Nursing Care of Patients with Alterations in the GI tract
advertisement

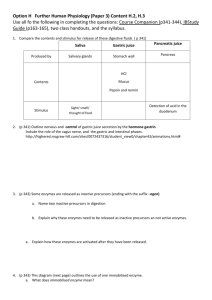
Nursing Care of Patients with Alterations in the GI tract C. Cummings RN,EdD A & P of GI system GI tract • Hollow muscular tube, lumen surrounded by 4 tissue layers: – Mucosa- innermost, thin layer of smooth muscle and exocrine cells (layer that sloughs off w/ ulcerative colitis) – Submucosa- connective tissue – Muscularis- smooth muscle – Serosa- outermost, connective tissue GI tract • Function: – Secretion- secretes HCL acid, digestive enzymes – Digestion- mechanical and chemical, food is broken down to chyme – Absorption- from GI tract to blood supply – Motility – Elimination – (absorbs all the minerals, w/out a GI tract you will die… stomach has pH of about 2… very acidic… if it leaks out it will cause big problems) GI tract • Nerve Supply – Intrinsic stimulation by myenteric plexus in smooth muscle and submucosa plexus in inner layer – Autonomic system- Parasympathetic stimulation by vagus nerve, connects with intrinsic system • Vagus-stimulates motor and secretory activity and relaxes spinchters – Sympathetic system- thoracic and lumbar splanchnic nerves slows movement, inhibits secretions and contracts spinchters – (Parasympathetic slows down the GI tract… fight or flight… don’t have to go to bathroom while trying to save yourself) Nerves of GI tract Mouth • Function: – Mastication, taste, begin movement – Glands produce 1 L of saliva/day – Saliva contains mucin and salivary amylase with begins to break down CHO – Oral preparatory phase- food is softened, made into a “bolus” and tongue moves to the back of the mouth – Oral phase- tongue presses bolus against hard palate, elevates the larynx and forces the food bolus to the pharynx, triggering swallowing (coughing opens the flap) – Pharyngeal phase- soft palate elevates and seals nasal cavity, inhibits respirations and allows esophagus to open – Esophageal phase- is when bolus enter at cricopharyngeal juncture, peristalsis now takes food to the stomach – All this takes about 10 seconds ! Esophagus • Canal about 10 in long, passes through the center of the diaphragm • Upper end is the upper esophageal sphincter, at rest it is closed to prevent air from entering the esophagus • Lower end is the lower esophageal sphincter, it sits at the gastroesophageal junction, at rest it is closed to prevent reflux of gastric contents, this is where GERD occurs (problems w/ the LES… doesn’t shut all the way, chocolate & pepermint keeps the sphincter open, large bolus of food can keep it open… GERD) • Function- to propel food and fluids and prevent reflux • Mucous is secreted to move the food along • Cardiac sphincter of the stomach opens to allow the food to enter Stomach • Digestive and endocrine organ, in midline and LUQ • Four regions: – Cardia- narrow part that is distal to the gastroesophageal junction (part closest to the heart) – Fundus- left above the GE junction – Body or corpus- largest area – Antrum- pylorus, is the distal portion and is separated from the duodenum by the pyloric sphincter, prevents backflow from the duodenum (at end) – Surface is covered in rugae or folds and have smooth muscle for motility – Has intrinsic and extrinsic nerves – (reglan stimulates the vagus nerve, causes contractions… gets food out of the stomack) Function: Stomach Parietal cells secrete HCL acid and intrinsic factor, which absorbs B 12, without it, what anemia can occur? Pernicious anemia… makes you weak & tired… red beefy tounge, B12 injections & pill… pill not as effective… water soluble vitamin Chief cells secrete Pepsinogenpepsin (breakdown enzyme) Cephalic phase- sight, smell and taste of food, regulated by vagus, begin secretory and contractile activity Gastric phase- G cells in the antrum secrete gastrin, which causes HCL and pepsinogen to be released. HCL changes pepsinogen to pepsin, which digest proteins. Mucous and Bicarb (prostoglandins) are secreted to protect the stomach wall (from the acid produced) Intestinal phase- chyme produced empties into the duodenum and causes distention, this produces secretin, which stops the acid production and gastric motility ! Stomach Small Intestine • Longest portion of the GI tract, 16-19 ft. • Made up of 3 sections: – Duodenum- first 12” and is attached to the pylorus. The CBD (common bile duct) and pancreatic duct join to form the ampulla of Vater and empty into the duodenum at the duodenal papilla. This surrounded by a muscle, called the Sphincter of Oddi – Jejunum- middle 8 ft portion – Ileum- last 8-12 ft. The ileocecal valve separates the ileum form the cecum of the large intestine – Inner lining is made up of intestinal villi and folds of mucosa and submucosa for digestion. – (all 3 sections for digestion) Small Intestine • 3 main functions: – Movement- mixing and peristalsis • Moves chyme by segmental contractions and mixes with enzymes – Digestion- enzymes produced by the intestinal cells make: • Enterokinase, peptidases, lactase, maltase and sucrase • Help to digest CHO, proteins and lipids – Absorption- absorbs most of the nutrients from