Document
advertisement

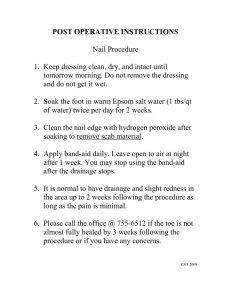
Dermatosurgery Digital Lecture Series : Chapter 27 Dr. Venkataram Mysore Director, Venkat Charmalaya Centre for Advanced Dermatology and Postgraduate Training, Bengaluru Contributors : Dr. Sindhu Potla, Dr. Subodh D. Jane, Dr. Madhulika Mhatre, Dr. Gayatri N. Khatri, Dr. Vani Yepuri, Dr. Vijayalakshmi S. P., Dr. Namitha Chathra CONTENTS Introduction Nail surgery Electrosurgery Vitiligo surgery Radiofrequency Hair Restoration surgery Cryosurgery Liposuction Chemical cautery MCQs Local Anaesthesia Photo Quiz Excision and Suture Acne surgery Dermatosurgery Dermatosurgery has made major advances in the last two decades. Major contributions have been made by dermatologists to these field. Generally these are done under local anaesthesia. These include basic surgeries such as electrosurgery, acne surgery, and advanced surgeries such as vitiligo surgery, hair transplantation and liposuction. Electrosurgery The term “electrosurgery” is a general term to describe the different procedures employing electrically generated heat. Methods of Tissue Destruction : The heat production results in tissue destruction by enzyme deactivation, RNA and DNA destruction, cell wall damage, protein coagulation, and steaming of water content (dehydration or cell explosion). Types of Electrosurgery : Electrofulguration Electrodessication Electrocoagulation Electrofulguration : Charring of superficial tissue is caused by sparks from the electrode without actually touching the tissue. The tissue destruction is rapid with cell dehydration and necrosis. Electrodesiccation : It involves touching the lesion with the electrode. The current intensity is marginally higher than in fulguration. The tissue destruction is deeper, superficial mummification and necrosis of cells occurs after initial dehydration. Electrocoagulation : The lesion may or may not be touched depending upon the depth of tissue destruction required. Deep necrosis and coagulation occurs with a hyalinized appearance. Thrombosis of midsized vessels (1–2 mm) also occurs. Electrosection : Used to cut a tissue rather than produce only destruction. The advantage is simultaneous hemostasis due to vessel coagulation. Paradoxically, this is also the drawback, since greater tissue destruction and subsequent delayed wound healing occurs due to poor vascularity. Electroepilation : Destruction of the hair follicle using an electric current. Truly permanent method of hair removal. Indications and Contra-indications Indications : Benign : Warts, acrochordons, dermatosis papulosa nigra, seborrheic keratoses, freckles, lentigines, mucosal and sebaceous cysts, spider angioma, cherry angioma, pyogenic granuloma, syringomas, trichoepitheliomas, xanthelasma, nevus sebaceus, etc. Premalignant : Actinic keratoses and Bowen’s disease. Malignant : Small basal cell carcinomas and squamous cell carcinomas. Contra-indications : Keloidal tendency, local infection, and cardiac disorders (especially if the patient is on a pacemaker), petit mal epilepsy. Radiofrequency Uses radio waves at a frequency of 3.8 mHz. Superior to electrosurgery as it has a coagulation mode, causes less heating and therefore less scarring. Used to treat a number of benign growths and some malignant growths. Also used in aesthetic indications such as blepharoplasty and resurfacing. Cryotherapy Cryosurgery is that branch of therapeutics that makes use of local freezing for the controlled destruction or removal of living tissues. Cryogens and their effective temperatures Saltice –20°C Carbon dioxide slush –20°C Fluorocarbons (Freon) –30°C Carbon dioxide snow –79°C Nitrous oxide –75°C Liquid nitrogen –20°C (swab) or –196°C (spray/probe) Mechanisms of Action (Cryonecrosis) Ice formation : Extracellular ice damages the cell membranes and intracellular damages the mitochondria and endoplasmic reticulum. Osmolarity changes : Extracellular ice causes decrease in extracellular water and a resulting increase in the solute concentrations causing cell membrane disruption. Thermal shock. Denaturation of lipoprotein complexes. Vascular changes : Ischemic necrosis starts around the vessels as a