Clinical Care - Chinook Primary Care Network
advertisement

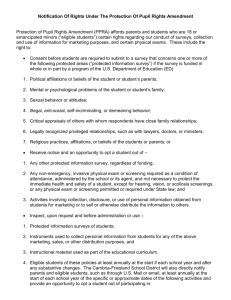
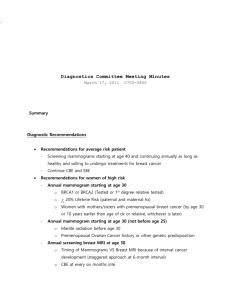
Focusing on Key Clinical Areas for Improvements: 10 Selected Topics What to do? Mike Davies, MD FACP Why are Toyotas more reliable than Fords? Why are Toyotas more reliable than Fords? Components of Excellent Clinical Care Satisfaction Access – no waiting Courtesy – especially in making appointments Technical Quality Access Prevention Chronic Disease Care Specific care often invisible to patients Cost Goal Championship teams: “Nothing is more important than the goal” What is the goal? We all agree on this: Our goal is to provide excellent clinical care Why Clinical Care Measures? Six Sigma – 99.99966% performance level Creating Intellectual Capital Five Sigma – 99.977% performance level Competitive Breakthrough · · Four Sigma – 99.370% performance level Continuous Improvement · Three Sigma – 93.32% performance level Compliance · Two Sigma – 69.2% performance level Capability · One Sigma – 31% performance level Control < One Sigma - < 31% performance level Containment · Six Sigma = 3.4 per million units Five Sigma = 230 per million units Four Sigma = 6,210 per million units Three Sigma = 66,800 per million units Two Sigma = 308,000 per million units One Sigma = 690,000 per million units Clinical Care: 10 Topics Prevention Flu Vaccination Pneumonia Vaccination Breast Cancer Cervical Cancer Colon Cancer Chronic Disease HTN CHF DM Lipids Depression Considerations for picking focus Screen Assess Treatment Outcomes Vaccine Cuts Pneumonia Risk in HighRisk Patients Archives of Internal Medicine 1999;159:2437-2442 2-year retrospective study involving ~1,900 elderly patients with chronic lung disease. ~2/3 had been vaccinated against pneumonia or influenza. Pneumococcal vaccination was associated with 43% reduction in hospitalization for pneumonia or influenza and 29% reduction in overall risk of death. Patients receiving both vaccines had a 72% reduction in hospitalizations and an 82% reduction in death. Pneumococcal vaccination was associated with an average cost savings of $294 per vaccine recipient over the 2-year period. Under-use of influenza vaccine increased use of health services for community acquired pneumonia Canadian Journal of Public Health, Sept/Oct 2003 2-year retrospective analysis of regional rates of influenza immunization coverage, cost & mortality for community acquired pneumonia in Alberta Influenza coverage rate 30-80% (mean 70%,n=298,473) Coverage rate highest in metropolitan areas, lower in rural, lowest in remote areas Regions with lower coverage had higher rates of pneumonia requiring hospitalization Immunization cost (approx $10) less than per capita cost for physician and/or hospital care for pneumonia Influenza Vaccine Canadian Immunization Guide 2002, 6th ed. Healthy infants and children age 6-23 months All adults ≥ 65 Residents of nursing homes or chronic care facilities People capable of transmitting to those at high risk Pregnant women in high risk groups Administer between September and February (Optimal is Oct/Nov) Prevention: Flu Vaccination National Advisory Committee on Immunization, 2005 Adults & children with chronic cardiac or pulmonary disorders Adults & children with metabolic diseases, cancer, immunodeficiency, immunosuppression, renal disease, anemia, hemoglobinopathy Adults & children with any condition compromising respiratory function or that may increase risk of aspiration Children and adolescents on long-term ASA Flu Vaccination Goal > 90% of eligible people vaccinated Numerator: eligible patients vaccinated Denominator: all eligible patients Note: Measure of “Treat” step Prevention: Pneumococcal Vaccination Alberta Health & Wellness, 2005 Children ≤ 18 months Children 24-59 months: aboriginal children, children with sickle cell