food, takes 3-10 hours for the contents to pass through • Major organ for absorption Small intestine Large Intestine • Ileocecal valve to the anus, 5-6’, lined with columnar epithelium tha thas absorptive and mucous cells. • Cecum- is the beginning, dilated pouch like structure, appendix is attached to the base • Colon has 4 divisions: – Ascending, transverse, descending and sigmoid • Rectum- last 6-8” to the sphincter muscles and anus • Main function is absorption of water (problem w/ ileostomy… watery feces b/c water hasn’t been absorbed yet) Large Intestine • Function: – Movement- segmental contractions, to allow time for the water and electrolytes to be absorbed – Absorption- absorbs most of water and electrolytes, reduces fluid volume of chyme and creates a more solid mass for elimination – Elimination- 3-4 strong peristaltic contraction /day triggered by colonic distention in proximal large intestine to propel contents to rectum, until urge to defecate. Nursing Assessment • Family history- GI disorders, cancer • Personal history- what kinds of things? • Diet history- anorexia, dyspepsia- what is that? What should you question them on for diet history? • Health history- diarrhea, constipation, # and color of stools, change in wt. or appetite • Abdominal pain– – – – – P- precipitating Q-quality- how intense, severe, type R-region or radiation S- severity scale- 0-10 T-timing- when did it first occur, duration and frequency Physical Assessment • Abdomen: – Inspection- skin, symmetry, rashes, lesions, scars – Auscultation- all four quadrants, normally heard in 515 seconds, normal, hypoactive or hyperactive, listen 1 full minute. What is borborygmus (very hyperactive bowel sounds)? Why would bruits be heard? (aortic) Why would there not be bowel sounds heard? – Percussion- tympanic- air filled, dull- organ – Palpation- light and deep palpation, masses, tenderness, look for guarding (w/ appendicitis, no pain felt until you release… McMurry’s sign) Lab tests • CBC- anemia • Oncofetal antigens- CA19-9 and CEA (carciniogenic embryonic antigen), used to monitor for cancer in the GI tract • Ca- decreased in malabsorption • K – decreased with vomiting, diarrhea • (also decreased Magnesium can be a problem) • Xylose absorptiondecreased indicates possible malabsorption in the small intesting (tells if you can absorb carbs… not common & won’t ask question about) • Stool for Occult blood • Stool for ova and parasiteinfection • Stool for fecal fat- increased with Crohn’s disease and malabsorption • • Radiology Abdominal films- air in bowel and masses Upper GI and small bowel- pharynx to duodenojejunal junction, barium swallow and SBFT – NPO 8 hours before, drink barium, then lie, stand and turn in multiple directions to view movement of barium – SBFT- drink more barium and view passage – After drink fluids to pass barium – (almost all the tests need GI prep, get rid of stool, gas & free air so when you put dye in you can see… NPO 8 hrs before test) • Barium enema – Large intestine, done for obstructions, masses, not done is perforated colon or fistulas – Only clear liquids for 12-24 hours prior, NPO, given bowel prep like Golytely – Insert rectal catheter with a balloon and give 500-1500 ml of barium and hold – Can be uncomfortable, must take a laxative after – (eat or drink chalk dye) – (Must get rid of the barium afterwards… prep afterwards, will turn to concrete if it stays in gut) Diagnostic Tests • EGD- esophagogastroduodenoscopy (what I saw in GI lab) • Visualize esophagus to duodenum, NPO prior, given versed and fentanyl, maybe cetacaine to inhibit gag reflex, pass tube and visualize structures, can take biopsies • Gag reflex may not return for 1-2 hours after, so no eating or drinking until then (put tounge blad in throat to see if it returned) • Colonoscopy- large bowel, take biopsies and remove polyps, have a bowel prep prior, given versed and fentanyl prior; Capsule enteroscopy is now done to visualize, apply a data recorder to the abdomen and the patient swallows the capsule • Proctosigmoidoscopy- like colonoscopy, only a rigid tube, less invasive and does not require the cleansing of the colonoscopy Colonoscopy Case Study • 72 year old male admitted with chest pain and nausea. He states that he awakens in the night with pain in his chest and nausea. • What would you do first to evaluate his condition? • What diseases could he have? (GERD, hiatal hernia, ulcer) • What kind of lab work would you like to obtain? (cardiac enzymes, CBC, electrolytes) • What past medical history do you need? (heart problems, GERD, GI bleed, what did he eat, when did he eat, drink alcohol Case Study • Your patient starts to have hematemesis. • What does this mean? (GI bleed) • Is this life-threatening? (yes, lots of elderly die from GI bleed) • What interventions should be done? (give blood & normal saline, will probably have to go to surgery to fix problems… cut out part of stomach that is bleeding) • What could have caused this condition? (if peritonitis, can get massive infection, mesentary is aggravated by blood & other stuff, makes stomach pull in fluid from other areas, get