result of microthrombi within the capillaries and arterioles. Cryoimmunomodulation : low temperatures can induce effective immune recognition of the remaining viral or tumor cells. Indications and Contra- indications Indications : Warts, molluscum contagiosum, cystic acne, acne scars, keloid, granuloma pyogenicum, skin tags, seborrheic keratosis, and mucoid cyst, leukoplakia, Bowen’s disease, erythroplasia of Queyrat, and actinic keratosis, basal cell carcinoma, basal cell nevus. Contraindications : Agammaglobulinemia, cold intolerance and cold urticaria, cryoglobulinemia, cryofibrinogenemia, Raynaud’s disease, pyoderma gangrenosum, multiple myeloma, concurrent treatment with immunosuppressives, and patients on renal dialysis. Methods of application : Dipstick technique, Spray technique, Cryoprobe technique, Cryoroller technique, Cone spray technique. Advantages : Outpatient procedure. Patients of all ages can be treated, even those at poor risk for surgery and general anaesthesia. Multiple tumors can be treated at the same time. Complications are rare and cosmetic results are excellent. Lesions on sites with poor skin mobility that are difficult to excise can be treated. Disadvantages : Postoperative edema Pigmentary changes Chemical Cautery The process of cauterization is carried out by using heat, cold or chemicals. When chemical agents are used to carry out this process it is called chemical cautery. Commonly used chemical agents : Trichloroacetic acid Phenol Podophyllin KOH Salicylic acid AgNO3 Formalin Local Anaesthesia Analgesia restricted to particular area or field of interest without causing any impairment of consciousness and cognizance. Most of the dermatosurgery procedure are performed under local anaesthesia. Mechanism : Local anaesthetic agent (LAA) inhibits nerve conduction by blocking the sodium channels. Adrenaline can be added to improve the efficacy and duration of action of LAA. Vasoconstriction at the site of LAA administration leads to delayed local clearance and increase in duration of local anaesthesia. (Adrenaline, 1:2,00,000). Classification and Mode of administration Classified based on chemical structure • Ester (-COO-) • Amide (-NH-) Esters : Cocaine, Procaine, Chloroprocaine, Benzocaine & Tetracaine. Amides : Lignocaine, Prilocaine, Bupivacaine, Mepivacaine and Ropivacaine. (Amides contains 2 ‘I’ in the name). Mode of administration : Topical anaesthesia Infiltration anaesthesia Tumescent anaesthesia Nerve block Topical Anaesthesia Method of application of LAA over skin or mucosa to cause anaesthesia. Eutectic mixture of local anaesthetics (EMLA) • Prilocaine 2.5% + Lidocaine 2.5% • Lidocaine 7% + Tetracaine 7% Superficial skin procedures - shave biopsy, skin grafting and laser procedures. Maximal safe dose for 70 kg adult - 300 mg for lidocaine and 50 mg for tetracaine. Infiltration Anaesthesia LAA is injected directly into the tissue of interest without considering the course of the nerve supplying it. Lignocaine is the most commonly used LAA. Safe limit of lignocaine • 4.5 mg/ kg without adrenaline • 7 mg/kg with adrenaline Adding adrenaline decreases blood loss, reduces the toxicity and increases the duration of action. Modifications (Infiltration Anaesthesia) Ring block : LAA is infiltrated all around the area of interest but not into it. Field block : LAA is injected subcutaneously to anaesthetise area distal to the site of injection. larger areas can be anaesthetised with lesser quantity of LAA. Regional block: Infiltration of LAA around a nerve or nerve plexus of hands, foot, fingers, toes and face. Tumescent Anaesthesia (TA) Newer method of local anaesthesia, used in several dermatosurgical procedures, particularly liposuction. LAA + Adrenaline + Saline mixture is used. Safe upper limit of lidocaine administration is 55 mg/kg body weight. In TA, rate of absorption of is slow, hence leads to smaller peak values and lesser toxicity. 