Chapter 37
advertisement

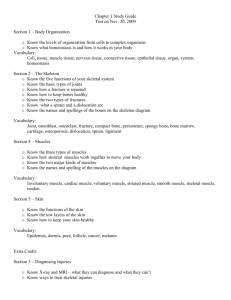
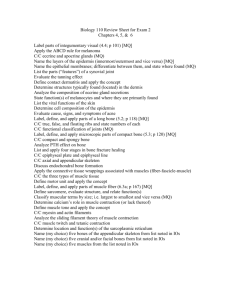
CHAPTER 37 STRUCTURAL SUPPORT AND MOVEMENT: A SUMMARY AP Biology Spring 2011 EVOLUTIONARY HERITAGE • Skeleton: structural framework that functions in maintaining body shape, supporting and protecting cells, and accepting the force of contraction that can bring about movements EVOLUTIONARY HERITAGE • Three types: • Hydrostatic Skeleton: muscle cells apply the force of contraction against a body fluid and thereby redistribute it within a confined space • Exoskeleton: rigid or flexible structures at the body surface accept applied force of contraction • Insect cuticle • Endoskeleton: internal body parts, such as bones, receive the applied force of muscle contraction INVERTEBRATE SKELETONS • Hydrostatic Skeletons: • Soft bodied animals • Many contractile cells oriented side by side, longitudinally, in body wall • Others oriented like rings around body cavity • Stiff fibers form a mesh in body wall, help prevent uncontrollable bulges when contraction makes fluid move inside gut cavity INVERTEBRATE SKELETONS • Exoskeletons: • Arthropods • Hinged exoskeleton with attachment sites for sets of muscles that move hard parts like levers • Move by combination of muscles and hydraulic pressure • Hydraulic: fluid pressure within a tube INVERTEBRATE SKELETONS • Invertebrates and Endoskeletons: • Echinoderms: endoskeleton within dermis • Ossicles: arrays of structural elements, made of tiny calcite crystals • Epidermis covers ossicles • Echinoderm = spiny-skinned • Move by combination of muscles and hydraulic pressure VERTEBRATE SKELETON • Human skeleton has 206 bones • Pectoral girdle and pelvic girdle- transfer weight to limbs • Appendicular portionpaired arms, hands, legs, feet • Axial portion- jaws, skull bones, ribs, breast bone, vertebra VERTEBRATE SKELETON • Vertebral column: bony parts offer attachment sites for paired muscles and protective canal for spinal cord • Column transmits torso’s weight to lower limbs • Backbone is curved into “S” shape to keep body’s main axis in vertical alignment • Intervertebral disks: separates bones of vertebra • Cartilaginous shock absorbers and flex points BONE STRUCTURE AND FUNCTION • Bone Tissue: bone cells and collagen fibers in a calcium-hardened organic matrix BONE STRUCTURE AND FUNCTION • 3 types of bone cells: • Osteoblasts: bone-forming cells; secrete the components of the matrix; present on outer surface and internal cavities of bones of adults • Osteocytes: osteoblasts that become imprisoned in small chambers after secreting matrix material around themselves; most common cone cells in bony tissue of adults • Osteoclasts: bone cells that break down bone tissue by secreting acids and enzymes into hardened matrix BONE STRUCTURE AND FUNCTION • 2 types of bone tissue: • Compact: resists mechanical shock, laid down as dense concentric rings around tiny canals for nerves and blood vessels • Osteocytes reside in narrow clefts between rings • Spongy: present in femur’s shaft and knobby ends, strong but doesn’t weigh much, hardened matrix is pocketed with open spaces BONE STRUCTURE AND FUNCTION • Red marrow: major site of blood cell formation, fills the spaces in spongy bone • Yellow marrow: central cavity of femur and most mature bones of adults, mostly fat, can be converted to blood cell-producing red marrow with severe blood loss BONE FORMATION AND REMODELING • First skeleton in embryos is made of cartilage • Cartilage is model • Osteoblasts infiltrate, transform cartilage to bone, narrow cavity opens BONE FORMATION AND REMODELING • Bone Remodeling: osteoblasts help form new bone tissue, which makes up for bone tissue that osteoclasts are breaking down • Bone is broken down to help maintain required blood levels of calcium and phosphorous BONE FORMATION AND