rigid boardlike abdomen (TEST QUESTION) Case Study • It is determined that your patient can be treated nonsurgically. What medications would be given? (should have 3) Protonix, prilosec & nexium (proton pump inhibitor, stimulates parietal cells) H2 (histamine) blockers, zantac, axid & pepsic… there will be many test questions about meds on exam!!! Also give an antacid (malox, gaviscon… seep in stomach, bicab based & coat stomach & bring up pH level) Reglan can help to empty stomach (prokinetic med) • What type of teaching would be done for prevention? (cut down on alcohol, smoking, no spicy foods, take zantac before you eat) • If he needed surgery, what could have been done? Esophageal Problems • GERD- gastroesophageal reflux disease (most common esophageal problem… obesity… eating too much) • Reflux causes esophageal mucosa to be irritated by the effects of gastric and duodenal contents, results in inflammation • Causes: – Inappropriate relaxation of the LES, sphincter tone is decreased (pH of 2 coming into esophagus where pH is normally much higher) – Irritation from refluxed material – Delayed gastric emptying, gastric volume or intra-abdominal pressure is increased – Abnormal esophageal clearance GERD • Refluxed material has a pH of 1.5-2, whereas the esophagus normally has a pH of 6-8 erosive esophagitis, once inflammed, the mucosa can’t eliminate the material as quickly. This leads to increased blood flow and more erosion. Gastric acid and Pepsin cause the tissue injury. • Can lead to Barrett’s epithelium- thicker, but can be cancerous, can also cause hemorrhage, aspiration pneumonia, asthma, laryngitis and dental deterioration. GERD GERD • Physical Manifestations: – Dyspepsia- heartburn, substernal or retrosternal burning that moves up and down in wavelike fashion, pain may radiate to neck or jaw or back, worsens when bends over, strains or lies on their back, occurs after meals and last 1-2 hours, helped by fluids (to flush, but don’t drink fluid w/ the meal… drink afterwards) and staying upright – Regurgitation- food entering throat without nausea, watch for cough (classic sign), hoarseness or wheezing (because of aspiration into lung… biggest GI complication is aspiration) – Hypersalivation- water brash in response to reflux, fluid without sour or bitter taste GERD • Physical Manifestations – Dysphagia and Odynophagia- difficulty swallowing, esophagus may be narrowed by inflammation or tumor, odynophagia- means what? – Chronic cough, mostly at night – Atypical chest pain – Belching and flatulence or bloating • Diagnosis: – Endoscopy, 24 hour ambulatory pH monitoring- pass a small tube into esophagus and monitor pH levels GERD • Nursing Diagnoses: – – – – – What diagnoses would apply to these patients? 1. altered nutrition 2. risk for dehydraion 3. electrolyte imbalance 4. acute pain (maybe) • Interventions: – Diet therapy- what type of dietary modifications would be appropriate? – Certain foods decrease LES pressure- chocolate, fat and mints. Also, smoking and alcohol decrease – Spicy foods irritate the esophagus and Carbonated can increase gastric pressure GERD • Lifestyle changes: – How should they sleep? (propped up on pillows) – What things increase intra-abdominal pressure? (ascites, liver failure, cancer in GI tract, obesity, pregnancy, Cushing’s, renal failure… fluid presses on stomach & gives GERD, respiratory problems) • Drug therapy: – Goal is to inhibit gastric acid secretion, accelerate gastric emptying and protect the gastric mucosa – Antacids: • Elevate the pH and deactivate pepsin, good for heartburn, take 1 hour before and 2-3 hr after a meal • Name 2 antacids. (malox, mylanta, gaviscon) GERD • Drug therapy: – Histamine Receptor Antagonists • Decrease acid, help promote healing of the esophagus • Name 2 common ones sold OTC (generic ends in “dine”) – Proton Pump Inhibitors • Main treatment for GERD, long acting inhibition of gastric acid secretions by inhibiting protom pump of parietal cell, can reduce by 90%/ day • Name 2 proton pump inhibitors (generic ends in “zole” once a day or q 12 h at most)) • Other therapies: GERD – Consider medications that may lower LES pressure (make it worse)- oral contraceptives, anticholinergics, sedative, tranquilizers, B-adrenergic agonists, nitrates and Ca channel blockers (they all slow gut movement, then reflux occurs as food stays longer in stomach) – Prokinetic drugs- for emptying and peristalsis- metoclopramide (reglan) – Endoscopic: • Enteryx procedure- spongy material in LES to tighten it Stretta procedure- radiofrequency energy through needles to inhibit the vagus nerve – Surgical: • Laparoscopic Nissen Fundoplication (main surgical procedure for GERD, takes stomach muscle up & wrap around esophagus to make it able to tighten, used a lot for hiatal hernia) • Angelchik esophageal antireflux- anchors the LES in the abdomen to increase sphincter pressure (not as common) Hiatal Hernia • Protrusion of stomach through the esophagus • Sliding or Rolling hernias • Symptoms are similar to GERD patient (pain 1 to 2 hours after you eat… usually will vomit non digested food… food hasn’t even