0.05–0.1% lignocaine and 1:100,000 –1.5:100,000 adrenaline are used. 10 mEq of sodium bicarbonate is added to 1 liter of solution to prevent stinging (due to acidic pH). Nerve Blocks Simple procedures that, can be carried in an outpatient setup. Small quantities of LAA anaesthetize large areas. Good knowledge of anatomy is required to prevent complications like intravascular injection or nerve laceration. Used in full face dermabrasion, vitiligo surgery on hands and feet, partial or total nail avulsion and hair transplantation. Complications of local anaesthesia Syncope Secondary to vasovagal attack Hypersensitivity Reactions Skin testing is required Methemoglobinemia Intravenous administration methylene blue is the treatment. Cardiovascular Toxicity • Ventricular arrhythmias and myocardial depression. • Rarely caused by commonly used LAA. • Mostly caused by Bupivacaine. Others : Bruising and Myonecrosis Excision The elliptical excision is the mainstay of dermatosurgery. Steps : • Proper planning of ellipse • Clear excision with dissection of lesion • Undermining of defect • Achieving hemostasis. Good understanding of anatomy, wound healing, lesion biology and RSTL’s is important. Types of Excisions Simple excision without suture (small lesions). Elliptical excision with suture (mod-large lesions). Excision with grafting or rotation flap (large malignant lesions). Punch excision (with or without suture). Planning of Ellipse Length: Width ratio - 3:1 Angle at tips : 30 degrees Parallel to RSTL Long axis of lesion parallel to long axis of excision. Malignant lesion : larger margin Tips in Excision Hold scalpel handle perpendicular Incise perpendicular through dermis to subcut tissue Pass blade parallel to hair follicle to avoid resection Avoid cross hatching Tips in Excision Avoid boat shaped incisions Ensure uniform depth of tissue removal, to avoid pseudo-dog ears. Suturing The ideal suture should be sterile, easy to handle, have high tensile strength, favorable absorption profile and uniform diameter and size. Types : • Absorbable and Non absorbable • Natural or Synthetic • Braided or Monofilament • Antibacterial Sutures Absorbable : Catgut, chromic, catgut, vicryl and dexon. Non absorbable : Silk, prolene, nylon and Dacron. Tips in suturing Regarding the knot strength, generally four throws are given Knot should not be placed in incision lines Knots should be small and the ends cut short (2-3 mm) Suture should not be tied too tightly as tissue necrosis may occur. Proper undermining of wound to prevent dog-ears post suturing Avoid high wound tension as it may lead to hypertrophic scarring Sutures should be removed in 7 to 10 days Characteristics of commonly used suture materials Filament type Nylon Polypropylene Polyester Polyglactin Gut Chromic Gut Fast Gut Mono Mono Multi Multi Mono Mono Mono NA NA NA 60-90 d 10-40 d* 15-60 d* 3-5 d Black Blue White White Tan Tan Tan Time required for absorption Color Common Use General General More Advantages secure knots Strength Tendon Buried Used in Dissolves tendons slowly Children’s skin Dissolves * In the mouth, plain gut absorbs in 3 to 5 days and chromic gut in 7 to 10 days Tongue Dissolves more slowly Children’s face Dissolves more quickly Choice of suture according to area Techniques Suturing technique Simple interrupted : Uncomplicated wounds Vertical Mattress : Causes approximation with minimal tension - used for wounds where tension is expected. Horizontal Mattress : Provides added strength in fascial closure. Continuous Suture : Provides rapid closure. Subcuticular Sutures : Ideal for linear cosmetic closure. Acne Surgery Acne scars are classified as atrophic (rolling, ice pick, boxcar scars) and hypertrophic. Treatment has to be tailored as per the type of scar. Fibrotic bands Surgical Approaches Microneedling Subcision Punch techniques • Punch excision • Punch floatation • Punch replacement grafting CROSS (Chemical Reconstruction Of Skin Scars) Dermal grafting Dermabrasion Scar revision techniques (Z, M and Y plasty) Microneedling Principle : Tiny micro-injuries in the upper dermis trigger the wound healing cascade including numerous growth factors which leads to a increased production of dermal collagen and elastin by the fibroblasts thus causing tissue remodelling. Indication : Boxcar scars and rolling scars. Method : • Topical anaesthetic cream is applied on the affected area for 45min. • After cleaning the area , the skin is stretched and the dermaroller instrument is rolled to and fro in 4 directions till pinpoint bleeding is seen and then the face is washed with water. • The session is done 4-6 times after an interval of 4-6 weeks. Microneedling principle Microneedling instrument (Dermaroller) Microneedling technique Subcision Indication : Rolling acne scars Principle : Releasing fibrotic bands underlying scars . Organization of blood in the induced dermal pocket. Connective tissue formation in the area. Method : Anaesthesia given subcutaneously with lignocaine and adrenaline. 