Alteration in Hematologic Function

Alteration in Hematologic Function
Lecture 7
1
White blood cells
Platelets
Introduction
Artery
Red blood cells
2
Physical Characteristics of Blood
• Heavier, thicker, and 3-4 more viscous than water
• 38 o C (100.4
o F)
• pH : 7.35 – 7.45
• 4-6 liters in an adult.
• Varies with electrolyte concentration and amount of adipose tissue
3
Components of the Blood
• Blood:
– Plasma
• water, albumin, electrolytes, clotting factors
– Cellular Components
• RBCs, WBCs, Platelets
• All formed in the red bone marrow (after birth)
– In utero- spleen, thymus, liver
• lymphatic system regulates maturation
Blood Volume
• Blood volume is about 8% of body weight.
• 1 kg of blood ≈ 1 L of blood
• 70 kg X 0.08 = 5.6 Kg = 5.6 L
• 45 % is formed elements
• 55% plasma
5
Blood Functions
1. Deliver O2
2. Remove metabolic wastes
3. Maintain temperature, pH, and fluid volume
4. Protection from blood loss- platelets
5. Prevent infection- antibodies and WBC
6. Transport hormones
6
Blood Percentages
• 55 % plasma
– Plasma is the straw-colored liquid in which the blood cells are suspended.
• 45 % formed elements
– Red blood cells (Erythrocytes)
– White blood cells (leukocytes)
– Platelets (thrombocytes)
7
Buffy coat-
<1%
Plasma-
55%
Formed elements-
45%
8
9
Plasma
• Plasma consists of:
– 90% water.
– 10 % solutes: albumin, electrolytes and proteins.
– Proteins consist of clotting factors, globulins, circulating antibodies and fibrinogen.
10
Erythrocytes
• RBCs
– carry hemoglobin which is attached to oxygenprovides O2 to the tissues
– life span 120 days
– manufacture regulated by erythropoetin
– Normal Hematocrit- 35-45%
– Normal Hemoglobin- 12-16 grams
• Hematopoiesis- production of RBC.
• Polycethemia: increase the number of RBC
RBC’s
• The bones are continually producing new cells.
12
RBC breakdown
• Healthy RBC’s live about 120 days; we break down about 174 million per minute
• RBC’s are removed from circulation by the liver and spleen
• Broken down into heme and globin portions
• Globin is broken down into amino acids
• Iron is removed from heme and stored or recycled
• Heme is broken down into biliverdin and then into bilirubin
13
RBC breakdown
• Usually eliminated in bile.
• To produce more RBC’s, the body needs sufficient iron and amino acids as well as the vitamins folate (folic acid) and vitamin B
12
• Erythropoietin is a hormone produced by the
kidneys in response to low blood oxygen levels; signals bone marrow to increase RBC production.
14
Leukocytes: White Blood Cells
• The battling blood cells.
• The white blood cells are continually on the look out for signs of disease.
• They are five types
• Leukopenia: decrease NO of WBC
• When a germ appears the WBC will:
– Produce protective antibodies.
– Surround it and devour the bacteria.
15
WBC’s
• WBC life span is from a few days to a few weeks.
• WBC’s will increase when fighting infection.
16
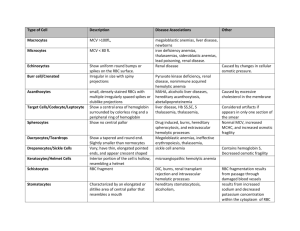
Type
Neutrophil
Eosinophil
Basophils
Monocyte
Lymphocyte
WBC
Function
Phagocytosis
Allergic reaction
Inflammatory reactions
Phagocytosis
B , T cell
Value
32-72%
2.4 – 4.8%
1%
3.5% - 13.4
13.5 – 52.8%
17
Platelets
• Platelets are irregularlyshaped, colorless bodies that are present in blood.
• Their sticky surface lets them form clots to stop bleeding.
• Thrombocytopenia
18
Normal value in children
Type
RBC (10 6 / microl)
Hematocrit
Hemoglobin
WBC (10 3 / microl)
Platelats (10 3 / microl)
New born
3.4 – 5.5
37.4 - 56.1
12.7 -18.6
6.8 – 14.3
165 -350
2 years
4- 4.9
31.7- 37.7
10.5 – 12.7
5.3 – 11.5
200 - 400
19
Pediatric differences
• At Second week = production of RBC
• 20 week production in liver.