gotten into the stomach) • Nonsurgical management is like GERD • Surgical: – Lap Nissen Fundoplication (same as GERD)- reinforces the LES, wraps a portion of the stomach around the distal esophagus to anchor it – Post op- risk for bleeding (biggest risk), infection and respiratory complications (don’t want to take a deep breath b/c it hurts • Have an NGT, begin PO once BS return • Watch for gas-bloat syndrome and air swallowing • MAY GET questions about when can you eat… must have bowel sounds return before eating TEST!!! Nursing Diagnosis: GERD • Impaired Nutrition: less than body requirements – What things can be done to improve their intake and decrease pain? – What would be the expected outcomes? – How would you monitor their progress? (albumin to check intake) • Acute Pain r/t irritation of the esophagus – What interventions can be performed? • Risk for aspiration r/t reflux of gastric contents – How can you determine that this does not occur? Peptic Ulcer Disease • Mucosal lesion of the stomach or duodenum • Peptic (any type of GI ulcer) can be gastric (top) or duodenal (bottom) • PUD- gastric mucosal defenses become impaired and they can no longer protect the epithelium from acid and pepsin • Three main types of ulcers: – Gastric – Duodenal – Stress (school, life, surgery) Peptic Ulcers Gastric Ulcers • Gastric mucosa is protected by mucous and bicarbonate that maintain a normal pH on the gastric tissue and protects it from acid • Gastromucosal prostaglandins increase the barrier’s resistance to ulceration by producing mucous (aspirin & NSAIDS inhibit prostaglandins… irritates GI) • Integrity is improved by a rich blood supply to the mucosa • If there is a break in the mucosal barrier, HCL acid damages the epithelium. Gastric ulcers result from backdiffusion of acid or dysfunction of the pyloric sphincter. Gastric Ulcers • If the pyloric sphincter doesn’t function, bile backs up into the stomach, produces H+ ion back diffusion and mucosal inflammation • Toxic agents and bile destroy the lipid plasma membrane of the mucosa. Delayed gastric emptying also affects. What drug can be given to improve emptying? • Gastric Ulcers are deep and penetrating and usually are in the lesser curvature of the stomach, near the pylorus • (high fat & protein meals stay in stomach MUCH longer & aggravate… BRAT diet settles … bananas, rice, applesause & tea) Duodenal Ulcers • Occur in the first portion of the duodenum. • Deep lesions that penetrate through the mucosa and submucosa into the muscle layer. The floor of the ulcer consists of a necrotic area on granulation tissue and surrounded by fibrosis • High gastric acid secretion, pH levels are low for long periods • Protein rich meals, calcium and vagal excitation stimulate acid secretion • Hypersecretion, rapid emptying of food from stomach reduces the buffering effect of food and delivers a large acid bolus to the duodenum • Inhibitory secretory mechanisms and pancreatic secretion may be insufficient to control the acid • Many patients have H. pylori infection. H. pylori produces urease changes urea to ammonia, H+ ions released contribute to damage (bacteria release hydrogen ions, greater acid levels) Stress Ulcers • Acute gastric mucosal lesions occurring after and acute medical crisis or trauma • Associated with head injury, major surgery, burns, respiratory failure, shock and sepsis • Bleeding is the principle manifestation • Multifocal areas often in the proximal portion of the stomach and duodenum • Usually elevated HCL acid levels and hospital stay longer than 11 days • (trauma, GI tract slows down, acid just sitting in stomach, causing trouble) Complications of Ulcers • Hemorrhage: – 15-25% of patients with PUD, most serious complication – Most often with gastric ulcers and elderly – After initial bleed, 40% have a recurrence if untreated, especially if H. pylori untreated and no H2 antagonist – Have Hematemesis- bleeding at or above the duodenojejunal junction – Smaller amounts of bleeding are seen as melena (blood in stool), more often seen in duodenal ulcers, stool may appear black. Complications of Ulcers • Perforation (biggest complication) – Gastric or duodenal may perforate or bleed – Stomach or duodenal contents can leak into the abdomen, acid peptic juice, bile and pancreatic juice empty through the anterior wall of the stomach into the peritoneal cavity – Sudden, sharp pain in midepigastric region and spread over the abdomen – Amount of pain correlates with the amount and type of GI contents spilled – Abdomen is tender, rigid and boardlike, go into a fetal position to decrease tension of abdomen – Chemical peritonitis, bacterial septicemia and hypovolemic shock follow paralytic ileus and possible death KNOW****** Complications of Ulcers • Pyloric obstruction – Small number of patients, vomiting caused by stasis and gastric dilation – Obstruction occurs at the pylorus and is caused by scarring, edema, and/or inflammation – Gastric outlet obstruction abdominal bloating, nausea and vomiting (between pyloris & duodenum… can’t pass the food, narrowing) – May go into metabolic alkalosis from loss