18 gauge Nokor needle is inserted in the periphery of scarred area just below the dermal subcutaneous junction plane and gently swept across the site, thus breaking the fibrotic bands. Subcision principle 18 gauge Nokor needle and Subcision Punch techniques Principle : All punch techniques remove a pitted scar with a small rim of normal tissue. Punch excision Indications : Ice pick ,deep boxcar scar less than 3.5 mm in dia. Method : Done under local anesthesia. Scars are excised with a biopsy punch and the skin is sutured. Punch floatation Indications : > 3mm boxcar scar that has no significant colour and textural abnormalities. Method : Punch sized to match the inner diameter of the scar is selected and punch is performed. Plug is elevated and positioned to lie slightly higher than the surrounding skin and the punch is secured by tissue adhesive. Punch floatation Punch replacement grafting Principle : Technique is similar to that of a punch floatation, but replaces the plug with a donor plug instead of elevating the original defect. Donor plug obtained from the postauricular area or inner arm. Indications : Deep, irregular pits and tethered boxcar scars with altered skin texture. Chemical Reconstruction of Skin Scars (CROSS) High strength TCA (trichloroacetic acid) is used focally on the atrophic scars to induce collagenization. Principle : TCA causes precipitation of proteins, coagulative necrosis of cells in the epidermis, and necrosis of collagen in the papillary to upper reticular dermis. Indications : Ice pick scars . TCA Cross Method : Skin is stretched and TCA applied with wooden toothpick upto bottom of the scar . After 10-15 secs frosting can be seen and then face is washed with water. (Repeated at 3 week interval for 3-4 sessions). Dermal grafting Dermal graft is a skin graft from which epidermis and subcutaneous is removed. Principle : Placement of dermal grafts into precise pockets under the skin after subscision. Indications : Rolling scars Method : After subcision, dermal graft is placed in the defect. Dermal grafting Dermabrasion Principle : It involves mechanical removal of layers of skin (restricted to upper reticular or mid - reticular dermis) by manual or electrical motorized abraders (diamond and steel brushes) and further allowing this wound to heal by secondary intention so as to achieve resurfacing effect. Limitations : As it is an invasive procedure involving long healing time and increased morbidity, it is largely replaced by laser resurfacing. Dermabrasion Equipment Diamond brushes Dermabrasion machine Manual dermabrader Nail Surgery Nail surgery requires thorough knowledge of anatomy , physiology and pathology of nail complex. Along with surgery skills, good anesthesia, aseptic precautions and good light, nail surgery has excellent outcome and gives satisfactory therapeutic / diagnostic results. Nail anatomy and blood supply Anatomy of nail unit Blood supply of nail Indications Diagnostic Exploration of the nail bed and the nail matrix : Inflammatory dermatoses, infections, connective tissue diseases and tumors. Performing biopsy : psoriasis, lichen planus, twenty nail dystrophy, nail unit tumors, nevi, melanonychia and pachyonychia congenita. Therapeutic Ingrown toe nail/onychocryptosis Chronic onychomycosis Traumatic nail injuries Chronic paronychia Pincer nails Myxoid cysts Subungual or periungual verruca Retronychia Tumours - glomus tumour, onychomatricoma Miscellaneous - melanoma and non melanoma cancers, pyogenic granuloma etc. Contraindications Peripheral vascular disease Collagen vascular disease Uncontrolled diabetes