disease, asplenia, HIV, chronic illness or immune compromising condition Children and adolescents with chronic conditions if not previously immunized Pneumococcal Vaccination All adults > 65 Adults < 65 with chronic illness Residents of nursing homes or chronic care facilities Administer anytime during the year Pneumococcal Vaccination Goal > 87% Eligible patients Vaccinated Numerator: Eligible patients vaccinated Denominator: All eligible patients Note: Measure at “treat” step Prevention: Breast Cancer Alberta Cancer Board, 2005 Most commonly diagnosed non-skin malignancy in Alberta Second only to lung cancer as cause of cancer-related death Risk for Development of Breast Cancer Over Next 10 Years by Age 4.00% 3.00% 2.00% 1.00% 0.00% 2.8% 0.4% 30-39 3.6% 1.5% 40-49 50-59 60-69 Breast Cancer Alberta Cancer Board, 2005 Mammography is the best way to detect breast cancer (finds cancer 1-4 years before a palpable lump) Regular mammography screening can ↓ breast cancer deaths by up to 30% in women 50-69 y of age If a typical panel has 1000 women; and 500 are over age 50, then about 15 will develop breast cancer in next 10 years – perhaps 1 per year. Breast Cancer Tool What: Orders for mammogram. Standing? Protocol? Who: Eligible panel women (age 50-69y) When: Every 1-2 years starting at age 50 Why: Early detection of cancer Where: Nurse check in process Breast Cancer Clinical Care Goal >95% of Eligible patients screened Numerator: All Denominator Pts with mammogram in chart every 1-2 years Denominator: All women eligible for Mammogram Note: Measure at “screen” step Cervical Cancer Alberta Cancer Board, 2005 10th leading cause of cancer death. Incidence in Alberta 11/100,000/year (2001) Preventable Alberta Cancer Board recommends screening women 18-69 years of age whom are sexually active and have a cervix Stop screening at age 69 if prior screening tests normal Don’t screen patients with life expectancy of less than 6 months Cervical Cancer Who? Eligible panel women What? Pap Smear annually Where? Clinic Appt When? Annually Why? Early detection of cervical cancer Cervical Cancer Goal > 90% Screened Numerator: Eligible patients screened Denominator: All eligible patients Note: screen step measure Colon Cancer Alberta Cancer Board, 2005 2nd most common invasive cancer 2nd leading cause of cancer death Person age 50 has 5% lifetime risk of diagnosis and 2.5% chance of dying from it Strong recommendation that men and women over 50 are screened Any screening method is better than no screening Colon Cancer Screening Options Canadian Association of Gastroenterology & Canadian Digestive Health Foundation, 2004 FOBT every 2 years Sigmoidoscopy every 5 years Colonoscopy every 10 years Stop screening at age 80 Colon Cancer Who? Pts. Age 50-80. What? Any of the 3 screening methods Where? Clinic education When? Every 2 years (FOBT); every 5 years (Sigmoidoscopy); every 10 years (Colonoscopy) Why? Early detection of colon cancer Colon Cancer Clinical Care Goal >95% of Eligible patients screened Numerator: All Denominator Pts with mammogram in chart every 2 years Denominator: All women eligible for Mammogram Screen measure Hypertension (Vascular Health) One of four adults has HTN 1/3 don’t know they have it Approximately ½ of adult Canadians are hypertensive by age 60 Continuous, consistent, and independent relationship of BP and heart attack, heart failure, stroke, and kidney disease The Challenge In Canada 22% of Canadians 18-70 years of age have hypertension 50% of Canadians >65 years of age have hypertension Hypertensive patients who are treated and BP controlled Hypertensive patients who are treated but BP uncontrolled 21% 22% Patients who are aware but remain untreated and BP uncontrolled 13% 43% 9% Diabetic patients who are treated and BP controlled Hypertensive patients who are unaware Joffres et al. Am J Hyper 2001;14:1099 –1105 4 Strategies for HTN Pay attention to blood pressure before it is high In people over age 50, systolic pressure is more important than diastolic Two (or more) drugs are better than one for most patients Build trusting relationships that motivate patients to be healthy HTN Who? All patients get BP reading every time by nurse What? Nurse records BP and notifies doctor if high Where? Clinic When? Every visit Why? Detect and manage HTN Hypertension Goal Good control Denominator: All patients with HTN Numerator: Those patients with both systolic and diastolic BP < 140/90 Poor Control Denominator: All patients with HTN Numerator: Those patients with either systolic or diastolic BP > 160/100 Heart Failure Common: Chronic heart failure affects 1 in 10 Canadians (over 2.3 million people) Expensive: HF accounts for more hospital admissions than any other diagnosis in patients over the age of 65. Approximately $5500 (modest) is spent on each hospitalization Lethal: approximately 2/3 of those with HF die within five years of their initial hospitalization. HF accounts for 9% of all deaths in Canada Heart Failure Patient non-compliance with physician's instructions is often a cause of re-hospitalization Self Management: Evidence indicates that patient involvement in co-managing their care can increase longevity and reduce the consumption of healthcare resources Patient Education Ensure that patients and their families understand the: Activity level Nutrition: specifics to salt and fluid restriction Discharge medications Follow-up appointment Weight monitoring What to do if symptoms worsen Heart Failure Measure Numerator: Number of patients with ejection fraction less than 40% and a diagnosis of heart failure who were on angiotensin-converting enzyme inhibitor (ACEI) and Beta blocker Denominator: Number of patients with ejection fraction less than 40 and a diagnosis of heart failure that had been treated for heart failure sometime during the previous 24 months “Treat” measure Patient Education Measure Numerator: Patients with a principal diagnosis of heart failure with complete instructions in the medical record Denominator: Patients with a principal diagnosis of heart failure “Treat” step measure Diabetes Over 6% of US population has DM. In Canada, physician-diagnosed prevalence of DM is 4.8% (1,054,100 adults) with true prevalence estimated at > 7%. Heart disease is the leading cause of diabetes-related deaths (2-4 X higher than adults without DM). Stroke risk is 2 to 4 times higher among people with diabetes. Blindness Diabetes is the leading cause of new cases of blindness among adults age 20-74. Diabetic retinopathy causes 12,000 to 24,000 new cases of blindness each year. Amputations More than 60% of nontraumatic lower-limb amputations in the United States occur among people with diabetes. Diabetes For every 1% reduction in A1C, the relative risk of developing microvascular diabetic complications (eye, kidney and nerve disease) is reduced by 40%. For every 10 mm Hg reduction in systolic blood pressure, the risk for any complication related to diabetes is reduced by 12%. Comprehensive foot care programs can reduce amputation rates by 45% to 85%. Detection and treatment of early diabetic kidney disease can reduce the development of kidney failure by 30% to 70%. Diabetes Measures Denominator = all patients with DM Numerator = BP < 130/80 (Optimal Control) “Treat” Measure BP < 140/90 (Good Control) “Treat” Measure BP > 160/100 (Poor Control) “Treat” Measure Hgb A1C > 9 or not done (poor control) “Screen” Measure LDL < 2.5mmol/L “Treat” Measure Retinal Exam Q 2 years if normal and Q 1 year if abnormal “Screen” Measure Foot Screening Yearly “Screen” Measure Lipids Background Good evidence that lipid measurement finds asymptomatic people at risk Good evidence that treatment substantially decreases the risk of CHD