File - Ashley Jacobson's Portfolio
advertisement
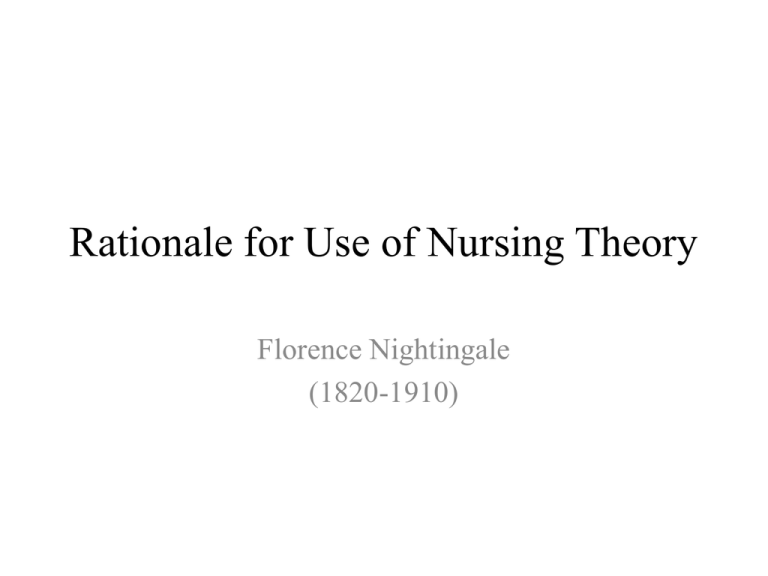
Rationale for Use of Nursing Theory Florence Nightingale (1820-1910) • Our group decided to use Florence Nightingale as our theorist. • We choose Nightingale because she set the standard for modern nursing (Tomey and Alligood, 2006). • Her theories and philosophies have changed the way nursing is practiced today. • Nightingale focused on a clean environment, air, water, efficient drainage, and efficient light (Tomey and Alligood, 2007). • Our group discussed how much we use Nightingale’s theories in our everyday practice. • Pam works in the operating room (OR). One of the most important factors in the operating room is keeping it as clean as possible. The doctors have to scrub in and remain as sterile as possible, sterilized equipment is used and the patient always gets a betadine scrub before surgery. All of these factors help reduce the chance for an infection. The OR uses the proper lighting and equipment to provide safety for the patient. • Rachel works on a Medical Surgical unit. She gets a variety of sick patients and must incorporate Nightingales theories. • If patients are sharing a room, it is most important to keep the room clean and free of clutter. Also, privacy is important when patients are in a semiprivate room. • Rachel accommodates her patients by using the divider curtain, talking to her patients in a low voice so the patient in the other bed cannot listen to their conversation. She discussed the importance of the patients belongings staying separate, and keeping their intake and outputs labeled for the correct patient. It is most important for Rachel to keep the patients environment clean, safe and comfortable for the patients to get well. • Ashley works on a cardiac unit and uses Nightingale’s theory in everyday practice as well. It is important to manage the patients pain, perform incision care to decrease chance of infections and provide a safe environment to promote healing. Nightingale said it best, “A contaminated, dirty, dark environment led to disease. Not only could she prevent disease from flourishing in such an environment, but she also recognized that disease prevention would be achieved through environmental controls” (Tomey and Alligood, 2006, p.79). The Nightingale Metrics Research Findings • • • This article discusses a study in an inpatient Cardiovascular and Critical care program at a Children’s Hospital in Boston. This hospital has a cardiology unit and three critical care units. There is a pediatric intensive care unit (PICU), a cardiovascular intensive care unit (CICU), and a neonatal intensive care unit (NICU). Martha Curley, one of the authors of this study, started the program. She met with nurses on each unit to talk about nursing care that they thought was most important in providing better patient outcomes (Curley and Hickey, 2006). “The Nightingale Metric project, where by staff nurses at our facility, Children's Hospital Boston, could identify which interventions were most important to patients and families, measure how often nurses performed these interventions, and use the data to improve care” The same question was asked to each group, “How do you put patients and families in the best condition for nature to act upon them?” (Curley and Hickey, 2006, pg. 66). “During their annual self-evaluation each nurse had to use exemplars to articulate his or her contributions to a patient outcomes, but in these sessions nurses spoke about their collective contributions. These sessions generated a preliminary list of “nursing care indicators,” chosen according to established and measurable standards of care” (Curley and Hickey, 2006, pg. 67). • The study was conducted at three month intervals. • “This process resulted in a set of what we called “Nightingale metrics” for each units: aspects of care identified by the nurses as important to the population served by that unit, reflected as standards of care, based on evidence, and measurable” (Curley and Hickey, 2006, pg.67). • Studies were conducted on each unit differently. Data was collected every three months and the data would show the rate that nurses were completing the assessments that were marked as most important. • If the goal was not met, then improvements were made, staff was reminded, and follow up with clinical nurse specialist was done on daily rounds (Curley and Hickey, 2006). • Audits were done every three months. If improvement was indicated, monthly audits were done until improvements were made. If the results were perfect for three audits in a row, then they were done