mellitus Disorders of hemostasis Acute infection or inflammation of the nail unit, including the surrounding paronychial tissues Instruments General instruments Binocular magnifier loupe Delicate adson’s forceps Castro veijo scissors Double prong Guthrie retractors Delicate needle holders Stevens scissors Straight mosquito forceps Curette Digital tourniquet Specific instruments Nail elevator- freer septum elevator/dental spatula English anvil-action nail splitter Nail nipper Instruments Instruments include fine curved (Castro Veijo's) scissors, fine curved forceps, nail spatula, nail splitter, and disposable biopsy punches (3 mm and 4 mm). Preoperative work up and Anaesthesia Proper history and diagnosis Clinical examination History of drugs that interfere with hemostasis Counsel and explain the patient Proper photographs and consent mandatory Anaesthesia Distal nail blocks • Distal digital block(wing block) • Distal anesthesia through PNF • Distal anesthesia through hyponychium Proximal digital blocks Transthecal digital anesthesia Regional blocks Nail surgery Procedures Nail Surgery Procedures Nail plate avulsions - complete/partial Nail plate repositioning Proximal nail fold reflection Nail biopsy Matrixectomy Nail avulsion is the most common surgical procedure Paring the nail plate is the process of taking off pieces of the nail in a transverse or longitudinal fashion to fully observe an involved area on the nail bed, performed in subungual or periungual verruca. Nail avulsion Excision of the body of the nail plate from its primary attachments, the nail bed ventrally and the PNF dorsally. The 2 primary methods of nail avulsion are distal avulsion and proximal avulsion. Nail avulsion can be partial or complete Indications – onychocryptosis, excision of tumours, for examination of underlying pathology, preliminary step in nail biopsy, therapeutically in fungal and bacterial infections, trauma. Partial nail avulsion a: nail plate is detached from nail bed b: cutting of nail plate to be removed with splitter c: nail plate removed with sweeping movements d: phenolisation to destroy matrix Biopsies of nail includebiopsy of nail bed, nail plate, nail matrix, nail fold and nail unit. Intra-operative Bloodless field is mandatory. For simple avulsions lateral digital pressure suffices. Commonly digital tourniquet at the base of the finger is used. Tourniquet should not applied for more than 15 mins at a stretch. Electrocoagulation should be avoided. Post-operative care Postoperative care is essential for a successful nail avulsion. Non-adherent, highly absorbent dressing is ideal. The lateral grooves may be studded with either a paraffin gauze or an antibiotic tulle. Dressing is removed after 24 h after soaking in warm water or saline. Povidine-iodine solution application may promote the healing process. The operated limb is kept elevated so as to minimize the pain and swelling. Minimal activity is recommended, especially if toenails are avulsed, for at least 2 weeks. Complications Complications are seldom and may result from nail matrix damage Pain - most common. Allergy to anaesthetic Minor wound discharge Infection Hematoma Nail deformity Mal-alignment Nail impaction (distal embedding) Local spicule growth Vitiligo surgery Indications Stable vitiligo • Absence of new lesions • No extension of old lesions • Absence of Koebner’s phenomenon Refractory lesions Secondary leucoderma Piebaldism 1 year Test-grafting : transplantation of few grafts on to the recipient area before the main surgical procedure. The test grafts are then observed over some time to see the repigmentation response. Types of vitiligo surgery Therapeutic wounding : to stimulate the melanocytes from the periphery and hair follicles. e.g. Therapeutic dermabrasion, laser ablation, cryosurgery, needling, local application of phenol or TCA. Grafting techniques : Repopulation of the depleted melanocytes by various grafts. e.g. Ultra-thin grafts, Suction blister graft, Miniature punch grafts, Cellular transplants (cultured and non-cultured). Tattooing : Uniform implantation of minute, metabolically inert, pigment granules into the dermis, to create permanent