Benefits of screening and treatment outweighs the harms Lipids Routinely screen and treat as appropriate men > 40 and women postmenopausal or > 50 Routinely screen and treat all younger patients with risk factors Measure total cholesterol, HDL, LDL, Triglycerides Lipids: Goals Lipid Screening > 90% Numerator: Eligible patients screened Denominator: Eligible patients Depression 10% of the population suffer from a depressive disorder at some point in their lives US spends $44 B per year in direct and indirect costs related to depression 50% of patients with depression go undetected or untreated Most patients with depression don’t complete adequate care Impact of Mental Illnesses (of which Depression is the most prevalent) Causes of Disability / United States, Canada, and Western Europe, 2000 (SOURCE: World Health Organization, 2001) Mental Illnesses Alcohol and Drug Use Disorders Alzheimer’s Disease and Dementias Musculoskeletal Diseases Respiratory Diseases Cardiovascular Diseases Sense Organ Diseases Injuries (Disabling) Digestive Diseases Communicable Diseases Cancer (Malignant neoplasms) Diabetes Migraine All Other Causes of Disability 0% 4% 8% 12% 16% 20% 24% Depression Screening “During the past month, have you been bothered by feeling down, depressed, or hopeless?” “During the past month, have you been bothered by little interest or pleasure in doing things?” Depression Goals Screen > 90% Numerator: Those screened Denominator: All adults Tools for Day-To-Day Care Progress Notes Narrative Checklist Nurse Provider Electronic Chart Audit Date of Most Recent Visit: ____________________________ Age: ______________________________________________ Sex: ______________________________________________ Is Flow Sheet in Chart?: ______________________________ Has It Been Updated Within Last 12 Months?: ____________ Smoker?: __________________________________________ Tobacco Counseling?: _______________________________ Health Screening Area: Guaiac: ____________________________________________ Breast Exam: _______________________________________ Mammogram: _______________________________________ PAP/Pelvic: _________________________________________ Comments: _________________________________________ Chronic Dz Clinical Goals Diagnosis Protocol? Our Outcomes Benchmark HTN 75%<140/90 DM Hgb A1c DM Eye <12% > 9 85% 80% DM Lipids >80% LDL<120 CVD Lipids <20% LDL>100 MDD New Meds >77% >95% 92% DM Foot CHF Weight CAP - Culture Prevention Clinical Goals Prevention Flu shot Colon Ca Breast Ca Cervical Ca Pneumo. V. MDD Screen SUD Screen Tob. Counsel Protocol? Results Benchmark >90% >75% >90% >90% >87% >95% >95% >93% Firm A Medical Outcomes: Baseline Through February '03 80% 70% Goal 50% % At 60% 40% 30% All Outcomes p < .01 A1c < 7.5 LDL cholesterol <100 20% BP < 140/90 10% Month Fe b03 03 Ja n- De c02 v02 No Oc t-0 2 02 Se p- g02 Au Ju l-0 2 -02 Ju n Ma y02 r-0 2 Ap Ma r -0 2 Fe b02 02 Ja n- Ba se lin e 0% Clinical Quality Indicators Oct 01 to Sept 05 Primary Care Dx Management 90% 80% 74% 74% 70% 60% 58% 61% 63% 66% 77% 72% 69% 64% 57% 66% 70% 69% 71% 70% 66% 65% 60% 58% 59% 54% 52% 47% 50% 40% 30% 20% 10% 0% % LDL < 100 Oct to Mar FY 02 Ap to Sept FY 02 % HgbA1c < 7.5 Oct to Mar FY 03 Ap to Sept FY 03 Oct to Mar FY 04 % BP< 140/90 Ap to Sept FY 04 Oct to Mar FY 05 Ap to Sept FY 05 Results: Improvement in CRC screening 80% 60% 40% 20% ne Au g No v De c Ja n Fe b M ay Ju ne Au g Oc t No v M ar ch M ay Ju ne Au g Ju ay 0% M % complete 100% 2003-2005 CRC Screening Stage IV CRC from Charleston VAMC Tumor Registry through April 1, 2005 7 6 5 4 Stage IV 3 2 1 0 2003 2004 2005 Finally Patient Self Care is ultimate goal Good References www.guidelines.gov US Preventative Services Taskforce ahrqpubs@ahrq.gov http://pda.ahrq.gov http://www.qmo.amedd.army.mil/pguide.htm www.cancerboard.ab.ca topalbertadoctors.org www.health.gov.ab.ca