Urinalysis
advertisement

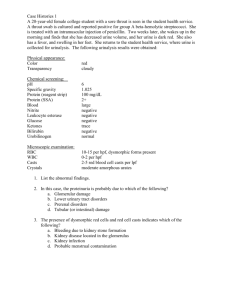
Interpretation of abnormalities in urine Shiva Seyrafian Isfahan University of Medical Sciences 20/8/1391 11/10/2012 The aim of this lecture 1. Urine tests (GFR and Proteinuria) 2. Urinalysis and urine sediment What you should learn at the end of this lecture 1) To know what are the urine tests. 2) How do we measure urine tests? 3) What is urinalysis? 4) How do we exam urinalysis? 5) What is the benefit of learning urine tests and urinalysis? Tests of Glomerular Filtration Rate • Creatinine Clearance • Normal finding : male : 90-139 ml/ min female : 80-125 ml /min Calculation of creatinine clearance 1. 24 hour urine collection • C cr = U cr x V/ P cr 2- Cockroft- Gault Formula • C cr = (140 – age in years) x ( lean body weight in Kg) / S cr x 72 • For women multiply final value by 0.85 OR put 85 instead of 72. 3- Modification of Diet in Renal Disease Formula • GFR = 186 X (Cr) -1.154 x age -0.203 x [0.742 (if woman)] • Normal range = 95 -105 ml/min/ 1.73 m2 • Low Cr clearance: 1. Acute renal failure (ATN, AIN, Acute GN) 2. Chronic renal failure: Chronic glomerulonephritis, chronic HTN, DM 3. UTO 4. Old age Tests that predict kidney disease Albumin/ Creatinine Ratio (ACR or Microalbumin) Albumin Creatinine Ratio (Microalbumin) In health, there is very little or no albumin in the urine Most dip sticks report albumin at greater than 150 mg/L Normal microalbumin: 30 -300 mg/24hrs Urinary Albumin – cont’d Detection of low levels of albumin (even if below dipstick cut-off) is predictive of future kidney disease with diabetes Very significant variation usually requires repeat collections Microalbuminuria: DM, Hypertension and early GN Urinalysis • The most commonly performed • As a screening procedure for asymptomatic individual. • To confirm the presence of renal disease, diabetes, or, more rarely, liver disease. • can be performed in emergency rooms, outpatient clinics, private physicians' offices, and patients' homes. Urinalysis • Three types of urinalysis can be performed: 1-dipstick urinalysis, 2microscopic urinalysis, 3-cytodiagnostic urinalysis (specialized analyses). 1,2= routine urinalysis • Cytodiagnostic urinalysis is more timeconsuming than traditional microscopic analysis Specimen Collection • Midstream, catheterized, suprapubic aspiration • Ideally within 30 minutes of collection • Specimens > 2 hours old are inaccurate • Can be refrigerated at 4oc up to 6 hours • Amorphous urate may precipitate • Should return to room temperature Urinalysis 1. macroscopic analyses consisting of physicochemical determinations (appearance, specific gravity), and multi-parameter reagent-strip measurements of biochemical constituents, 2. microscopic examination of urinary sediment: hematuria, pyuria, cylindruria (casts), crystalluria, and others. Physical Examination of Urine physicochemical determinations i. Volume (750 -2000 ml/ day) ii. Odor (Mild, inoffensive odor) iii. Appearance (color and turbidity) Bad odor to the urine • Either cystitis or vaginitis • Look for: -Lost and forgotten tampon -Yeast -Trichomonas -Bacterial vaginosis -Asparagus eating -Ampicillin intake Color of urine urine color due to Metronidazol Physical Examination of Urine physicochemical determinations iv. Specific gravity: refractometer [measures the density (mass per unit volume) of the suspended particles] The normal range is 1.003 to 1.035 g/mL. A value of 1.020 or greater indicates good renal function Physical Examination of Urine physicochemical determinations • V. Osmolality: osmometer ( the number of particles per unit mass). • The healthy kidney is capable of producing urine with a wide range of concentrations, from 50 to 1200 mOsm/kg. Normally, a urine's osmolality will range from approximately one-sixth to four times the osmolality of normal serum (280 to 290 mOsm/kg). Physical Examination of Urine Reagent-strip testing urine pH • The urinary pH range is usually 4.7 to 7.8. Extremely acidic or alkaline urine usually indicates a poorly collected specimen. • More acidic with increased meat intake • More alkaline with vegetarian diet • High pH with prolonged storage or urea splitting organisms, diuretic therapy, vomiting, ,gastric suction and alkali therapy. Chemical Examination of Urine Reagent-strip testing Blood and myoglobin Normally not detectable in the urine Oxidizing agents such as povidone - iodine and myoglobin will cause a positive reaction Positive dipstick without RBCs suggests hemolysis or rhabdomyolysis. • Chemical