REMODELING • Until humans are 24 years old, osteoblasts secreting more matrix than osteoclasts can break down, so bone mass increases • Bones become denser and stronger, later in life osteoblast activity declines, bones weaken • Osteoporosis: significant loss of bone density WHERE BONES MEET- SKELETAL JOINTS • Joints: areas of contact or near-contact between bones • Ligaments: straps of dense connective tissue at many joints, attach bone to bone • Tendons: attach bone to muscle WHERE BONES MEET- SKELETAL JOINTS • Arthritis: joint inflammation and degenerative disorders • Osteoarthritis: cartilage at freely moving joints wears away • Rheumatoid arthritis: joint membranes become inflamed, thicken, cartilage degenerates, bone deposits accumulate as a result of autoimmune response SKELETAL-MUSCULAR SYSTEM • Muscle fiber: groups fused together into one multinucleated muscle fiber • Bundles sheathed in dense connective tissue, extends past them SKELETAL-MUSCULAR SYSTEM • Attachment sites of muscles: • Act as lever system, is which a rigid rod is attached to a fixed point and moves about it • Muscles connect to bones (rigid rods) near a joint (fixed position) • When contract, transmit force that makes bones move SKELETAL-MUSCULAR SYSTEM • • • • Skeletal muscles also interact with one another Some work in pairs or groups, some work in opposition Only skeletal muscles are the functional partner of bones Human body has close to 700 skeletal muscles SKELETAL MUSCLE CONTRACTION • Long, slender muscle fibers run parallel with muscle’s long axis • Myofibrils: bundle of contractile filaments that run from one end of fiber to the other • Bands give muscle striated appearance SKELETAL MUSCLE CONTRACTION • Sarcomeres: repeated one after another along length of myofibril • Each end is anchored to its neighbor at a Z band, a dense mesh of cytoskeletal elements SKELETAL MUSCLE CONTRACTION • Actin: thin filaments, extend from Z bands toward sarcomere center • Myosin: thick filaments, starts at center of sarcomere, runs parallel with thin filaments but not all the way to the Z band SKELETAL MUSCLE CONTRACTION • Muscle fibers, myofibrils, think filaments, and thick filaments have the same orientation • Run parallel with long axis • Repetitive orientation focuses the force of contraction, so all sarcomeres in all fibers of a muscle work together to pull a bone in the same direction SLIDING FILAMENT MODEL SLIDING FILAMENT MODEL • Myosin heads move actin filaments toward sarcomere’s center by short, repetitive ATP driven strokes • Myosin filaments stay in place, actin filaments slide past them • Both Z bands pulled inward wit them, shortens sarcomere • Myosin heads latch onto binding sites along actin filaments SLIDING FILAMENT MODEL • Part of myosin head is enzymatic, catalyzes phosphate-group transfer from ATP, which is the energy that drives contraction • Myosin forms cross-bridge to actin when local concentration of calcium ions rises and a binding site for myosin’s head is exposed • Once head binds, tilts towards sarcomere’s center and actin slides along with it • When another ATP boost breaks grip on actin, myosin head reverts to resting position SLIDING FILAMENT THEORY • http://www.youtube.com/watch?v=EdHzKYDxrKc • http://www.youtube.com/watch?v=pWP1u7rRJS8 CONTRACTION • Action Potential: voltage difference of interstitial fluid and cytoplasm of a cell membrane can reverse in response to a stimulus CONTRACTION • Signals from nervous system strongly spread rapidly from stimulation site, then along T tubules (transverse tubule) • Small tubes are extensions of plasma membrane • Actin filaments in sarcomeres are attached to them • Sarcoplasmic reticulum: takes up, stores, and releases calcium ions in a controlled way CONTRACTION • Arrival of action potentials causes calcium ions to flow out of chambers • Released