You will role-play providing patient education - English-for
advertisement

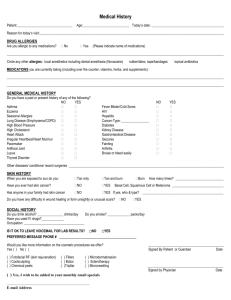
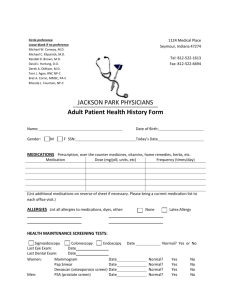
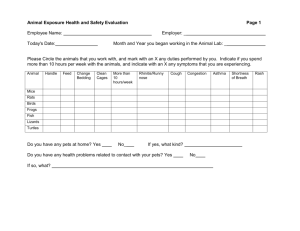
CELBAN Role-plays Dermatology Role-play1 Parent of baby Child: Noah McCallum, 9 months old Came in because of Severe rashes; low grade fever for the last week, lethargic. Red, itchy (scratches), weeping, sometimes slightly hot, maybe infected. Especially on face, legs, arms, stomach…sometimes back. Father: Sam McCallum, 35, allergies, high blood pressure, teacher Mother: Janice McCallum, 36, asthma, eczema Siblings: Older sister (Sally), 9, allergies (peanuts), asthma, psoriasis Older brother (Joshua, 4), a few mild allergies (cats) History: Doesn’t sleep more than 3-4 hours at a time… No other diagnosed problems… but sometimes seems colicky – maybe asthma. And perhaps has allergies… Not on any medications. Except baby Tylenol when has a fever… happened 4x. Except on antibiotic cream when rash seems infected. Food: Nurses 6 times a day… Started solid food at 7 months. Now eating some veggies and rice cereal, cherios…. Mood… cries a lot… generally seems uncomfortable Weight : seems to be gaining weight normally… average on chart during monthly checkups at health centre Growth: Length… a little short for age…but has been since birth Pain: I don’t know… He cries a lot…often can’t be comforted. Seems uncomfortable. 1 Note: This activity could be used as the Speaking mid-term Exam, with the instructor or volunteer taking the role of the client and evaluating the students using the Evaluation Tool for Role-play. Students should use the Pediatric Clinic Assessment Form to guide their interview. Dermatology Role-play2 9 year old girl Child: Sally McCallum, 9 years old Came in because of Red, scaling, flaky skin over large patches of her body, especially on face, legs, arms; parts hot and red. Low fever, comes and goes. Tried moisturizer, and antibiotic creams but it doesn’t go away. Father: Sam McCallum, 35, allergies, high blood pressure, teacher Mother: Janice McCallum, 36, asthma, eczema Siblings: Younger brother (Joshua, 4), a few mild allergies (cats) Younger brother (Sam, 9 months), rashes History: Eczema (moisturizer usually works, sometimes antibiotic creams), allergies, esp. to peanuts (epi-pen) asthma Puffers: salbutamol and flovent Food: normal appetite; but perhaps eats too much junk food when feeling depressed. Mood: embarrassed; kids tease her. Doesn’t feel like joining in on activities – especially PE. Weight : slightly heavy – 60 pounds Growth: normal Pain: just itchy 2 Note: This activity can be used as the Speaking mid-term Exam, with the instructor or volunteer taking the role of the clients (alternating different clients), and evaluating the students using the Evaluation Tool for Role-play. Students should use the Pediatric Clinic Assessment Form to guide their interview. Intake Interview: Preparation worksheet In preparation for an intake interview role-play, you will invent an imaginary client whose role you will play. Search the illness or condition you have been assigned on health.yahoo.com, in combination with the terms “symptoms” or “when to call the doctor.” Use the information you gain to complete the following worksheet: Disease/Condition:_______________________________________ 1. Choose 3-4 of the symptoms listed to be your presenting symptoms. These symptoms are the reason you are seeking medical attention: ______________________ ____________________ _____________________ 2. Now, list 4-5 additional symptoms – these will be symptoms that, if the LPN asks the right questions, will come up during the intake interview. 3. Now think of 1-2 other on-going problems you have (Note: these are not the reason you are seeking medical attention, and these conditions may or may not be related to your presenting symptoms). 4. Make a list of medications you are on, including dosage and frequency. 5. Now fill in additional details for your character (if it is a baby or very young child that is sick, you may play the role of parent): Client name:______________ Age_________ Gender________________ Family, including health of parents/siblings 6. Other relevant details: Language for Giving Instructions Use sequence markers: Some stronger phrases for giving instructions: First, ___ We need you to___ Then, ___ You’ll have to___ After that, ___ You have to___ Next, ___ You’ve got to___ After you do___, you can… When you’ve finished (doing something), ___ Oh, and before you ___, you should ___. Emphasize important points: Make sure you… Make sure you don’t… Use suggestion forms to sound polite: Don’t forget to… It’s a good idea to___ Be sure to… You might want to___ Be sure you don’t… You could/can___ You’d better… Why don’t you___ It’s (very, extremely) important to… Could/can you ____ It’s urgent/important/necessary that you… Never… Use the imperative (sparingly): It can sound a bit “bossy” – but sometimes that is the tone you’ll need! Then, check their comprehension: Always… You should never/always… Does all that make sense? Are you still with me? Do you have any questions so far? Any problems yet? 1. Think of a nursing procedure that you are very familiar with. Imagine you are teaching a nursing student or a caregiver how to do that procedure. Practice giving those instructions to a partner, using sequence markers and suggestion forms, and emphasizing important points. 