yearly (Curley and Hickey, 2006, pg. 67). • A bundle approach was also used on the different units. This type of approach is used more commonly to improve quality monitoring (Curley and Hickey, 2006). • “A bundle describes a group, say three to five, of evidence-based steps that must be taken to improve a clinical outcome” If all the bundles are not done, then the entire bundle is incomplete. (Curley and Hickey, 2006, pg. 68). • The three ICU floors did a study on the percentage of patients where pain assessments were completed every four hours. At the end of the study, one ICU did better than the other two. • Another study was done on the percentage of ventilated patients who received ventilator-associated pneumonia (VAP) bundle. They only hit the 100% mark once. There staff needs to be more compliant with this study. • Data is collected quarterly. It happens on random days by chart audits, direct observation, or both. Chart audits are limited to the past seven days (Curley and Hickey, 2006). • A study was performed on continuity of care What is continuity of care? • “While most of the nightingale metrics were “process indicators” describing nursing care, we also monitored a “system indicator” that described one aspect of nurse staffing: continuity of care (Curley and Hickey, 2006, pg. 69). • This study made sure that the same nurse or a few nurses cared for the same patient each day. • “It was monitored by calculating the continuity-of-care-index (CCI),dividing the number of different nurses caring for a patient during a hospitalization by the number of nursing shifts in that hospitalization” (Curley and Hickey, 2006, pg. 669). • “They have found that, overall, the number of nurses assigned to each patient should be limited: the greater continuity of care, the better knowledge the nurses, patient, and family have of one another” (Curley and Hickey, 2006, pg.69). Examples of Nightingale Metrics • INPATIENT CARDIOLOGY UNIT • In patients at risk for congestive heart failure, documentation of total intake and output every 24 hours and daily weight. • In newborns to be discharged in 72 hours, documentation of results of a phenylketonuria test, the car-seat challenge, and hearing screening. • In patients undergoing noninvasive monitoring, the setting of the monitor on a mode appropriate for age (paced, if needed) and the alarm limits on ± 20% of baseline heart rate, respiratory rate, and oxygen saturation. • “Time to critical intervention”: the number of unplanned patient transfers to the (CICU) and the time interval from first assessment of distress to CICU transfer (Curley and Hickey, 2006, pg.70). Pediatric Intensive Care Unit • Documentation of sedation score every 4 hours. • In patients with a central venous line, changing the dressing every 7 days. • Establishment of a nutrition plan within 24 hours of admission. • The double checking of all medications by 2 nurses. • Pressure ulcer bundle: if patient is immobile, documentation of position change every 2 hours and positioning of heels off the bed; if not on bed rest, documentation of patient being out of bed or held in parent’s or nurse’s arms. • Ventilator-associated pneumonia bundle: Head of bed elevation at 30°–45°; documentation of oral hygiene twice in 24 hours; peptic ulcer prophylaxis (in patients not receiving tube feedings); discussion of extubation readiness test on rounds; daily holiday from sedation and chemical paralysis. • “Time to critical intervention”: “panic” laboratory value, the time intervals from sending specimen to laboratory to first intervention to correct the laboratory value (Curley and Hickey, 2006, pg.70). Cardiac Intensive Care Unit • Documentation of PR interval at the start of each shift. • Checking central line blood return at the start of each shift. • Presence or absence of pressure abrasion from oxygen saturation monitoring. • Adult care bundle: in patients on bed rest, wearing of compression boots and stockings and maintenance of potassium > 4 mEq/L; in extubated patients, getting the patient out of bed before 10 AM and health care proxy in place. • Neonatal care bundle: placement of physical boundary; documentation of head circumference on admission; maintenance of temperature, 36.5°C– 36.7°C; placement of those weighing < 2 kg in an isolette; checking glucose level every shift. • “Time to critical intervention”: interval between fever (> 38.5°C) and administration of first antipyretic (Curley and Hickey, 2006, pg.70). Neonatal Intensive Care Unit • Documentation of weight daily (for up to 7 days). • Parental notification of patient’s transfer status. • Documentation every 2 