of large quantities of acid gastric juice (H+ and Cl-) – Hypokalemia may result from the vomiting Complications of Ulcers • Intractable disease – Disease may recur throughout life, stressors, inability to adhere to therapy, no longer responds to management • Cause: – Use of NSAID’s- break down the mucosal barrier and disrupt the protection by COX inhibition. Cause the depletion of prostaglandins, have a high rate of recurrence – Drugs such as Theophylline, corticosteroids (prednisone) and caffeine stimulate HCL acid production – H pylori infection is transmitted person to person – 50% of people with PUD have a first or second line relative with PUD, usually the same type of ulcer Physical Manifestations • Epigastric tenderness, midline between the umbilicus and xiphoid process • May begin as hyperactive BS, then diminish if perforation • Dyspepsia- discomfort around the epigastrium, sharp, burning or gnawing – Gastric- occurs in upper epigastrium with localization to the left of the midline and may be relieved by food (1 to 2 hrs after eat, relieved by food that neutralizes…) – Duodenal- located to the right of the epigastrium, occurs 90 min to 3 hours after eating and awaken at night, may be aggravated by spicy foods, onions, alcohol, caffeine and ASA, NSAIDS (just remember the pain will be later & more midline & to the right) Physical Manifestations • • • • • • • Vomiting may occur Appetite is maintained, unless pyloric obstruction occurs Fluid volume deficit, if bleeding, take orthostatic BPs Watch for Hematemesis and melena Monitor H & H Dx- barium swallow and EGD Test for H. pylori is IgG serologic testing and urea breath testing Nursing Diagnoses • • • • • • • Name 5 diagnoses r/t PUD 1. 2. 3. 4. 5. What would be an expected outcome for this disorder? Nursing Interventions • Drug Therapy – Goals: Provide pain relief, eradicate H. pylori, heal ulcerations, prevent recurrence – Eliminate H. pylori- triple treatment: TEST QUEST • Bismuth product (pepto-bismol, antacids to coat the stomach) or a a proton pump inhibitor (prilosec) and two antibiotics (metronidazole (Flagyl) and tetracycline or amoxicillin) • May have to take medications 4 x’s/day for 14 days and often they don’t complete the series Nursing Interventions • Drug therapy: – Hyposecretory drugs- reduce gastric acid secretions • Antisecretory agents- proton pump inhibitors, “zole” ending, suppress H, K-ATP ase enzyme system of gastric acid production, can be given IV or PO • H2 receptor antagonists- block histamine-stimulated gastric secretions, “dine” ending • Prostaglandin analogues- reduce gastric acid secretion and enhance gastric mucosal resistance to tissue injury, Misoprostol (Cytotec, coats GI tract) helps prevent NSAID induced ulcers, does cause uterine contraction and can not be given to pregnant women Nursing Interventions • Antacids – Buffer gastric acid and prevent formation of pepsin, heal duodenal ulcers – Aluminum hydroxides (may cause constipation) and magnesium hydroxide, may affect those with renal impairment (Mg causes diarrhea, malox) – Take 2 hours after meals to reduce the H+ion load – Calcium carbonate (TUMS) is an antacid, but it triggers gastrin release and causes a rebound acid secretion – Antacids can interact with other drugs- tetracycline, dilantin, also may have a high sodium content • Mucosal Barrier fortifiers- sucralfate (Carafate) supplies a protect coating by forming a complex with proteins, binds with bile acids and pepsin, should be given on an empty stomach and not within 1 hour of eating or taking antacids Nursing Interventions • Diet therapy – Bland diet may help to relieve symptoms – Food may help to neutralize acids, rebound may follow when more acid is released – Avoid foods that stimulate gastric acid release – They are?? – Yoga for stress relief, herbals, such as licorice and vitamins may help Gastrointestinal Bleeding • What would be a nursing diagnosis for GI Bleeding? • 1. hypovolemia, anemai, altered tissue perfusion • 2. altered oxygenation (lack of blood), acute pain…. • What would be the expected outcome and how would you know that this was met? Gastrointestinal Bleeding • Hypovolemia Management – Monitor vital signs and I&O, assess for bleeding and vomiting, monitor CBC – Fluid and electrolyte replacement is necessary, usually NSS or LR, may give PRBC’s or FFP – Watch for signs of shock, what are they?? (drop in BP & elevated HR) • Bleeding reduction – Monitor labs, insert and NGT to decompress the stomach, give an H2 blocker, may need gastric lavage, what is that?? – Ice lavage, cold saline, irrigate & then suction it back out… thought to stop the bleeding in the stomach) Nursing Interventions for GI bleeding • Endoscopic therapy – – – – – EGD, can do: cautery on the bleeding sites inject a sclerosing agent with diluted epipherine Laser therapy Clip the bleeding vessel • Somastatin Analogue- Sandostatin (given IV & also used to stop diarrhea) may be used to suppress gastric acid secretion on parietal and chief cells, vasoconstricts the splanchnic arteries which reduce hemorrhage Surgical management of GI bleeding • MIG- minimally