Examination of Urine Reagent-strip testing • Bilirubin: no detectable in the urine • Urobilinogen: 2-10 mg/L Only conjugated bilirubin is passed into the urine. In hemolysis urine urobilinogen is often positive False positive test for urine bilirubin can occur if the urine is contaminated with stool Prolonged storage and exposure to light can lead to false negative results. Chemical Examination of Urine Reagent-strip testing • Sugars: not detectable sugars in the urine. • Ketones: not detectable in the urine • Nitroprusside reaction used to detect ketones (acetone and acetoacetate) • b-OH butyrate is not normally detected Chemical Examination of Urine Reagent-strip testing • Nitrites: detect bacteriuria: measures the nitrite formed from converaion of nitrates to nitrites by certain bacteria in urine. • Normally does not contain detectable nitrite. • False negative: • Ascorbic acid and high urine SG • Low urinary nitrates (due to diet) • Rapid transit of urine (takes 4 hrs to convert nitrates to nitrites in bladder ) • Degradation of nitrites (prolonged storage of urine) • Gram positives, N. gonorrhea, M. TB. Chemical Examination of Urine Reagent-strip testing • Leukocytes: pyuria (leukocytes in urine) are based on the presence of intracellular esterases released from lysed granulocytes, . • Normally does not contain detectable leukocytes. • False positive • Long standing urine, more granulocyte lysis • Vaginal contamination Normal Proteinuria • 30 to 150 mg/day • Usually only small proteins (<20,000 daltons) pass across capillary wall and most are reabsorbed in prox. tubules e.g., a2-microglobulin, apoproteins, enzymes, peptide hormones • Tamm-Horsfall protein (uromodulin) • High m. wt. 23 x 106 daltons glycoprotein • Thick ascending limb and distal convoluted tubule • IgA and urokinase in small amounts • Protein : False Negative Results proteins proteins False Positive Result Bence Jones Heavy-chain Alkaline urine • Sulfosalicylic acid: False negative Alkaline urine Microscopic Examination Of Urine Microscopic Examination • Cells • Casts • Crystals • Organisms • Artifacts Chemical Examination of Urine – Microscopic examination of urine • Red blood cell: Less than 3 erythrocytes per highpowered field • White blood cell: Less than 5 leukocyte, per three high-power fields (400X). 3000 cells/mL • Twice RBC size, cytoplasmic granulation • Inflammation or infection • Eosinophils, best seen with Hansel’s stain or Wright’s stain RBC WBC Epithelial Cells • Squamous, transitional, renal epithelial cells • Squamous epithelial cells • Large flat, 30 to 50 micrometers in diameter • Nucleus to cytoplasm size ratio is 1:6 • Contamination from distal genital tract Squamous epithelial cell Renal epithelial cell Casts • Renal casts are cylindrical structures that are formed in the nephron and excreted in the urine. Casts are significant because of their localizing value. Casts are composed of mucoprotein, or uromucoid, (TammHorsfall protein), which is always present in urine, usually in solution. Casts • The Tamm- Horsfall mucoprotein is produced by the tubular epithelial cells lining the ascending limb of the loop of Henle. • Casts are formed when urine stasis exists, which allows uromucoid to precipitate. • Increased concentrations of protein and salts and a low urine pH all contribute to cast formation. Casts • Casts: Less than 3 hyaline casts, zero to one granular cast, and no pathological cast per low-power field (100X). • Casts include: • RBC • WBC • • • • • Epithelial Granular Hyaline Fatty Waxy RBC Cast RBC Cast WBC Cast WBC Cast Hyaline cast Granular cast Waxy cast Fat droplets, Oval fat bodies in nephrotic syndrome Nephrotic syndrome Renal epithelial cell cast in ATN Crystals • Least clinically important • Crystals exist with/without presence of stones • Cooling urine will have some crystal precipitate • More in concentrated urine • Crystals: Small numbers of common, nonpathological crystals, such as uric acid or phosphate crystals. No specific disease, Present in Ca Ox stones and ethylene glycols toxicities No specific disease, Present in Ca Ox stones and ethylene glycol toxicities No specific disease Present in uric acid stones No specific disease Present in uric acid stones Specific in cystinuria Coffin lid • Fungus, parasites, or viral inclusion cells: None. • Bacteria: Less than 10 bacteria per highpower field (400X). Summary 1. Urinalysis is used as a routine test. 2. GFR, proteinuria and urinalysis are the most important tests. 3. cellular casts are more important than crystals.