camouflage, using manual/electrical needles; depth of deposition is 1.5mm, in the upper & mid dermis. Excision with primary closure : removal of the depigmented areas. Suction Blister Technique Donor site : Application of a prolonged suction at a negative pressure to produce split at Dermo-Epidermal Junction. Blister is cut all along its border, anchoring filaments & coagulum scraped, split thickness skin grafts containing only epidermis obtained. Recipient site : Transplant epidermal sheet to dermabraded/laser ablated vitiligenous patch. Tulle & dressing, removed 10-12 days. Course of graft • Melanocyte transfer occur by 48-72 hrs • Grafts either dries or gets macerated • Complete regimentation after 2-3 months Miniature punch grafting Donor site : Take miniature skin punch grafts of sizes 1.5, 2, 2.5 mm with cylindrical skin biopsy punches. Recipient site : Individually insert donor grafts in the punched out chambers (same size as donor site) spaced 5 to 10 mm apart. Place grafts all along the border and at the same level as adjacent skin, pressure dressing. Pressure dressing (after 24 hrs check if any grafts have shifted) for 8 to 10 days. Peri-graft pigmentation starts by 1 month & gradually increases to cover entire patch in 3 to 6 months. Test Grafting Miniature punch grafting Thin Thiersch’s split thickness skin grafting Donor site : Obtain split thickness skin grafts, consisting of epidermis & part of papillary dermis from thigh/gluteal area/ abdomen. Ultra Thin Skin Grafting : contains epidermis & uppermost part of superficial papillary dermis. Recipient site : Dermabrade 2 to 3 mm beyond the border, until punctate bleeding points appear. Lift graft with ring forceps & place it with dermal surface facing abraded bed • Extend 3-5 mm beyond edge Apply surgical glue along edges followed by pressure dressing which is removed after 10-12 days. Graft taken up by 10 days, merges with surrounding skin by 3 months. Noncultured Melanocytes-keratinocyte Transplantation (Autologous melanocyte rich cell suspension technique) Thin split thickness skin grafts trypsinized & incubated at 370c for 50 min. Add 2 ml of Trypsin inhibitor in PBS to discontinue trypsin action. Tease & separate the epidermis from dermis with forceps, cut the epidermis. Add Dulbecco's Modified Eagle's Medium and centrifuge at 2000 rpm for 10-15 minutes. Pellet formed is smeared over dermabraded recepient area, covered with a collagen dressing for 10 days. Pigmentation noticed after 3 wks & blends with surrounding area after 6 to 8 months. Noncultured Melanocytes-keratinocyte Transplantation Before surgery After surgery Advantages Method Tattooing Thiersch’s split thickness skin graft Miniature punch graft Suction blister graft Non-cultured epidermal cell suspension Advantages Instant, inexpensive, no chance of rejection, repeatable, at any anatomical site. Larger areas, Good cosmetic result, Immediate results. Easy & least expensive, 'difficult-to-treat' locations. Pure epidermal graft; no scarring, Good repigmentation. Ten fold large areas can be treated at one time, Excellent cosmetic results. Complications of vitiligo surgery Method Tattooing Thiersch’s split thickness skin graft Suction blister graft Miniature punch graft Complications Leaching, color mismatch, change in shade over time. Graft rejection, stuck-on tyre patch, perigraft halo, scarring of donor site. Ecchymosis, post-inflammatory hyperpigmentation. Cobblestoning, polka dot appearance, depigmented junctional zone, graft rejection, scarring of donor site. Complications of vitiligo surgery Method Complications Therapeutic wounding (Phenol) Scarring Ultra-thin skin grafts Skip areas and depigmented junctional line. Milia, scarring, koebnerization. Non-cultured epidermal cell transplantation Hair transplantation Androgenetic alopecia is the commonest cause for baldness and is largely treated by hair transplantation. Based on donor dominance - occipital hair is androgen resistant and hence regarded as permanent. Principle is to extract these hairs and then implant them in bald area. Two steps: • Donor harvesting • Recipient insertion Done under local anaesthesia. Hair transplantation Concept of