• Bone marrow production occur at every bone.
• Fetal hemoglobin has high affinity for oxygen.
• Blood volume: 80 ml/ kg of body wt.
• High level of erythropoietin .
• Platelet lower than older : requires Vitamin K
20
Diagnostic Procedure
Test
The complete blood count (CBC)
Purpose
Help diagnose various conditions, such as anemia, infection, inflammation, bleeding disorder or leukemia
Clotting indices
Iron indices
Vit B12
G6PD
Example
Wbc
RBC
Platelet
Clotting disorders
To detect iron deficiency anemia
Potential cause of anemia
Genitics cause of anemia
PT, PTT and ACT
Serum iron, serum ferritin
B12
G6PD
21
Problems of Erythrocyte Production
• Anemia – reduction of RBC volume or Hgb concentration below normal
Causes of Anemia
•
•
•
•
Nutritional deficiency – iron, folate, B12
Increased destruction of RBCs – sickle cell anemia
Impaired or decreased rate of production – aplastic anemia
Excessive blood loss - hemophilia
Iron deficiency Anemia
• Is the most common type and the most common nutritional deficiency in children. It effects:
• 3% > 2years
• 6-18% of toddler
• 9-11% adolescent female.
• 1% adolescent male.
24
Iron Deficiency Anemia
•
•
Causes
- inadequate supply of iron
- impaired absorption
- blood loss
- excessive demands for iron req’d for growth
- inability for form Hgb
Most children need to receive 8-10 mg of iron per day. Breastfed babies need less, because iron is absorbed 3 times better.
Abnormal Laboratory Values
• Hemoglobin levels less than 8 g/dL
• Decreased levels of Serum Iron or Total Iron
Binding or Serum Ferritin
• Microcytic and hypochromic red blood cells
26
Clinical Manifestations
• very pale whites of eyes
• Brittle nails
• Decreased appetite (especially in children)
• Fatigue
• Headache
• Irritability
• Pale skin color (pallor)
• Shortness of breath
• Unusual food cravings (called pica)
• Weakness
27
Treatment
• Treatment involves iron supplements (ferrous sulfate), which are taken by mouth.
– The iron is best absorbed on an empty stomach, but many people need to take the supplements with food to avoid stomach upset. Another way to increase iron absorption is to take it together with vitamin C.
• Milk and antacids can interfere with iron absorption.
• Iron-rich foods include meats (especially liver), fish, poultry, egg yolks, legumes (peas and beans), and wholegrain bread.
• Screening for anemia is recommended at 9-12 months, 15-
18 m, and again at adolescent.
• Ferrous sulfate medication.
28
Nursing diagnosis
• Imbalance nutrition less than body requirements related to dietary intake.
• Ineffective tissue perfusion related lack of oxygen.
• Activity intolerance related to decrease oxygen carrying capacity.
• Risk of delayed growth and development related to decrease tissue perfusion.
29
Implementation
• Dietary management.
• Teach family and child about food that rich in iron and vitamin C.
• The infants over 6 month should have a diet include breast milk or iron fortified formula.
• Oral iron preparation
• explain laboratory testing.
30
Sickle Cell Anemia (SCA)
Sickle red blood cells become hard and irregularly shaped
(resembling a sickle)
Become clogged in the small blood vessels and therefore do not deliver oxygen to the tissues.
Lack of tissue oxygenation can cause excruciating pain, damage to body organs and even death.
31
Normal and Sickled Red Blood Cells in Blood Vessels
Figure B shows abnormal, sickled red blood cells clumping and blocking the blood flow in a blood vessel. The inset image shows a cross-section of a sickled red blood cell with abnormal strands of hemoglobin.
Figure A shows normal red blood cells flowing freely in a blood vessel. The inset image shows a cross-section of a normal red blood cell with normal hemoglobin.
Source from http://www.nhlbi.nih.gov/health/dci/Diseases/Sca/SCA_WhatIs.html
32
Sickle Cell Anemia (SCA)
Red blood cells (RBC)
Contain a special protein called haemoglobin (Hb)
Hb is the component that carries oxygen from the lungs to all parts of the body.
Most people have only hemoglobin type – Hb A within RBC
(normal genotype: Hb AA).
