secondary to spinal cord injury, usually cervical spine (down to T6) • Loss of sympathetic system vascular tone – Blood vessels dilate – Blood return to the heart decreases and cardiac output drops • Perfusion and tissue oxygenation are usually maintained – Skin remains warm and dry Injuries Commonly Associated With Cardiogenic Shock Pneumothorax • Tension – Blunt or penetrating – Breath sounds decreased or absent – Marked ventilatory distress – Hemodynamic compromise • Simple – Blunt or penetrating – Breath sounds decreased or absent – Mild to moderate ventilatory distress – No hemodynamic compromise Pericardial Tamponade • Penetrating mechanism most common • Blood in pericardial sac: – Compresses the heart – Prevents adequate filling – Thus, cardiac output decreases Blunt Cardiac Injury • Direct injury to heart muscle – May cause: • Dysrhythmia – Sinus tachycardia most common • Right atrial or right ventricular rupture • Valve rupture — rare – New murmur • Sudden death Shock Management (1 of 14) • Four questions guide prehospital management: – What is the cause of shock in this particular patient? • Hemorrhage is the most common – What is the care for this type of shock? – What can and should be done between now and the time the patient reaches definitive care? – Where is the best place for the patient to get definitive care? Shock Management (2 of 14) • Proper shock management – Improves the oxygenation of RBCs – Improves the delivery of RBCs to the tissues • Airway – What are the needs? • Ventilation – Does it require assistance? Shock Management (3 of 14) • Oxygenation – Is it adequate? • Circulation – Hemorrhage controllable? Shock Management (4 of 14) • Patient positioning – Supine – Trendelenburg position no longer recommended • Allows the abdominal organs to push up on the diaphragm and impede its movement • No benefit in elevating lower extremities Shock Management (5 of 14) • Hemorrhagic shock – Critical to stop ongoing blood loss and to maintain perfusion – Hemorrhage control • External hemorrhage • Internal hemorrhage Every RBC counts! Shock Management (6 of 14) • Hemorrhagic shock (cont’d) – External hemorrhage control • Direct pressure will control most external hemorrhage • Tourniquet • Immobilization of fractures • Topical hemostatic agents (use to pack bleeding wounds) – Internal hemorrhage • Controlled in the operating room External Hemorrhage Control Shock Management (7 of 14) • Fluid therapy in hemorrhagic shock – Balanced resuscitation • Balance between how much fluid is given and how high the BP is raised • Excessive resuscitation leads to increased bleeding Shock Management (8 of 14) • Patients with signs of hemorrhagic shock – Maintain systolic BP at approximately 80–90 mm Hg – If signs of traumatic brain injury are present, maintain systolic BP at approximately 90–100 mm Hg – Adult patients may require 1000–2000 ml of warmed lactated Ringer’s solution or normal saline – Pediatric patients: 20 ml/kg bolus Shock Management (9 of 14) • Reassessment following fluid therapy • Three responses: – Rapid response • Suggests that hemorrhage has stopped, may still require surgery – Transient response • Significant blood loss and probably ongoing hemorrhage, requires urgent surgery – Minimal or no response • Massive ongoing hemorrhage, requires immediate surgery Shock Management (10 of 14) • Distributive (neurogenic) shock – Must rule out hemorrhage as the primary cause of shock – Spine movement restriction (immobilization) – Fluid administration Shock Management (11 of 14) • Cardiogenic shock in trauma – Extrinsic • Tension pneumothorax – Needle decompression • Pericardial tamponade – Rapid transport – Fluid administration – Intrinsic • Treat dysrhythmias as necessary • Prevent fluid overload Shock Management (12 of 14) • Transport considerations – Transport without delay to appropriate destination • Most procedures may be accomplished while en route – Maintain body temperature • Cover patient after completing assessment • Patient compartment temperature should be kept as warm as possible Shock Management (13 of 14) • Prolonged transport – Ensure airway and optimize ventilatory status – Maintain external hemorrhage control – Prevent body heat loss – Reassess, reassess, reassess Shock Management (14 of 14) • Left untreated, shock progresses • Prehospital care can affect outcome by helping to restore perfusion and energy production • Managing shock in the prehospital setting can help prevent the cascade of cell death, organ death, and patient death Minimizing Complications (1 of 2) • Assess for and recognize the signs of shock • Assume hemorrhagic shock until proven otherwise – Control external hemorrhage as rapidly as possible • Cardiac output and tissue oxygenation are impaired early Minimizing Complications (2 of 2) • Restore and maintain airway, ventilation, oxygenation, and circulation • Hypothermia creates a cycle of worsening shock and hypothermia • Transport without undue delay Summary • Shock is a state of cellular hypoperfusion, leading to inadequate energy production to meet metabolic needs • The most common cause of shock in the trauma patient is hemorrhage • Shock is hemorrhagic until proven otherwise • The management of shock is aimed at improving oxygenation of RBCs, improving delivery of oxygenated RBCs to the microcirculation, and controlling hemorrhage Questions?