permissive hypotension in hypovolemic shock resuscitation
advertisement
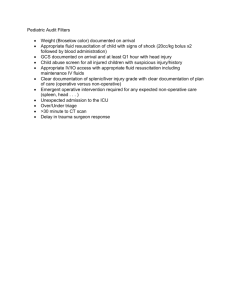
PERMISSIVE HYPOTENSION IN HYPOVOLEMIC SHOCK RESUSCITATION CDR GIRARD POIRIER MC USN Brief Review Shock - Inability of the body to adequately perfuse end organs which can lead to irreversible damage and death Hypovolemic shock from hemorrhage is common with severe injury and must be assumed until ruled out. The numbers: 10% of all trauma patients present with immediate post traumatic hypotension. Presence of shock in the pre-hospital setting is a strong predictor of mortality Prehospital Hypotension Predicts Mortality %Mortality 70 60 Blunt 50 Penetrating 40 30 20 10 0 120 + 120-90 90-60 60-0 SBP Classes of Hemorrhagic Shock Class I 750 mL (15%) ● Slightly anxious ● Normal blood pressure ● Heart rate < 100 / min ● Respirations 14-20 / min ● Urinary output 30 mL / hour ● Warm skin, Normal Cap Refill Class II 750-1500 mL (15-30%) ● Anxious ● Normal blood pressure ● Heart rate > 100 / min ● Decreased pulse pressure ● Respirations 20-30 / min ● Urinary output 20-30 mL / hour ● Pale, Cool, Cap Refill Delayed Class III 1500-2000 mL (30-40%) ● Confused, anxious ● Decreased blood pressure ● Heart rate > 120 / min ● Decreased pulse pressure ● Respirations 30-40 / min ● Urinary output 5-15 mL / hour ● V. Pale, Sweaty, Cap refill V Delayed Class IV >2000 mL (>40%) ● Confused, lethargic ● Hypotension ● Heart rate > 140 / min ● Decreased pulse pressure ● Respirations >35 / min ● Urinary output negligible Not All Trauma Patients are Alike Division into 3 categories Blunt Penetrating TBI / Head injury Not All Trauma Patients are Alike The very young and very old may present differently. Children have a very large reserve capacity Elderly may be on medications that blunt normal responses. Also may be unable physically to mount a tachycardic response. Finally, many elderly are hypertensive and may present as “normotensive.” Resuscitation History Goal was to normalize HR and BP Animal models of the 1950’s and 60’s showed benefit of aggressive fluid resuscitation. Subsequent review of methods showed numerous flaws Testing did not accurately reproduce the pathophysiology of an actual exsanguinating trauma patient Bleeding was tightly controlled as well as BP Overall paucity of controlled trials during that time. Resuscitation History Animal models in the 80’s and 90’s better designed. Improved physiologic modeling of actual trauma patients. Volume and duration of hemorrhage now dependent on animals physiological responses and not the operator. (thrombus formation as well as vasoconstriction) Experiments with this design showed harm with aggressive fluid resuscitation. Thought that aggressive fluid mgmt. led to clot disruption, dilution of clotting factors, and reversal of natural vasoconstriction. Historical Management 2 large bore IV’s 2 liters or saline or LR wide open Continue replacement / maneuvers until normalization of BP and HR MAST trousers, legs up in Trendelenburg, vasopressors Control bleeding The question of possible harm with aggressive resuscitation was actually broached during WWI by US Army Surgeon Cannon and published in JAMA 1917. Current ATLS Mgmt Identify and control source of bleeding (direct pressure, tourniquet, suture ligation, or surgery) Access (2 large bore periph IV’s, IO, CVL) 2 liters of warmed crystalloid initially if hypotension is present followed by fluids at a 3:1 ratio to accommodate fluid shifts into the interstitial spaces. Blood products only if no response to initial fluid bolus Prevent Hypothermia Choice of Fluid Crystalliod : LR vs NS. LR may be beneficial due to its buffering ability in acidosis and lessening risk of hyperchloremic acidosis. (studies show this benefit only in massive transfusions. No benefit with minimal replacements). Risk of hyperkalemia with use of LR, especially those with renal disease. Choice of Fluid Colloid : Theoretically a good idea. Rapidly expands circulating volume and stays in the circulation longer therefore much less third spacing of fluids. However, multiple