Glutamine is substituted for valine
Sickle Cell: HbS
S similar to A, but one structural change
Other types: HbC, HbD, and HbE
33
Pathopysiology -HbS
• When sickle hemoglobin (HbS) gives up its oxygen to the tissues, HbS sticks together
– Forms long rods form inside RBC
– RBC become rigid, inflexible, and sickle-shaped
– Unable to squeeze through small blood vessels, instead blocks small blood vessels
– Less oxygen to tissues of body
• RBCs containing HbS have a shorter lifespan approximately 20 days
– Normally 120 days
34
Pathophysiology
- vaso-occlusion from sickled RBCs
- increased RBC destruction
- splenic congestion and enlargement
- hepatomegaly, liver failure
- renal ischemia, hematuria
- osteoporosis, lordosis, kyphosis
- cardiomegaly, heart failure, stroke
Whaley & Wong Text
36
Body Systems Affected by SS
• Brain: CVA – paralysis - death
• Eyes: retinopathy – blindness
• Lungs: pneumonia
• Abdomen: pain, hepatomegaly, splenomegaly (medical emergency due to possible rupture
• Skeletal: joint pain, bone pain – osteomyelitis
• Skin: chronic ulcers – poor wound healing
37
Medical Complications
1. pain episodes
2. strokes
3. increased infections
4. leg ulcers
5. bone damage
6. yellow eyes or jaundice
7. early gallstones
8. lung blockage
9. kidney damage and loss of body water in urine
10. painful erections in men
(priapism)
11. blood blockage in the spleen or liver (sequestration)
12. eye damage
13. low red blood cell counts
(anemia)
14. delayed growth
38
Serious Complications: PAIN
Recurrent Pain Episodes
Occur at any age but appear to be particularly frequent during late adolescence and early adult life
Unpredictable
Red Blood Cells get stuck in the small veins and prevent normal blood flow
Characterized by sever pain in the back, chest, abdomen, extremities, and head
Highly disruptive to life
Most common reasons for individuals to seek health care
39
Alleviating Pain
Warmth: increases blood flow
Massaging and rubbing
Heat from hot water bottles and deep heat creams
Bandaging to support the painful region
Resting the body
Cognitive Behavioral Therapy
Getting the sufferer to relax
deep breathing exercises
distracting the attention
by other psychological methods.
Pain-killing medicines (analgesics): paracetamol, codeine nonsteroidal anti-inflammatory, morphine if necessary
40
Daily Preventative Measures
1. Taking the folic acid (folate) daily to help make new red cells
2. Daily penicillin until age six to prevent serious infection
3. Drinking plenty of water daily (8-10 glasses for adults)
4. Avoiding too hot or too cold temperatures
5. Avoiding over exertion and stress
6. Getting plenty of rest
7. Getting regular check-ups from knowledgeable health care providers
41
Treatments
Effective treatments are available to help relieve the symptoms and complications of sickle cell anemia, but in most cases there’s no cure
.
The goal is to relieve the pain; prevent infections, eye damage, strokes and control complications if they occur.
Pain medicine: acetaminophen, nonsteroidal antiinflammatory drugs (NSAIDs), and narcotics such as meperidine, morphine, oxycodone, and etc.
Heating pads
Folic Acid
Blood Transfusions
42
What Is Thalassemia?
• Thalassemia is an inherited blood disorder that causes mild or severe anemia. The anemia is due to reduced hemoglobin and fewer red blood cells than normal .
Hemoglobin is the protein in red blood cells that carries oxygen to all parts of the body.
43
RBC Characteristics
– Microcytosis = small in size
– Hypochromia = decrease hemoglobin
– Poikilocytosis = abnormal shape
44
The two main types of thalassemia
• alpha and beta, are named for the two protein chains that make up normal hemoglobin. The genes for each type of thalassemia are passed from parents to their children. Alpha and beta thalassemias have both mild and severe forms.
45
The two main types of thalassemia
• Hemoglobin includes two kinds of protein chains called alpha globin chains and beta globin chains.
• If the problem is with the alpha globin part of hemoglobin, the disorder is alpha thalassemia.
If the problem is with the beta globin part, it is called beta thalassemia.
• There are both mild and severe forms of alpha and beta thalassemia. Severe beta thalassemia is often called Cooley ’ s anemia .
46
47
What Are the Signs and Symptoms of
Thalassemia?