Follicular unit (FU) : 1-4 hairs are held together by arrectores as a unit of hairs. Implanting these units is referred to as follicular unit transplantation (FUT). This method allows dense packing and gives natural results- and hence is the gold standard method. Two methods of harvesting : FU strip harvesting. FU extraction. FU strip dissection A strip 1 cm wide (length depending on number of grafts) is taken. Strip is carefully dissected and removed. Strip dissection Wound sutured in two layers to obtain a linear scar. It is important to avoid wound tension to avoid a wide scar. Needs experience to ensure thin scar. Microscopic dissection Microscopic dissection of the strip is essential to ensure minimum damage to roots. Units are separated by careful dissection. Follicular unit extraction A small hole is made for each unit through a punch up to the level of arrectors. This loosens the unit and the unit is extracted with a forceps. Time-consuming, but leaves less scar, and heals faster. Implantation Can be done in three ways : Making all holes and then placing grafts one by one. Making each hole and then placing units. Using special implanters. Results Tumescent liposuction Gold Standard for removal of fat Large amount of fluid with anaesthetic infiltrated in to fat and then aspirated through cannula. Klein has shown that, in tumescent anaesthesia, much higher doses of lidocaine, even up to 45-55 mg /kg weight can be administered. Liposuction removes resistant fat which can not be removed by exercise / dieting. It is safe, done under local anaesthesia. Mechanism - How does tumescent liposuction work? Step 3 Fat after suction Fat before liposuction Step 1 filling fat with 2-3 L of special tumescent solution Step 2 Sucking the fat through small cannulae (2-3 mm pipes) Common areas for liposuction In women : Abdomen, hips, thighs and knees. In men : Flanks, abdomen, breast (Gynaecomastia). Other areas : Chin, arms, neck and face. Instruments Suction apparatus of 1HP power Cannulae for aspiration and infiltration Pressure cuffs for infiltration Procedure Aspiration is done through cannula of different sizes. To and fro motions of the cannula; smooth, fan shaped movements from below to upper layers. Average duration : 1-2 hours depending on the area. Patient goes home with dressings. Patient should come back next day for removal of dressing. Power-assisted liposuction Power-assisted liposuction uses a machine which moves the cannula to and fro and side by side and efficiently removes fatty tissue. Decreases surgeon fatigue, increases precision, in less time, with less bruising and a faster healing time. It also helps in removing tough fat & causes skin tightening. Results Results are seen at 6 weeks Liposuction removes fat in two ways : • By sucking it out • By Damaging it which gets absorbed over 4-6 weeks Once removed fat cells are not regained easily, hence after liposuction the new body’s shape is permanent. There is no hanging of skin post surgery. Since skin is elastic, it returns to its normal state after liposuction. Laser and powered machines induce fibrosis and induce some tightening. However, patient needs to maintain the shape by regular exercise. MCQ’s Q.1) A. B. C. D. Which of the following chemicals are not used for chemical cautery? Phenol Acetone TCA Formalin Q.2) A 26 year old lady has primarily ice pick scars. The treatment of choice is A. Microneedling B. Grafting C. TCA CROSS D. Subcision MCQ’s Q.3) A. B. C. D. Chemical matricectomy is done by use of the following agent 88% phenol 50% TCA 50% glycolic acid 30% Q.4) A. B. C. D. Eutectic mixture of local anesthetics (EMLA) is an example of Infiltration anesthesia Topical anesthesia Tumescent anesthesia Nerve block MCQ’s Q.5) A. B. C. D. Which of the following is the best method to cover larger area Suction blister grafting Miniature punch grafting Tattooing Non- cultured epidermal cell suspension Q.6) A. B. C. D. Which is the gold standard method of hair transplantation Punch transplant Minimicrograft Follicular unit hair transplant None of the above Photo Quiz What is the type of block given in the picture? Photo Quiz Identify the procedure. Thank You!