MRRN Sept 14 2011
advertisement

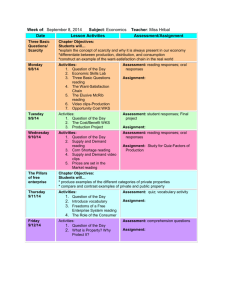
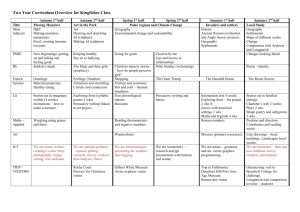
MRRN September 14, 2011 CMU College of Medicine • Starting a new medical school • Accreditation – LCME • Strategic Planning • Educational Program design and development • Fund raising • Organizational change – the university • Getting the community on board • Managing politics – competing health systems, etc. • Recruiting faculty • And, lots more… Medicine’s Challenges (Macy) • Accelerating pace of scientific discovery • Calls for more public accountability • The economy • Rising cost of health care • Shortfalls in health care quality • Racial/ethnic disparities • Rising burden of chronic illness/disability • Aging population Challenges/needs • Re-define foundation sciences of medicine • Psychology, social science, quality improvement, decision science, epidemiology, EBM, CQI… • Facilitate problem solving and self-directed learning skills • Certification and maintenance of certification • Assure students experience continuity of care • Students need skills in continuous improvement and safety Challenges/needs • Increase emphasis on community-based education rather than the hospital • Prepare students to work as team members (inter-professional teams) • Increase knowledge of public health and nonbiological determinants of health and disease • Foster long-term relationships between students and faculty • Develop teaching and mentoring skills of faculty Needs Assessment - CMED • LCME • USMLE • AHRQ, HHS, CMS,IHI, IOM, etc. – care quality, safety, • • • • • • patient experience, control costs, etc. Other curricula (content, models, organization) AAMC – HHMI- competencies AAMC Training Physicians white papers ACGME/ABMS – competencies, MOC, etc. Local disease/health data Literature of medical education IHI Goal: Crossing the Quality Chasm • Care that is: • Safe, Effective, Patient-Centered, Timely, Efficient, Equitable • Evidence-Based • Personal • Holistic, and CARING Competencies – ACGME-plus 1. Patient care Consider procedural skills as a competency? 2. 3. 4. 5. 6. 7. Medical knowledge Communication & interviewing Professionalism Practice-based learning & improvement Systems-based practice Community and population health Future Practice of Medicine • Patient-centered care • Patients as individuals and member of population to be cared for supporting health assessment, patient outreach, illness prevention strategies • Systematic assessment and improvement of quality indicators for physicians, hospitals, systems, patient populations • Coordinates and delivers care through organized systems • Places value on cost-effective care • Helps address constraints on health care resources Helps to define physician skill set for future Local needs/challenges • Physician shortage current – perhaps 1,000 • By 2020 – 6,000 • Closing the gap and the ongoing loss of physicians to their communities through retirement, etc. • Distributional issue • Recruiting to rural environment • Retaining physicians in rural environment • Who will come, who will stay? • Pipelines-AHEC • Specialty distributional issue 11 Complexity of undertaking… What is unique about CMED? • Location • Mission, vision • Curriculum Mission • Prepare exceptional physicians • Improving access to individualized, essential care (health care delivery) • Focus in rural and medically underserved regions of Michigan • Rural/small community focus • Differentiated skill set • Generalist focus: (FM,IM, Peds, Gen Surg, Ob/Gyn, Psych, EM, PM&R) Vision • Excellence in instruction/active learning • Team-based learning experiences • Early patient contact • Student-centered environment/program • Patient-Centered care • Residencies (new, distributed) • Community-based, 11 affiliations thus far Feedback & Revise Evaluate Instruction (Summative) Develop Objectives Develop Assessment s Design Instruction Assess Needs Manage Instruction Iterative Process Implement Instruction Revise Instruction Evaluate Instruction (Formative) Develop Instruction Pilot Instruction LMCE: Integrated MD Curriculum Formal Knowledge/ Courses Clinical Experience Inquiry, Discovery, Innovation Year I Year II Year III Year IV Course