• The symptoms of thalassemia depend on the type and severity of the disease. Symptoms occur when not enough oxygen gets to various parts of the body due to low hemoglobin and a shortage of red blood cells in the blood
(anemia).
48
How Is Thalassemia Diagnosed?
1. Thalassemia is diagnosed using blood tests, including a complete blood count (CBC) and special hemoglobin studies.
2. Hemoglobin studies measure the types of hemoglobin in a blood sample.
Poor prognosis / death within 1 st year due to septicemia or heart failure.
49
Treatment
• Severe thalassemia is treated with frequent blood transfusions and iron chelation therapy to remove excess iron that builds up in the body from the transfusions. The medicine deferoxamine
• Bone marrow or stem cell transplants have cured thalassemia in some children, but this treatment is not available for most people with thalassemia.
• Researchers are studying new treatments, including ways to cure thalassemia through stem cell and gene therapies.
50
Nursing diagnosis
1. Imbalance nutrition less than the needs associated with nausea, vomiting, anorexia.
2. Activity intolerance related to reduced oxygen supply to the central nervous system.
3. Bleeding
4. Risk of infection associated with invasive measures: a reduction in immunological
51
Nursing interventions
• Monitor nutritional intake and output
• Monitor weight gain
• Help clients and families identify and select foods that contain calories and protein in accordance with a programmed diet.
• Serve food in warm and attractive
• Collaboration with a dietitian to determine the proper diet as well as physicians in the provision of vitamins.
52
Nursing interventions
• Observation of general condition Clients
• Monitor laboratory results (number of platelets)
• Observation of signs of bleeding
• Collaborative provision platelet transfusion
53
Bleeding Disorders
• Three types Hemophilia: males only
– Type A most common – factor VIII deficiency
– Type B - lack of factor IX
– Type C – lack of factor XI
Von Willebrand Disease – 1% of population – men or women – prolonged bleeding time
54
Hemophilia Type A
• Hemophilia type A is the deficiency of clotting factor VIII.
– A serious blood disorder
– Affects 1 in 10,000 males in the US
– Autoimmune disorder with lowered level of clotting factor
– All races and socio economic groups affected equally
55
Hemophilia
• Hemophilia is a sex-linked hereditary bleeding disorder
• Transmitted on the X chromosome
• Female is the carrier
• Women do not suffer from the disease itself
56
Goals of Care
• Goals of care:
– Provide factor VIII (IX) to aid blood in clotting.
– To decrease transmission of infectious agents in blood products; hepatitis & AIDS.
– Future: gene therapy to increase production of clotting factor.
57
Symptoms
• Circumcision may produce prolonged bleeding.
• As child matures and becomes more active the incidence of bleeding due to trauma increases
58
Symptoms
• May be mild, moderate or severe
• Bleeding into joint spaces, hemarthrosis
• Most dangerous bleed would be intracranial.
59
Diagnosis
• Presenting symptoms
• Prolonged activated aPTT and decreased levels of factor VIII or IX.
• Genetic testing to identify carriers
60
Treatment
• Products used to treat hemophilia are:
– Fresh frozen plasma which are from single blood donors and require special freezing.
– Second generation of factor VIII are made with animal or human proteins.
61
Nursing Diagnoses
• Risk for injury
• Pain with bleed especially into a joint
• Impaired physical mobility
• Knowledge deficit regarding disease and management of disease
62
Nursing interventions
• No rectal temps.
• Replace the factor as ordered by physician.
• Manage pain utilizing analgesics as ordered.
• Maintaining joint integrity during acute phase: immobilization, elevation, ice.
• Physical therapy to prevent flexion contraction and to strengthen muscles and joints.
• Provide opportunities for normal growth and development.
63
Nursing interventions
•
•
•
• Prevent bleeding
Recognize and control bleeding (RICE)
- Rest
- Ice
- Compression
- Elevation
Prevent crippling effects of bleeding
Client education
Teaching
• Avoid aspirin which prolongs bleeding time in people with normal levels of factor VIII.
• A fresh bleeding episode can start if the clot becomes dislodged.
• Natural reactions in the body cause the clot that is no longer needed to “break down. This process occurs 5 days after the initial clot is formed.
65
Family Education
• Medic-Alert bracelet
• Injury prevention appropriate for age
• Signs and symptoms of internal bleeding or hemarthrosis
• Dental checkups
• Medication administration
66