studies have shown no benefit 2002 Cochrane Review actually showed increased RR of death in those receiving albumin Saline vs Albumin Fluid Evaluation (SAFE) showed no benefit using albumin. TBI patients at much higher risk of harm using albumin. Finfer S, Bellomo R, Boyce N, et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 2004;350(22):2247–56 Choice of Fluid Hypertonic Saline. Osmotic agent that can reduce cerebral edema in TBI Stays intravascular for longer period therefore decrease risk of lung injury and abdominal compartment syndrome (ACS) Human trials to date are inconclusive in showing benefit in the prehospital and initial treatment phases. Subgroup analysis: Blunt trauma receiving massive transfusion did show decreases risk of ARDS. TBI patients showed no changes in outcomes. Signif increase in mortality in trauma patients who did not receive blood transfusion in the first 24hrs. Kobayashi L. Hypovolemic Shock Resuscitation. Surg Clin N Am 92 (2012) 1403–1423 Choice of Fluid LR and transfusions: Currently not advised by the American Board of Blood Banks due to possibility of clot formation in lines. (calcium in LR may bind with Citrate preservative therefore increasing risk of clotting.) However, recent studies have shown this not to be the case especially in those receiving massive / rapid transfusions. Risk is greater with slower transfusion rates. New preservatives also in PRBC’s (AS-3) Michael Vlessides. Study: Ringer’s Lactate Does Not Trigger Clotting Cascade. Clinical Anesthesiology. OCTOBER 2008 | VOLUME: 34:10 Problems with Traditional Mgmt. Immediate and aggressive fluids to normalize BP with increase blood flow and perfusion pressures to injured areas. This may disrupt clot formation Will lead to significant third spacing of fluids leading to pulmonary as well as intestinal edema. Also, increased risk of abdominal compartment syndrome and ARDS Dilutional coagulopathy: starts at about 750ml of cystalloid admin. Uncontrolled Hemorrhage : Is Normal Blood Pressure the Target ? Roberts et al Lancet 2001 Bleeding or Re-bleeding Mechanic effect on vascular clot SAP Increase Agressive Volume Loading Hemodilution Anemia Hypothermia Hypoxemia Coagulation disorders Normal blood pressure is not the target ! Normotensive or hypotensive resuscitation ? A meta analysis Mapstone J, Roberts I, Evans PH , J TRAUMA 2003, 55 , 571 Favour hypotensive Favour normotensive Permissive hypotension improve survival ! What About Human Studies Landmark Study by Bickel and colleagues most cited. Compared immediate with delayed fluid resuscitation in penetrating trauma to the abdomen One group received standard fluid mgmt. while the other was delayed until reaching the OR. Std group received on avg about 2L of saline. Delayed group received 100-200cc) Overall survival of the Delayed group 70% vs 62% for Standard grp. Also noted was an increase in ARDS, pneumonia, sepsis, and coagulopathy in the standard group. Bickell WH, Wall MJ Jr, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 1994;331(17):1105–9 What About Human Studies Study By Owens and Colleagues Restrictive fluid resuscitation model following traumatic amputation significantly increased survival. Owens TM, Watson WC, Prough DS, et al. Limiting initial resuscitation of uncontrolled hemorrhage reduces internal bleeding and subsequent volume requirements. J Trauma 1995;39(2):200–7 [discussion: 208–9] Study By Morrison and Colleagues Evaluated differences between intra-operative MAP of 50 vs the standard of 65 in guiding resuscitation. Lower group exhibited less blood loss, less transfusion, improved early survival as well as improved mortality rates at 30 days Benefits most beneficial in penetrating trauma Morrison CA, Carrick MM, Norman MA, et al. Hypotensive resuscitation strategy reduces transfusion requirements and severe postoperative coagulopathy in trauma patients with hemorrhagic shock: preliminary results of a randomized controlled trial. J Trauma 2011;70(3):652–63 What About Human Studies Restrictive Fluids in Blunt Trauma Paucity of studies Turner