Structure YEAR 1 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 MED 630: FOUNDATIONAL SCIENCES OF MEDICINE (21 wks) MED 600: SOCIETY AND COMMUNITY MEDICINE MED 610: ESSENTIALS OF CLINICAL SKILLS MED 620: THE ART OF MEDICINE MED 640: REPRODUCTIVE/ HUMAN DEVELOPMENT (8 wks) MED 600 MED 610 MED 650: CARDIO/PULMONARY: WELLNESS & DISEASE (10 wks) SOCIETY AND COMMUNITY MEDICINE BREAK (2 wks) 4 SPRING BREAK 3 WINTER BREAK (3 wks) 2 ORIENTATION 1 ESSENTIALS OF CLINICAL SKILLS MED 620 ART OF MEDICINE YEAR 2 47 48 49 50 51 52 53 54 55 56 57 MED 740: NEUROSCIENCES/BEHAVIOR: WELLNESS & DISEASE (12 wks) MED 610: ESSENTIALS OF CLINICAL SKILLS MED 620: THE ART OF MEDICINE MED 620: THE ART OF MEDICINE MED750: MUSCULOSKELETAL/ DERMAL (4 wks) MED 760: GASTROINTESTINAL: WELLNESS & DISEASE (4 wks) SOCIETY/COMMUNITY MEDICINE ESSENTIALS OF CLINICAL SKILLS SPRING BREAK MED 610: ESSENTIALS OF CLINICAL SKILLS MED 750: MUSCULOSKELETAL/ DERMAL (4 wks) MED 600: SOCIETY/COMMUNITY MEDICINE WINTER BREAK (3 wks) MED 600: SOCIETY AND COMMUNITY MEDICINE BREAK (2wks.) MED 730: RENAL/ENDOCRINE: WELLNESS & DISEASE (10 wks) 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 MED 760: GASTROINTESTINAL (3 wks) MED 770: HEMATOLOGY/ ONCOLOGY (5 wks) SOCIETY/COMMUNITY MEDICINE ESSENTIALS OF CLINICAL SKILLS THE ART OF MEDICINE THE ART OF MEDICINE 95 96 97 98 99 100 101 102 103 BOARD PREP RESEARCH PROJECT YEAR 3 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 HOLIDAY BREAK (2 wks) 1 LONGITUDINAL CLERKSHIPS 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 LONGITUDINAL CLERKSHIPS CC - A (4 wks) CC - B (4 wks) CC - C (4 wks) CC - D (4 wks) YEAR 4 CC/CE (4 wks) CC/CE (4 wks) CC/CE (4 wks) CC/CE (4wks) CC/CE (4 wks) CC/CE (4 wks) CC/CE (2 wks) 2 wk. Holiday break 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 CC/CE (2 wks) 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 CC/CE (4 wks) CC/CE (4 wks) CC/CE (4 wks) CC/CE (4 wks) CC/CE (4 wks) Curriculum • College culture: respect, compassion, inclusiveness, social responsibility, excellence, innovation, curiosity • Integration of foundation and clinical science • Anatomy, biochemistry, physiology, pharmacology… • Psychology, decision science, continuous improvement… • Early clinical experience • Continuing foundation science education • Schemata and Patient Presentation model, simulated patients and families (relevancy) • Team-based learning (learning communities, in practices, in the hospital, friendly competition-game theory) • Inter professional (PA, PT, et al.) • Self directed learning/cognitive science Knowledge Scheme for Anemia ANEMIA MACROCYTIC NORMOCYTIC MICROCYTIC B12/Folate def. Iron deficiency Alcohol abuse (diet, chr. Loss) Chemotherapy Sideroblastic PRODUCTION I Aplastic anemia/rbc aplasia Myelodysplasia/Malig. CRF/Anemia of chr. Dis. INCREASED DESTRUCTION (>2% retics) INHERITED HbOPATHY Sickle cell Thalassemia Unstable HB MEMBRANE/ METABOLISM Spherocytic HMO shunt, Glycolytic BLOOD LOSS Visible/Occult Classification Mechanism ACQUIRED IMMUNE Coombs pos. Drug related Cold agglutinin Infection Mechanical TTP/HUS Malaria Causation/ Cases Flow Diagram of the Learning Process 1. Provision of schemata and assigned readings 6. Review of relevant anatomy and practice physical examination 11. Discussion of ethical & professionalism issues 2. Students prepare for instruction of coming week 3. Socratic session discussion of basic science principles 7. Socratic discussion of diagnostic process 8. Socratic discussion of treatment, focus on pharmacology 12. Open question & answer sessions 4. Large group discussion of clinical skills 9. Small group/ team work to identify and solve problems from PPs 13. Journal club/EBM session relevant to PP-diagnosis/ treatment Orange: large group information sharing and discussion sessions Blue: small group sessions Gray: clinical experience Yellow: large group Socratic sessions (questions based upon PPs) Green: student self-study sessions 14. Small group discussion of problems/solutions clinical experience 5. Discussion of “Patient Presentations” for the week 10. Discussion of patient management & adherence challenges – Society/Community 15. Formative assessments/ Discussion Typical