hours of turning or repositioning of immobile patients. • Confirmation of nasogastric tube placement by checking the pH level of aspirate. • Discussion of intravenous access plan on rounds for patients with difficult vascular access. • Documentation of baseline withdrawal score in patients being weened off opioids. • Safety bundle: placement of hand disinfectant at bedside; setting of oxygen saturation alarms according to protocol; placement of 1 size of each suction catheter at bedside; peripheral IV visible; securing of servomechanism for temperature regulation (visible and not on bony prominence). • “Time to critical intervention”: panic laboratory value: the time intervals from sending specimen to laboratory to first intervention to correct the laboratory value. Florence Nightingale How Her Theory Framed the Research • • • • • • • Nightingale thought a clean environment and healthy surrounding was best for the patient. “Her theory of the five essential components of environmental health: pure water, pure air, efficient drainage, cleanliness, and lights” (Tomey and Alligood, 2006, p75). “Proper ventilation for the patient seemed to be of greatest concern to Nightingale; her charge to nurses was to keep the air he breaths as pure as the external air, with out chilling him (Tomey and Alligood, 2006, p. 75). In one of the studies that took place at Boston Children’s Hospital was the ventilator- associated pneumonia bundle. It was their goal for the patients to have proper air and care provided to keep the patient from developing pneumonia. Nightingale was also concerned for the patient and wanted the best care given possible. This study developed a continuity of care study. It showed that the less nurses caring for a patient, the greater the care they receive. The studies were done in three month interval to try to keep track of results and see if goals were met. “Trying a measurement process to nursing vigilance and preventative care is one way of building upon the legacy of Florence Nightingale” (Curley and Hickey, 2006, p.69). Critique of the Research • The study was only done on four units. • Only some nurses took part in the questioning of what they though was important nursing care related to patient outcomes. • They study did not have 100% compliance from all the nurses. • When compliance was low an improvements needed to be made, they did monthly audits until data improved. • The nurses were retrained if needed, given reminders and followed up with a clinical nurse specialist during daily rounds (Curley and Hickey, 2006). Implications For Practice • • • • • • • • This main aspect of this study was to take care, assess , and implicate care on patients. Nurses had to assess and document the care that was given for the study to work. If there was non-compliance or changes that needed to be made in the study, than the appropriate step were taken. I utilize these mechanism in my standard of care, but the difference between the study was the ages of the patients. I take care of adult patients. I also do not take care of ventilated patients. However, I know how important it is to get the cardiac patient up walking, cough and deep breathing, teaching patients how to use an incentive spirometer and to spit out pulmonary secretions. It is important to assess pain management on all patients. This is a standard part of my everyday practice. I agree with continuity of care as well. I find if I have the same patients three days in a row, we have developed a trusting relationship, their families do as well, and it seems that the patient receives better care. I have taken care of patients for four hours and it is really difficult to develop any type of a relationship with the patient and family. It also makes it difficult due to time restraints to know exactly what is going on with the patients. Critical Reflection • I thought this study was very useful. It is important to asses the patients pain levels, try to prevent pneumonia from the ventilator and improve the patients continuity of care. • It is important to reassess the research often to see if appropriate changes need to be made. • I think the Nightingale Metrics used on the in patient cardiology unit, PICU, NICU and CICU were great standards. These standard prove to be efficient as long as there is compliance by the staff. Even though I work with adults, most of these examples I use in everyday care. • These factors are important and some may seem basic. As Florence Nightingale stated, “What nursing has to do…is to put the patient in the best condition for nature to act upon him.” (Curley and Hickey, 2006, p.66).