invasive gastrectomy- laproscopic to remove chronic gastric ulcer or treat hemorrhage, make several small incisions, may partially remove the stomach and/or vagotomy to control acid secretion • Gastroenterostomy- creates a passage between the body of the stomach and jejunum, reduces motor activity in the pyloroduodenal area, diverts acid, a vagotomy (cut nerves) may be done with it to decrease secretion. Can do truncal, selective or proximal. Billroth I- connect to duodenum, Billroth II connects to jejunum • Pyloroplasty- widens the exit of the pylorus and empties the stomach Billroth 1 Postop care for GI surgery • NGT management • Monitor for complications of: – Dumping syndrome- vasomotor symptoms, rapid emptying of gastric contents into the small intestine, shifts fluid into the gut and cause abdominal distention, 30 min after eating have vertigo, tachycardia, syncope, sweating, pallor, palpitations. 90 min later have excessive amount of insulin released, this dizziness, palpitations, diaphoresis and confusion – Should eat smaller amounts, take less liquid with food, high protein and fat, low CHO diet, sandostatin may be given and pectin with food – (Stomach doesn’t know the stomach is smaller after surgerystomach thinks there is too much sugar (high carb or high sugar) and the pancreas releases too much insluin… pt goes into hypoglycemia… diaphoretic, cold, clammy, tachycardic Postop Care of GI surgery • Reflux gastropathy- bile reflux, when pylorus is bypassed, bile in stomach and have abdominal discomfort and vomiting • Delayed gastric emptying- usually resolves in 1 week, edema at the anastomosis or adhesions may occur, hypokalemia, hypoproteinemia and hyponatremia may also cause • Afferent loop syndrome- duodenal loop is partially obstructed, pancreatic and biliary secretions fill the intestinal loop, it becomes distended painful contractions, bloating and pain 20-60 min after eating (a lot of N & V after you eat… ) Post op GI surgery • Recurrent ulceration- occurs in 5% of patients, may have ulcers at the anastomosis • Nutritional management: – Deficiencies of B12, folic acid and iron – Impaired Ca metabolism and reduced absorption of Ca and vitamin D – Shortage of intrinsic factor, r/t the resection and rapid emptying of the food – pernicious anemia- weak, anemic, atrophic glossitis- beefy shiny tongue – Give back B12 and folic acid Pernicious anemia Irritable Bowel Syndrome • Chronic GI disorder, with chronic or recurrent diarrhea, constipation, abdominal pain and bloating • Spastic colon, impairment of the motor/sensory function diarrhea alternating with constipation • Usually begin as a young adult • Stress, anxiety and familial factors may predispose patient • (from spastic colon & stress… Parasympathetic is not stimulated… gut slows down… constipation with diarrhea) IBS • Assessment: – History of bowel pattern – Manning criteria- abdominal pain relieved by defection, abdominal distention, sensation of incomplete evacuation of stool, presence of mucus with the stool (don’t have to remember this) – Pain in LLQ and cramps, may be tenderness and air in bowels – Dx- flexible sigmoidoscopy or colonoscopy if >40 – Barium enema IBS • Interventions – Diet therapy- limit caffeine, alcohol, beverages with sorbitol (artificial sweetners), take in fiber and bulk, 30-40 gm/day – Drug therapy: • Bulk forming laxatives (Metamucil) • antidiarrheals (loperamide, immodium, make sure they regulate how often… can cause severe constipation & dilated bowels if they take it too often) • anticholinergics (bentyl, to decrease GI spasms) • antidepressants (elavil) • 5-HT4 agonists(Zelnorm, stops GI tract pain & cramping) for prokinetic activity (allow to pass smoother), imitates serotonin to stimulate peristalsis – Stress management- relaxation techniques – (big problem is what they eat… need more fruits & veggies, fat is bad, need more fiber Nursing Diagnoses • Constipation r/t low residue diet and stress – What can be done to manage this? • Diarrhea r/t increased motility of intestines – How can this be corrected or treated? • What can be done to correct constipation and impaction? (better to take fiber than a laxitive) • What role may analgesics play in constipation? • (Opiods slow down gut a lot) Colorectal Cancer • 95% are adenocarcinomas, most come from adenomatous polyps • 2/3 occur in rectosigmoid region • Can metastasize through blood and lymph, liver most common site with 15-30% spread there, can also go to the lungs, brain, bones and adrenals • May form fistulas into bladder and vagina • Genetics- autosomal dominant disorder- familial adenomatous polyposis (multiple polyps) only 1%, 100% malignant, usually starting at age 20. Also, hereditary nonpolyposis colorectal cancer- autosomal dominant, 10% of cancers, develop by age 45 • (colon cancer treated w/ chemo.. Major complication is diarrhea & bleeding… colon cancer, 3rd leading cause of death… spreads easily to liver, lungs-most common) Colorectal cancer • 75% have no known cause (diet thought to have a lot to do w/ it) • Age is a risk factor • Dietary- decreased bowel emptying time, foods with