Student Schedule for a Week of Instruction for Years 1 & 2 Day Time 8:00-8:50 9:00-9:50 9:50-10:00 10:00-10:50 Monday Tuesday Wednesday Socratic discussion of algorithmic approach to condition classification, etiology, pathophysiology , diagnosis, treatment, etc. Learning Goals: Diagnosis and Evaluation of relevant conditions Imaging & Lab Normal vs. Abnormal Learning Goals Society Matters in Health Care Patient presentationbased: management, adherence issues Learning Goals Art of Medicine Ethical Issues relevant to patient presentations Large Group- C Questions and answers on patient presentations – open student session Optional Large Group BC Large Group C Questions and answers on patient presentations – open student session Optional Large Group BC Large Group C Society Matters in Health Care EBM/Journal Review related to patient presentations Large Group C Break Applied Pharmacology Management of relevant conditions – Break Self-Study Break Clinical – Facilitator review of problem solving results for patient presentations Interactive patient presentation-based session to help students assess their understanding of concepts presented in self-study preparation Teams Large Group BC Break Essentials of Clinical Medicine History & Physical Examination Learning Goal Socratic, role play, video, session. Patient presentations distributed: Team Large Group C Interactive patient presentation- based session to help students assess their understanding of concepts presented in self-study preparation 12:00pm-1:00pm Break Learning Goal Large Group B Break 1:00-1:50 Clinical: Review anatomy, practice physical exam, Facilitated 11:00-11:50 2:00-2:50 3:00-3:50 4:00-4:50 Team 1 hr B, Anat. Lab 1 hr C, LG B Self-Study Anatomy Self-Study Thursday Friday Self-Study Self-Study Break Self-Study Team Facilitators Small Groups Break Self-Study Clinical – small group/team work on cases – identify and solve problems (2:00 – 5:00 pm) Team Clinical – small group/team work on cases – identify and solve problems (2:00 – 5:00 pm) Team Facilitator joins group from 4:00 to 5:00 pm Facilitator joins group from 4:00 to 5:00 pm Break Break Clinical session in family medicine practice Formative Evaluation Large Group BC Formative Evaluation Feedback, Review plans for next week Large Group BC Self-Study Encounter with cardiac patient(s) Practice V Self-Study Example Student Schedule for a Week of Instruction for Year 3 Longitudinal Integrated Clerkship Session & Schedule Monday Tuesday Wednesday Thursday Friday Saturday-Sunday Inpatient rounds if students have patients in hospital Pre-round if students have patients in hospital Patient Care work Patient Care work 3-self-directed learning, based on patient panel, 2small group case presentation/ discussion sessions. Patient Care work and end-day rounds as appropriate Community and Art of Medicine Curriculum Tutorials in basic and clinical science Patient Care work Afternoon Patient Care work Morning Patient Care work In-patient attending physician rounds Total instructional hours/ week: 5 hours rounds, 6 hours small group sessions = 11/week Curriculum • Longitudinal clinical skills curriculum – integrated with anatomy, imaging, physical examination, interviewing • Longitudinal courses: Art of Medicine, Society & Community Health • Clinical and health services/delivery research • Lean, process and quality improvement – including as research, at the practice and system levels • Population health, epidemiology, community health • Evidence-based medicine (proven practice) • Health system, care delivery, business of medicine, financing… • Assessments: to facilitate success for individual and team (simulations, mannequins, simulated patients, actual patients) Curriculum • Longitudinal, integrated clerkship • Gradual transitions as skills/knowledge develop • Focus on self assessment, lifelong learning, practice- based learning and improvement… • Rural/small community emphasis • Clinical experience based there • Community faculty as preceptors and facilitators • GME in the rural/small community setting • Patient Centered Medical Home CMU College of Medicine Office of the Dean 208 Rowe Hall Phone: (989) 774-7547 Web site: www.cmich.edu/med 26