2. Imagine that later, the student/care-giver makes a number of mistakes (perhaps forgets an important step) when performing that procedure. Give those instructions again, but use more of the imperatives, stronger phrases and emphasizing phrases. 3. Think of instructions you may have to give a client who is slightly cognitively impaired and uncooperative. Give those instructions using sequence markers, imperatives, stronger phrases, and emphasize important points. Oncology: Providing Client Education You will role-play providing patient education regarding an exam or test that a cancer patient may receive. Step 1: With a partner, search your assigned topic on health.yahoo.com3: Leukemia + bone marrow aspiration and biopsy OR lumbar puncture Colorectal cancer + sigmoidoscopy OR barium enema Cervical cancer + Cervical biopsy OR colposcopy Breast cancer + MRI of the breast OR breast biopsy Prostate cancer + prostate biopsy Step 2: Take notes: You will be providing education to a patient with the condition you researched. What kinds of things will you need to know? What kinds of things might s/he ask you? Take notes here: Step 3: Role-play The patient knows s/he has or might have the condition you researched. Your job is to inform the patient that the doctor has recommended s/he have a __________________, and then provide information on the test to reassure the patient. Your patient teaching should include: 3 Introduction + small talk + explanation of why you are there. A question which introduces the topic (e.g., So, do you know what is involved with a cervical biopsy? Have you ever had a barium enema? Would you like me to explain what will happen during the test?) An explanation of test (why s/he is having it, what will happen, what precautions to take, etc.) Response to the patient’s anxieties, fears, and questions. Google “Yahoo! Health,” select “Conditions,” and then search your terms (you will need to search both the condition and the test). Pediatric Assessment Role-play #1: Teen Girl (Speaking/Writing) Student A: Client: Rachel James Student B: LPN You have come to a pediatric clinic with your parent because you’ve not been feeling well: always feeling cold, headaches. Answer the nurse’s questions with the following information (only give details when s/he asks probing questions): You are Rachel James, 14 years old, grade 9, missing school probably 2-3 times a month. Interview the client to fill in the pediatric clinic assessment form. Afterwards, explain that the doctor has requested a blood test to check her thyroid: Father: Peter James, 42, no health problems, Owns own art store Mother: Marcie James, 42, hypothyroid, substitute teacher Siblings: Brother (Jeremy James), 12, no health issues She’s afraid of blood tests… explain what will happen during the blood test. Give suggestions for dealing with the school regarding wearing warmer clothes. Explain that the mood swings may be related to normal hormone levels changing. Even though menstruation hasn’t happened yet, hormones can cause mood swings. Give some suggestions for dealing with the mood swings. Sister (Anita James), 9, allergies (shellfish), asthma You have a history of asthma, eczema, and allergies…to mould, farm animals, peanuts. You are on the following medications: Anemia when you were 2 – seemed to be related to high lead content. Not an issue now. Came in for an appointment because of mood swings (for about a year – you lose your temper a lot…get unreasonably angry. Then you feel very depressed.) Always feeling cold (chronic, but a bigger problem since September). You feel cold even when everyone else in your school is fine…no one else is cold. Hands freezing – sometimes feel numb. You’d like to wear your coat, hat, fingerless gloves at school, but not allowed. You dress warm, always! Lots of headaches and general aches (this last month). Food: you eat a lot of fruit and veggies, not much meat. Fast food maybe once a month. Junk food – maybe just a little once a week. No pop. Weight gain: Gaining a little bit…strange because you don’t eat much. Growth: didn’t grow much...short for age Development: has not started period… some breast development Pain…on a scale of 1-10, where 10 is unbearable… headaches are about a 3 – it’s that they last a long time. Today it’s just a 2 – you can ignore it, but when you are bored, you notice it. Stress: Yes…get stressed about everything…High marks. Other: Not much exercise…don’t feel comfortable because of the