carcinogens- red meat, fatty food, fried meats and fish, concentrated sweets • High fat diet increases bile acid secretion and anaerobic bacteria • Irritable bowel diseases can make you more prone to colorectal cancer • Third most common malignancy Colorectal cancer • Manifestations: – Rectal bleeding, anemia and change in stool – Gas pains, cramping or incomplete evacuation – Hematochezia- bright red blood when in rectum – Tumors can grow large when in upper abdomen, mostly liquid stool, more pain when in lower – Tests- stool for occult blood, CEA, barium enema, CT of abdomen – Colonoscopy or sigmoidoscopy Colorectal cancer • Nursing Diagnoses- Name 4 diagnoses, associated with colorectal cancer • 1. anxiety • 2. anticipatory grieving • 3. altered elimination, pain, • 4. impaired nutrition • What would be the expected outcomes? • (“this is the one that will be altered elimination & impaired nutrition”) Colorectal cancer • Nonsurgical management: – Duke’s staging classification • A- tumor has penetrated into, but not through the bowel wall • B- tumor has penetrated through the bowel wall • C-tumor has penetrated through the bowel wall and there is lymph node involvement • D- tumor has metastasized to distant sites • Radiation therapy (problem is it can’t be localized to gut… often have problems w/ other areas, will change normal cells & make them cancerous… leukemia later) • Drug therapy- chemotherapy IV 5-FU and leucovorin, side effects are diarrhea, mucositis, leucopenia and mouth ulcers (stomatitis, affect, mouth all GI, diarrhea, N & V & bone marrow suppression) – Eloxatin, Camptosar, Avastin (closes off blood vessles from tumor… finds rapidly growing cells & shuts off their blood supply) are also being used, along with monoclonal antibodiescetuximab Colorectal cancer • Surgical management: – Colon resection- removal of tumor and lymph nodes – Colectomy- colon removal – Abdominal perineal resection (A & P)- removes sigmoid colon, rectum and anus, colostomy is performed (colostomy & superpubic cath for life… very invasive procedure) – Colostomies may be ascending, descending, sigmoid, transverse or double barreled (if majority of colon has to be taken out..) – Stool returned depends on the site of the colostomy Colostomy Colorectal cancer • Postoperative Care: – Colostomy management • What types of nursing diagnoses may accompany this procedure? • How should the stoma appear? • Report any bleeding, breakdown of the sutures from the wall and signs of ischemia or necrosis – Wound care management- JP drains, monitor for infection – Fluid volume deficit and electrolyte imbalance – (empty bag when 1/3 to ½ full, keep it dry, w/ descending colostomy they can put a cap on it & don’t have to wear a bag all the time) Colorectal cancer • Teaching: – Colostomy care- what kinds of things should be covered? (change bag every 7 days) – Dietary measures to control stool and gas, what would they be? (no beer, broccoli, gas forming foods) – Psychological adjustment to the colostomy, what diagnosis relates to this? – Grief and family coping- what resources may be needed? – Genetic testing if familial type Intestinal Obstruction • Partial or complete • Mechanical- bowel is physically obstructed by adhesions, tumors (food or adhesions… ) • Nonmechanical- paralytic ileus or adynamic ileus, neuromuscular distrubance- slow movement or backup (could be from anesthesia or narcotics) • Contents accumulate at or above the obstruction distention, peristalsis increases to aid movement, stimulates more secretions more distention edema of the bowel, increased capillary permeability • (metabolic alkalosis, can die from shock… too much can can make you acidotic … stomach pH) Intestinal Obstruction • Plasma leaks into the peritoneal cavity and trapped fluid decreases the absorption of fluid and electrolytes into the vascular space reduced blood volume and electrolyte imbalances, can hypovolemic shock • Can also lead to metabolic alkalosis if high and there is a loss of gastric acid, if low, metabolic acidosis occurs with the loss of alkaline fluids • Bacterial peritonitis and septic shock can also occur from the release of endotoxins Intestinal Obstruction • Adhesions account for 45-60%, r/t scar tissue • Intussusception- telescoping bowel (slides inside itself) and volvulus- twisting of the bowel • Paralytic ileus (usually from meds or surgery)decreased peristalsis from trauma, toxin or autonomic, can result from surgery, MI’s, rib fracture, pneumonia, peritonitis and vascular insufficiency from heart failure or shock Intestinal Obstruction • Assessment: – History of symptoms and occurrence – Abdominal pain and cramping – Obstipation, vomiting with brown and foul smelling – Borborygni above the obstruction, then absent – Abdominal distention and tympanic abdomen – Abdominal films and CT of abdomen – WBC elevated in some cases Intestinal Obstruction • Nonsurgical management: – NGT to decompress to LCS (remove contents) – Nasointestinal tubes- Miller-Abbott, mercury balloons and migrate down the intestine by peristalsis, don’t irrigate with fluid- it will increase edema at the obstruction – Fluid and electrolyte replacement- NPO, give NSS or LR, replace K (always replace K) – Pain control- not normally given, opioids mask pain and peritonitis – Antibiotics if suspect perforation • Surgical management: – Exploratory laparotomy Case Study • 24 year old female admitted with frequent bloody diarrhea stools, weight loss and anemia. • What do you suspect? Colitis, crones disease • What labwork should you do? CBC, platelet, chemistry K & Mg) • What treatment may be needed? (diet, meds to decrease inflammation… related to some process that has cause the bowel to swell… autoimmune… allergic reaction in the gut) Case Study • Your patient tells you that the diarrhea has been occurring for months. • How do you differentiate between U.C. and Crohn’s disease? • Colitis is the colon, crone’s disease can be anywhere in the bowel… • ulcerative colitis is the sloughing of the inner layer… lots of bleeding & diarrhea • Pt w/ crones disease: more complications: invades all 3 or 4 layers of the gut… bouts of constipation w/ diarrhea…, can have fistula into rectum & bladder… more complications than colitis • What may be her treatment options? Surgery to resect & possibly ostomy Case Study • How do you help your patient decide about a colostomy? Pt. education • If she does want a colostomy, what type of teaching needs to be done? Chronic Inflammatory Bowel Disease • Ulcerative Colitis and Crohn’s • Ulcerative Colitis: – Remissions and exacerbations – Loose stools with blood and mucous 10-20/day – Poor absorption of nutrients and thickening of the colon wall – Abdominal distention and cramping – Complications are: hemorrhage, perforation, fistulas and nutritional deficiencies – May be familial tendency, inflammation r/t response to normal flora Chronic Inflammatory Bowel Disease • Crohn’s disease – Terminal ileum, patching involvement through all layers of the bowel – Deep fissures and ulcers occur – 5-8 loose stools/day, rarely bloody – Complications are: • Fistulas (biggest problem), nutritional deficiencies – Cause is thought to be mycobacterium paratuberculosis, genetic predisposition Ulcerative Colitis • Manifestations: – Abdominal pain, bloody diarrhea, tenesmusuncontrolled straining – Dx- barium enema • Nursing Diagnoses: – Diarrhea r/t inflammation of the bowel – Acute and chronic pain – Imbalance nutrition: less than body requirements – Disturbed body image Ulcerative Colitis • Diarrhea management– Drugs- salicylate compounds- Sulfasalazine (Azulfidine) inhibits prostaglandins to reduce inflammation, also use Asacol, Pentasa – Corticosteroids- Prednisone to decrease edema – Immunosuppressive- cyclosporine – Antidiarrheals – Monoclonal antibody- Remicade neutralizes the activity of tumor necrosis factor and prevents toxic megacolon (gut stops & fills up w/ toxins… can kill you w/in matter of days) Ulcerative Colitis • Diet therapy: – NPO at first, then TPN, may have low fiber or low residue, what foods would be included? (salad, raw veggies…) • Surgical management: – Total Proctocolectomy with permanent Ileostomy – Total colectomy with a continent ileostomy – Total colectomy with ileoanal anastomosis and ileoanal reservoir or pouch • Postop- teaching for ostomy, pain control and monitoring for GI bleeding and fluid volume deficit • A Colostomy is when only part of the large intestine is removed whereas an Ileostomy involves the removal of the whole of the large intestine and often the rectum as well. The distinguishing feature between a colostomy and an ileostomy is that in a colostomy, the stoma is made out of the large bowel and the stoma is therefore a little bigger than for an ileostomy where the stoma is made from the small intestine. Both colostomies and ileostomies can either be permanent or temporary. A Urostomy is when the bladder is bypassed or removed • Historically, the standard operation for ulcerative colitis has been removal of the entire colon, rectum, and anus. This operation is called a proctocolectomy (Illustration A) and may be performed in one or more stages. It cures the disease and removes all risk of developing cancer in the colon or rectum. However, this operation requires creation of a Brooke ileostomy (bringing the end of the remaining bowel through the abdomen wall, Illustration B) and chronic use of an appliance on the abdominal wall to collect waste from the bowel Crohn’s Disease • Aggravated by bacterial infection, inflammation and smoking • History of fever, abdominal pain and loose stools, weight loss • Steatorrhea is common- fatty stools • Fistulas may occur between bladder and vagina • Drug therapy- same as UC, except may take metronidazole (Flagyl for anaerobic bacteria in gut) if fistulas and imuran as an immunosuppressant • Diet therapy- may be on TPN, supplements like ensure, vivonex Crohn’s Disease • Monitor for fistulas- infections, skin problems, malnutrition, fluid and electrolyte imbalances • Fluid and electrolyte therapy- what would this entail? • Name one antidiarrheal. • Surgical management: – Bowel resections – Fistula repairs – Ileostomies may also be required to rest the bowel or repair damaged areas.