Fluid Resuscitation in Trauma
advertisement
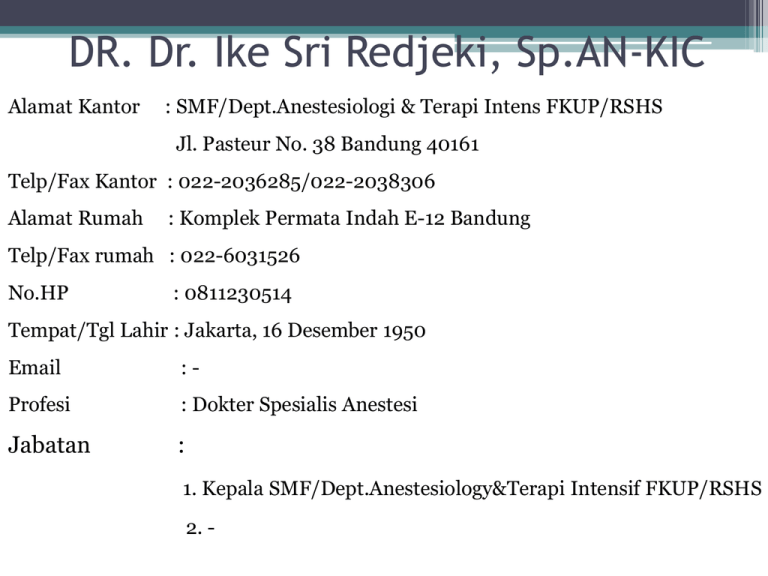
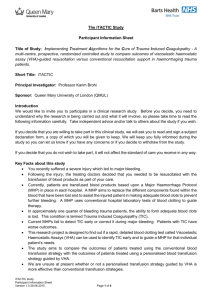
DR. Dr. Ike Sri Redjeki, Sp.AN-KIC Alamat Kantor : SMF/Dept.Anestesiologi & Terapi Intens FKUP/RSHS Jl. Pasteur No. 38 Bandung 40161 Telp/Fax Kantor : 022-2036285/022-2038306 Alamat Rumah : Komplek Permata Indah E-12 Bandung Telp/Fax rumah : 022-6031526 No.HP : 0811230514 Tempat/Tgl Lahir : Jakarta, 16 Desember 1950 Email :- Profesi : Dokter Spesialis Anestesi Jabatan : 1. Kepala SMF/Dept.Anestesiology&Terapi Intensif FKUP/RSHS 2. - Fluid Resuscitation and Transfusion for Trauma Ike Sri Redjeki RS Hasan Sadikin/ FK. UNPAD Bandung When Fluid Resuscitation is Needed ? In SHOCK ! SHOCK Blood loss True Hypovolaemia Sepsis Apparent Hypovolaemia (vasodilation) Pump Failure” “ Saline loss Dehydration Peripheral circulatory failure INADEQUATE CARDIAC OUTPUT Plasma loss Cardiogenic Pulmonary Embolus Tamponade Tension pneumoTx Neurogenic Anaphylaxis Adrenal insufficiency Concept of pathogenesis of physiologic changes in Multiple Trauma Trauma Inflammation Activation of haemostasis & endothelium Haemorrhage Shock Tissue Hypoxia and Coagulopathy Acidosis Fibrinolysis Primary Survey In Trauma Patients • Patients are assessed and treatment priorities established based on their injuries, vital signs, and injury mechanisms • ABCDEs of trauma care –A –B –C –D –E Airway and c-spine protection Breathing and ventilation Circulation with hemorrhage control Disability/Neurologic status Exposure/Environmental control What is the Recommendation ? ( Sphan et al critical Care 2013,17:R76) • Initial resuscitation and prevention further bleeding • Minimal elapsed time – The time elapsed between injury and operation be minimised for patients in need of urgent surgical bleeding control – Grade 1A – Adjunct touniquet use to stop life threatening bleeding from open extreemity injuries in the pre surgical setting – Grade 1B What is the Recommendation ? ( Sphan et al critical Care 2013,17:R76) • Patients presenting with haemorrhagic shock and an unidentified source of bleeding undergo immediate further investigation – Grade 1B • Chest • Abdominal cavity • Pelvic ring Further CT for haemodynamically stable patient What is the Recommendation ? ( Sphan et al critical Care 2013,17:R76) • It is not recommended the use of single Hct measurement as an isolated laboratory marker of bleeding – Grade 1B • Serum lactate or base deficit measurement as sensitive test to estimate and monitor the extent of bleeding and shock – Grade 1B • Routine practice to detect post traumatic coagulopathy include the early, repeated and combined measurement of PT, APTT, fibrinogen and platelets – Grade 1C Recommendation of Fluid Therapy in Trauma Patients • Fluid therapy be initiated in the hypotensive bleeding trauma patient – Garde 1A • Crystalloids first choice – Grade 1B • Avoid hypotonic solution RL sol • Coloids used within the prescribed limit for each solution • Hypertonic solution for unstable penetrating torso trauma – Grade 2C Recommendation of Fluid Therapy in Trauma Patients • Administration of vasopressors to maintain to target MAP if no response to fluid therapy – Grade 2C • Or inotropic myocardial dysfunction • Maintain temperature > 35 degree C – Grade 1C • Target Hb 7 – 9 gr% • Damage control resuscitation is now the predominant focus upon arrival in hospital • Crystalloid delivery should be minimized, as it can be associated with harm • Trauma-induced coagulopathy is a common problem caused by dilution and consumption of clotting factors, hypothermia and acidosis • Evidence suggests it can be decreased by early delivery of blood products • The best resuscitation appears to be with whole blood rather than component therapy • Can 1:1:1 ( Plasma : RBC : Platelets ) ever be an adequate substitute for fresh whole blood, or should blood banks consider a return to using whole blood? • Tranexamic acid should be consider and is significantly cheaper ( compare to Factor VII ) • Giving unnecessary plasma and platelets should be discouraged in order to reduce the risk of transfusionrelated acute lung injury • Poin of care coagulation tests may aid decision making and reduce unnecessary transfusionst of care • Massive transfusion protocols, improve communication and delivery of blood products to the patient • Enable clinicians to give fresh plasma up front, rather than giving red blood cells initially and plasma later How about Crystalloid ? • Giving a significant amount of crystalloid upfront on admission a common practice leading to various problem : Abdominal compartment syndrome ( ACS ), Acute Resp Distress Syndrome (ARDS ), multiple organ failure • Giving crystalloid > 1.5 liters in emergency department independent risk factor for mortality > 70 years old OR 2.89 and Non elderly patients OR 2.09 • High volume ( > 3 liters ) > 70 years OR 8.61, • Using Colloid decreased lactate level and < renal injury better tissue resuscitation Transfusion Strategy • Masive transfusion : > 10 unit RBc within 24 hour • A significant advantage of Warm Fresh Whole Blood over component therapy contain full amount of platelets • Even vs best practice component therapy 1: 1:1 Fresh Whole Blood >> effective than Component Damage control resuscitation (on admission) • Rapid control of surgical bleeding • Early and increased use of red blood cells, plasma and platelets in 1: 1: 1 ratio • Limitation of excessive crystaloid use • Prevention and treatment of hypothermia, hypocalcemia, and acidosis • Hypotensive resuscitation strategies Sphan et al Critical Care 2013; 17:R76 – 1-45 Current recommendation for blunt trauma is to administer just enough fluid to maintain perfusion Rapid, high-volume fluid administration is discouraged Recommendation : Target BP systolic 80 – 90 mmHg, until major bleeding stop afterwards optimalized In patients combined haemorragic shock and severe TBI (GCS < 8) MAP > 80 mmHg Permissive Hypotension in Traumatic Brain Injury • Oxygenation and Blood Pressure – Hypoxemia (<90% SpO2) and/or hypotension (<90 mm Hg systolic) are associated with poor outcomes. – Pulse oximetry and blood pressure must be monitored. – Continuous waveform capnography beneficial CPP = MAP- ICP Slightly higher systolic pressure may be required to maintain CPP in TBI Target of Fluid Ressuscitation DO2 = (CO x Hb x SpO2 x 1.34 ) + (PaO2 x 0,003) ↓ O2 Balance O2ER= VO2 / DO2 = 25% ↓ VO2 = O2 Consumption CONTROL CENTER IN THE MICROENVIRONMENT Glycocalyx http://www.glycocalyx.nl/background.php Structure of Glyccocalyx Glycocalyx Endothelial cell Reitsma S, et al. Eur J Physiol 2007; 454:345–359 Protect the Vessel Wall ELECTRONE MICROGRAPH OF MYOCARDIAL CAPILLARY Gouverneur M, Van den berg B, Nieuwdorp M, Stroes E, Vink H. Journal of Internal Medicine 2006; 259: 393–400 Alteration of Glycocalyx leads to extravasation • Alteration in the composition of the glycocalyx Hypervolemia following exposure to an inflammatory insult is one of the earliest features ↓ of endothelial activation • It is nowLeads acceptedtothat TNFα, oxidised disruption of the lipoproteins, lipopolysaccharide, thrombin, glycocalyx ischaemia/reperfusion, hyperglycaemia and growth factors all cause glycocalyx disruption via the action of proteases Conclusion • First hour of trauma management ABC’s primary survey and secondary survey being accomplished as fast as possible • The time elapsed between injury and operation be minimised for patients in need of urgent surgical bleeding control • Damage control resuscitation on admission • Shock in trauma cases mostly hypovolemia restore the iv volume • Fluid resuscitation avoid further damage • Keep the blood pressure not to high before hemorrhage being controlled • Avoid hypervolemia • Target of resuscitation balance between DO2 and VO2 Conclusions • Blood transfusion Masive transfusion can be predicted ( BE -10 and Hb • Prefer to use WFWB than blood component • Blood component 1 : 1 : 1 • Use plasma first to prevent traumatic coagulopathy