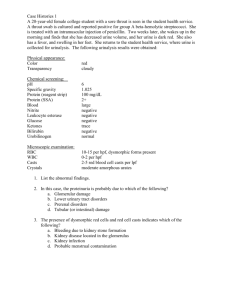
Routine Urine Analysis
advertisement

Routine Urine Analysis Dr.Ather Farooq MBBS, Mphil Hematology Urine: • Is an ultrafiltrate of plasma from which glucose, amino acids, water and other substances essential to body metabolism have been reabsorbed. • Urine carries waste products and excess water out of the body. Urine consists of: (96%) water (4%) dissolved solids: (2%) Urea: (half) (2%) Other compounds Inorganic: Cl-, Na, K. trace amounts of: sulfate, HCO3 etc.) Organic: creatinine uric acid Collection of urine specimens • Containers for collection of urine should be wide mouthed, clean and dry. • Analysed within 2 hours of collection else requires refrigeration. Types of urine sample Sample type Sampling Purpose Random specimen most common, taken anytime of day Routine screening, chemical examination. Morning sample First urine in the morning, most concentrated Pregnancy test, microscopic test Midstream Discard first few ml, collect the Culture rest 24 hours All the urine passed during the used for quantitative and day and night and next day Ist qualitative analysis of sample is collected. substances,Protiens,AFB, Microalbuminurea Postprandial 2 hours after meal Determine glucose in diabetic monitoring Urine examination • Macroscopic examination • Chemical examination • Microscopic examination Macroscopic examination • • • • • Volume Color Transparency Odour PH Urinary volume • • • • • Normal = 600-1550ml Polyuria- >2000ml Oliguria-<400ml Anuria-complete cessation of urine(<200ml) Nocturia-excretion of urine by a adult of >500ml with a specific gravity of <1.018 at night (characteristic of chronic glomerulonephritis) Color • Normal= clear & pale yellow Color Many things affect urine color, including fluid balance, diet, medicines, and diseases. Color intensity of urine correlates to concentration. Amber yellow Urochrome (derivative of urobilin, produce from bilirubin degradation, is pigment found in normal urine). Colorless due to reduced concentration. Silver or milky appearance Reddish brown Yellow foam Pus, bacteria or epithelial cells Blood (Hemoglobin). Bile or medications. Orange, green, blue or red medications. Transparency Transparency Urine is normally clear. Bacteria, blood, sperm, crystals, or mucus can make urine look cloudy. Is classified as clear or turbid. In normal urine: the main cause of cloudiness is crystals and epithelial cells. In pathological urine: it is due to pus, blood and bacteria. Degree of cloudiness : Turbidity: may be due to gross bacteriuria, Smoky appearance: is seen in hematouria. Thread-like cloudiness: is seen in sample full of mucus. Urinary pH • Reaction reflects ability of kidney to maintain normal hydrogen ion concentration in plasma & ECF • Normal= 4.6-8 • Tested by- 1.litmus paper 2. pH paper 3. dipsticks Odour • Normal= aromatic due to the volatile fatty acids • Ammonical – bacterial action • Fruity- ketonuria • Maple syrup - Maple syrup disease Chemical examination • • • • • • • • • • • Proteins PH Sugars Ketone bodies Bilirubin Bile salts Urobilinogen Blood Leucocytes Nitrite Specific Gravity Urine dipsticks Urine dipstick is a narrow plastic strip which has several squares of different colors attached to it. Each small square represents a component of the test used to interpret urinalysis. The entire strip is dipped in the urine sample and color changes in each square are noted. The color change takes place after several seconds to a few minutes from dipping the strip. The dipstick method of chemical analysis of urine Specific gravity • Depends on the concentration of various solutes in the urine. • Measured by-urinometer - refractometer - dipsticks Specific gravity • Normal :- 1.001- 1.040. Increase - Low water intake, Diabetes mellitus, Albuminuruia, Acute nephritis. Decrease - Absence of ADH, Renal Tubular damage. Heat Test • • • • • Procedure Take a 5 ml test tube. holding the tube from the bottom while heating the upper part Fill 2/3rd with urine. Boil upper portion