ions diffuse into myofibrilis and reach actin filaments • Actin binding sites for myosin heads are blocked in resting muscle fibers, calcium clears them CONTRACTION • Figure 37.17: cross-bridge binding site blocked • Proteins, tropomyosin and troponin, positioned in or near grooves at actin filament surface http://www.youtube.com/watch?v=mWPmUqRZYls CONTRACTION • Calcium levels low proteins joined so tightly that tropomyosin is forced out of groove • Moves slightly which blocks cross-bridge binding site • Calcium levels high calcium ions bind with troponin to cause shape change • Troponin now has different molecular grip on tropomyosin filament, which is free to slip back into groove • Binding site now exposed ENERGY FOR CONTRACTION • Muscle fiber has small amounts of ATP when starts contracting • Produce more by transferring one phosphate group from creatine phosphate to ADP ENERGY FOR CONTRACTION • 6x as much creatine phosphate as ATP • Supply only fuels ~15sec of contraction • After contraction, supply of creatine phosphate restored, ATP donates phosphate to creatine ENERGY FOR CONTRACTION • Prolonged moderate exercise • Aerobic respiration provides energy • First 10-15 min: Muscle fiber converts stored glycogen to glucose (starting substrate) • Next 30 min • Glucose and fatty acids sustain activity • Fatty acids become main energy source for further contraction • Lactose transposable form of energy (anaerobic pathway) TYPES OF CONTRACTIONS • Motor Unit: a motor neuron and all of the muscle fibers that are functionally connected to it • When motor neuron is stimulated, all fibers in motor unit contract • Muscle Twitch: contractile force that is generated; contraction TYPES OF CONTRACTIONS • Tetanus: • Applying a new stimulus before a response ends makes muscles twitch again • Repeatedly stimulating motor unit during short interval makes all of twitches run together • Resulting sustained contraction • Generates 3-4 times force of single twitch TYPES OF CONTRACTIONS • Muscle Tension: mechanical force exerted by a muscle on an object • Load: opposing force of muscle tension • Weight or object or gravity’s pull on muscle • Muscle tension exceeds opposing forces stimulated muscle shorten TYPES OF CONTRACTIONS • Isotonically contracting muscles: shorten and move load • Isometrically contracting muscles: develop tension as attempt to lift something that is too heavy, but they cannot shorten MUSCLE FATIGUE • When ongoing, strong stimulation keeps a muscle in a state of tetanic contraction • Muscle fatigue: decrease in muscle’s capacity to generate force, decline in tension • Needs rest to contract again • Glycogen depletion is one factor in muscle fatigue MUSCLE FATIGUE • Brief intense exercise fatigue and recover fast • Prolonged, moderate exercise fatigue slow and recover slow • Muscle cramp: abrupt involuntary, often painful contraction that resists release • Message and heat can relieve • To avoid: stretch, avoid overexertion, dehydration MUSCLE DYSTROPHIES • Muscular Dystrophies: class of genetic disorders in which muscles progressively weaken and degenerate • Duchenne muscular dystrophy children • Mutant gene on X chromosome • Myotonic muscular dystrophy adults MUSCLES, EXERCISING, AGING • Cannot make more muscle fibers • Existing ones get bigger, more active, and more resistant to fatigue • Aerobic exercise: long in duration, increase number of mitochondria in muscles and number of blood capillaries • Strength training: brief intense exercise, causes muscle fibers to thicken, stimulates enzymes necessary for glycolysis MUSCLES, EXERCISING, AGING • • • • • Aging: number and size of muscle fibers decline Tendons (muscle to bone) stiffen, more likely to tear Muscle mass does not increase much Aerobic exercise improves blood circulation Modest strength training can slow loss of muscle tissue