and Colleagues compared fluid restriction in the field vs standard paramedic protocols. Significantly more blood was transfused in the standard group vs the restrictive group Flawed compliance by paramedics was significant. Turner J, Nicholl J, Webber L et al. A randomized controlled trial of prehospital intravenous fluid replacement therapy in serious trauma. Health Technol Assess 2000;4:1-57. What About Human Studies Head Injury There are no human studies that have evaluated hypotensive resuscitation in the trauma patient with concurrent head injury. What About Human Studies Subsequent studies have failed to reproduce consistently these results. Active debate continues on the uses of permissive hypotension Fluids should never be restricted to patients with a MAP of <40 who are pulseless. These patients have little chance of survival and any fluid admin to maintain some tissue perfusion outweighs any risk of increased hemorrhage risk. Mortality with Blood Transfusion Data shows a stepwise increase in mortality Table 2 Stepwise increase in mortality with transfusion Mortality Inaba PRBCs ( Units ) 1 – 10 Como et al, 15 22 % 2004 Huber-Wagner et al, 17 2007 et al, * Uncross-Matched <7 5 30 % 14.8 % >7 5 54 % 11 – 20 30 % 21 – 40 35.1 % 20 – 29 5 53.7 % 50 % 30 5 60.4 % >40 * This 59 % study includes patients given uncross-matched blood. 142 <15 5 78 % >15 5 95 % 2008 What is the Target MAP / SBP Coronary Autoregulation 50 160 Cerebral Blood Flow Autoreg. CPP = MAP - ICP Current Recommendations On Target MAP Most recent guidelines are based on expert opinion and results of animal and human trials. Goal is to limit the volume of infused fluids and maintain SBP at a minimum safe level. Target SBP of 80-90mmHg If concurrent brain injury is suspected then a goal of 100mmHg is recommended to ensure adequate perfusion in the face of possible increased ICP. Current Recommendations On Target MAP Morrison and Colleagues: Compared MAP of 50 vs 65mmHg (intra-operative) Showed significant reduction in fluid and transfusion requirements in the lower MAP group. Reduced post operative coagulopathy Statistically lower mortality in the immediate post op phase and trend toward lower mortality at 30 days Morrison CA. Hypotensive resuscitation strategy reduces transfusion requirements and severe postoperative coagulopathy in trauma patients with hemorrhagic shock: preliminary results of a randomized controlled trial. The Journal of Trauma. 2011 Mar;70(3):652-63 Current Recommendations On Target MAP Israeli Methods: Commence hypotensive resuscitation when one of the following is met: Altered mental status Loss of radial pulse SBP < 80 Up to 250ml of fluid are given at a time in order to return mental state, regain radial pulse, or SBP to 80mmHg Review The Bickel paper is the only randomly controlled trial which enables some conclusions to be drawn on the topic of hypotensive resuscitation. Some harm has been shown with aggressive fluid resuscitation in the field. Hypotensive resuscitation reduces blood loss and transfusion requirements. Animal studies consistently show that increased SBP in resuscitation increases or restarts bleeding. Evidence for hypotensive resuscitation in blunt trauma or TBI is sparse and needs further investigation. Permissive Hypotension in Other Areas of Medicine Leaking AAA : normal physiologic response to maint SBP 70-80. Treatment is to maint hypotension until proximal control achieved. Dissecting aneurysm : afterload reducing agents to induce hypotension Pulmonary contusions treated with fluid restriction Bleeding Duodenal ulcers treated by lowering BP and holding off on transfusion if possible until definitive treatment. Final Thought "There is nothing more difficult to take in hand, more perilous to conduct, nor uncertain in its success, than to take the lead in the introduction of a new order of things, for the innovator has for enemies all of those who have done well under the old, and lukewarm defenders in all of those who may do well under the new.“ - Machiavelli Questions ? Anecdotes From Your Practice ?