asthma and allergies. **You can’t remember ever having a blood test…and the idea of a blood test frightens you. Pediatric Assessment Role-play #2: Pre-teen Boy (Speaking/Writing) Student B: Client: Jonathan Masters Student A: LPN You have come to a pediatric clinic with your parent because you’ve been experiencing severe headaches. Answer the nurse’s questions with the following information. Only give details when s/he asks probing questions. You are Jonathan Masters, 12 years old, grade 7, missing school probably 2-3 times a month. Interview the client to fill in the pediatric clinic assessment form. Afterwards, explain that the doctor has suggested he get a CT or MRI scan (choose whichever one you are most familiar with): Father: Jim Masters, 45, migraines, high blood pressure, Nurse Mother: Sandi Masters, 42, allergies, asthma Siblings: Older sister (Sally), 15, allergies (severe, peanuts) Little brother (Liam, 9), a few mild allergies (cats) History: You have a history of allergies – but nothing severe like your sister’s peanut allergy. Just to cats, mould, horses, like your brother. You aren’t on any medications, other than pain medications. You generally take Advil – sometimes 2-3 gel tablets (mg?) Came in for an appointment because of Severe headaches. You’ve always had headaches… you remember having headaches when you were in kindergarten… would cry and tell your parent you had headaches. But they are worse now (last 2 months). Sometimes vomiting. Sometimes dizzy. See spots. Usually you can’t function. Pain starts around nose and eyes – behind eyes, moves to temple and whole head. Usually you stay home from school. You were on a sports team (basketball), but had to quit because you missed too many practices. Pain: Right now, on a scale of 1-10, where 10 is unbearable… you would say a 6 or 7. Sometimes, though, a 10. That’s when you stay home from school. Food: Normal… balanced, although you don’t like vegetables. Fast food maybe once a week. Some junk food – chips, pop, maybe 2-3 times a week. Stress…yes…grade 7 is different from elementary school – hard to learn to get to different classes in only 3 minutes. Each teacher gives homework – sometimes they don’t talk and so it’s too much. But you like it better than elementary school. The teachers are better. Weight gain: no… 1. Explain what happens during the scan. 2. The doctor has given a prescription for a stronger headache medication. Explain how to take it. 3. Explain the doctor would like him to keep a headache diary to see if there are any “triggers” which can be identified. When he has a headache, he should list the following: o what he ate in the last 5 hours o any emotional stresses (e.g., test, argument) o what you were doing in the hours before the headache started (e.g., delivering flyers, playing a computer game, homework). Growth: 3rd tallest boy in the class. Other: Now that off the team, not much exercise. Delivers flyers 3x a week. Likes to play computer games. Pharmacy Roleplay: NSAIDs (Speaking/Writing) To prepare for your role as a GERIATRIC PATIENT (who is on a variety of medications), think through the following questions.4 7. Name Age Living situation Family support 8. Reason for admission (e.g., a fall, broken __, stroke, etc.) 9. Make a list of 3-4 prescription medications you are on, including dosage and frequency and why you are taking these medications. Be sure that some of these medications are NSAIDs.5 10. List one or two over-the counter NSAIDs that you are taking, but don’t tell the LPN about them unless s/he specifically asks you. In your role as LPN, you will take a patient history to fill in the following form. Think through the questions you will need to ask to elicit the correct information. NOTE: During the interview, if the LPN uses any medical terminology (e.g., what is the route?), ask for clarification or don’t answer. 4 However, don’t easily volunteer all of these at once. You will need prompting from the LPN to help you remember everything. 5 Co-worker conversations: Being tactful and professional Situation 1. Your supervisor is telling you, once again, about a meeting scheduled for Monday morning at 8:30. She’s mentioned it more than 4 times (AND she sent you an e-mail). 2. You just finished putting in an IV – no problem at all – you’ve done this many times in your country of origin, and a few times here. Your supervisor comes up and asks “How did it go, putting in that IV? Did it go alright?” 3. You stop in the hall to talk to an acquaintance you haven’t seen for a long time. Your supervisor comes by and says, “What’s going on? Don’t you have something you should be doing?” Brainstorm for 4 different reasons for the supervisor’s comments. Brainstorm for one possible response. What might be a consequence of that response? 