for 2 minutes (lower part acts as control. If precipitation or turbidity appears add a few drops of 10% acetic acid. Interpretation • If turbidity or precipitation disappears on addition of acetic acid, it is due to phosphates; if it persists after addition of acetic acid then it is due to proteins • • • • • • • No cloudiness = negative. Cloudiness against dark background = traces (less than 0.1 g/dl). Cloudiness without granularity = + (0.1 g/dl). Granular cloudiness=++ (0.1-0.2 g/dl) Precipitation and flocculation = +++ (0.2-0.4 g/dl). Thick solid precipitation = ++++ (0.5 g/dl). Benedict’s test Heat to boiling for 2 minutes . Interpretation No change of blue colour = Negative Greenish colour = traces (< 0.5 g/dl) Green/cloudy green ppt = + (1g/dl) Yellow ppt = ++ (1-1.5g/dl) Orange ppt = +++ (1.5-2g/dl) Brick red ppt = ++++ (> 2g/d Microscopic examination • Microscopic urinalysis is done simply pouring the urine sample into a test tube and centrifuging it (spinning it down in a machine) for a few minutes. The top liquid part (the supernatant) is discarded. The solid part left in the bottom of the test tube (the urine sediment) is mixed with the remaining drop of urine in the test tube and one drop is analyzed under a microscope Make condenser low with partial closure of diaphragm . First examine it under low power, then under high power and keep on changing the fine adjustment in order to visualize the sediments in different planes and report as …..cells/HPF (high power field). Contents • • • • 1. Cells (RBCs,WBCs, epithelial cells) 2. Casts 3. Crystals 4. Miscellaneous structures Cells RBCs RBC's may appear normally shaped(pale or yellowish, biconcave), swollen by dilute urine or crenated by concentrated urine. Hematuria White Blood Cells These appear as round granular 12-14 μm in diameter Pyuria refers to the presence of abnormal numbers of leukocytes that may appear with infection in either the upper or lower urinary tract or with acute glomerulonephritis. May indicate urinary tract infection UTI if more than 10/HPF Pyuria Epithelial Cells • Squamous epithelia – Large flat cell with central oval nucleus • Transitional (bladder) epithelia – Spindle shaped with large oval nucleus – Maybe in sheet • Renal tubular epithelia – Small cell with large oval nucleus – Most clinically significant Squamous Epithelia Transitional Epithelia Renal Tubular Epithelia RTEC Sq EC Casts • Urinary casts are formed only in the distal convoluted tubule (DCT) or the collecting duct (distal nephron). • The proximal convoluted tubule (PCT) and loop of Henle are not locations for cast formation. • Hyaline casts are composed primarily of a mucoprotein (Tamm-Horsfall protein) secreted by tubule cells. Casts The factors which favor protein cast formation are: *low flow rate, *high salt concentration, *low pH, all of which favor protein denaturation and precipitation, particularly that of the Tamm-Horsfall protein. Hyaline casts can be seen even in healthy patients cylindrical,colourless homogeneous and transparent Yellowish - orange colour Granular cells (WBCs) in a clear matrix Granules form from degenerating cells or solidification of plasma proteins How many casts do you see? Crystals • Crystalluria indicates that the urine is supersaturated with the compounds that comprise the crystals, e.g. ammonium, magnesium and phosphate. Common Crystals in Acid pH • Amorphous urate – Orange powder – May clear with warming or saline • Uric acid – Brown lemon shaped or star shaped – Birefringent with polarized light • Calcium oxalate _Colorless retractile ,octahedral ,envelope-like structure. Amorphous Urate Uric acid Uric Acid Calcium Oxalate and Epi 61 Calcium Oxalate 62 Common Crystals in Alkaline pH • Amorphous phosphate – White powder – May clear with saline • Triple phosphate _ in the form of prisms _ dissolve when urine is made acidic • Calcium carbonate _ in the form of granules, spheres or rarely dumbbell-shaped . Amorphous Phosphate Triple phosphate Triple Phosphate Calcium Carbonate