4. Your supervisor criticises you, in front of your coworkers, for not sending her a copy of a poster announcing a Christmas party, prior to posting it. She held up the poster and said “What’s this?! Who approved of this?! You can’t put this up without my approval!” Co-worker conversations: Language for giving and receiving criticism…professionally! When you have to confront someone… Don’t lose your cool! When someone criticizes you… Approaching the person: Don’t lose your cool. Stay calm and professional. Speak to the person privately: “Hey, Marie, could I talk to you a moment?” “Marie, do you have a minute (to talk)?” If the person is with someone else, you could ask “Hi, do you mind if I steal/borrow Marie (or ‘your nurse’) for a moment?” You may choose to begin tactfully (especially if you are speaking to a superior, or if you think the person has no idea s/he is doing something wrong) 1. Use softeners (um, well, just, maybe, seems, could, might, potentially, possibly) 2. Use rising intonation to indicate reservation and show politeness. 3. Use “we” instead of “you” (How about if we…? Could we maybe…? Perhaps we could…?) 4. Ask questions which express concern, but that allow the other person to re-evaluate the situation. (What about…? Do you think __ might…? Don’t you think ___ might…? Could __ possibly…?) 5. Use the “sandwich” method: compliment, criticism, compliment. However, you may choose to approach the issue more assertively, if you are dealing with a serious issue or if the person has not responded to a tactful approach. 1. 2. When you are being criticised, try to get to the real issue. Ask for clarification. I’m sorry. What do you mean by…? I’m sorry…I’m not sure what you mean. How could I have done this differently? So, what is it exactly that you want me to do here? Indicate attention, respect and understanding. Eye contact Nodding Verbal cues (ok, ok, mmhmm, all right) Paraphrasing: So, you’re saying I should… OK, so I should… Use phrases to emphasize importance (you can combine them with softeners from #1 above) It is imperative (OR extremely important) that you… Explain yourself politely, but assertively Make sure you (always)…. Be sure you don’t/never… Do you mind if I say something? Don’t forget to… It’s a good idea to… Could I explain why I did it that way? Really listen – the person you are arguing with may have a good point. Be willing to back down if you are convinced (e.g., “Oh, OK, that makes sense”). Actually, I’d like to point out that… Co-worker conversations: Practice giving and receiving criticism You are the charge-nurse in a long-term care facility and you notice the problems listed below. What would you say? 1. In a small group, discuss how you would respond to the following situations. 2. With a partner from a different group, take turns in the role of Charge Nurse and role-play the situation. 1. One of your employees keeps bringing her 4 year old son to work. The first time, her husband dropped off the son ½ an hour before the end of the shift – that was OK. Then a few days later, he was dropped off 1 hour before the end of the shift. Now it seems that 2-3 times a week, the son is dropped off 1-2 hours before the end of the shift. The child is wellbehaved and plays quietly, but you don’t think this is appropriate. 2. One of your new staff, a young woman (in her early 20’s), wears her headphones while she is working with clients – clients and other staff are complaining. Besides that, she is doing an excellent job. 3. One of your staff did not turn up for work yesterday. No one could get a hold of her, and everyone had to work short until you found someone to come in at overtime for 4 hours. Today, when you asked where she was, she said she’d gone to Calgary for the weekend to visit a friend and decided to stay an extra day. You are upset because she didn’t bother to phone How would you approach the person? Remember, do not lose your cool Avoid insulting the person and their profession. Use questions to point out the problem, and softeners if you are trying to be tactful. Be clear and tactful, and use phrases for emphasizing importance. and let anyone know. 4. You walk by a room and hear a patient shout “NO, I’m not getting up now! Leave me alone!” Then you see your staff member pull the covers off the patient, throw them on the chair, and say threateningly, “When I tell you to get up, you get up! NOW! 5. Other staff members are complaining about one of the other staff – they say that she smells bad and they don’t want to work with her. Some patients have mentioned the problem as well. 6. Your staff is making life very difficult for a new receptionist who has just been hired. She is very different from the previous receptionist (who had been very outgoing, and would arrange activities, such as baking cookies, for the clients). They complain to her, and they complain about her to you. She is very frustrated and is thinking about quitting. Talk to the other staff. 7. Make up your own scenario:
![Pediatric Health Histroy.Initial child.d[...]](http://s3.studylib.net/store/data/006593866_1-7ecae25d724665d2a564380f86b41e96-300x300.png)