Day 1 Notes - Roundtable Discussion
advertisement
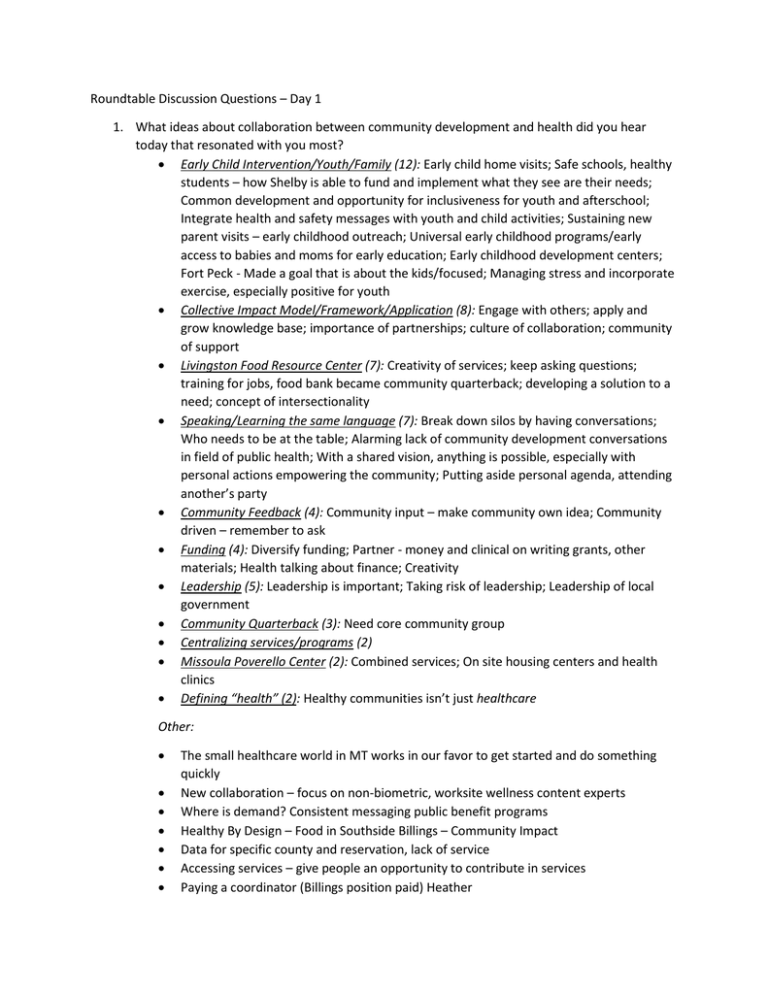
Roundtable Discussion Questions – Day 1 1. What ideas about collaboration between community development and health did you hear today that resonated with you most? Early Child Intervention/Youth/Family (12): Early child home visits; Safe schools, healthy students – how Shelby is able to fund and implement what they see are their needs; Common development and opportunity for inclusiveness for youth and afterschool; Integrate health and safety messages with youth and child activities; Sustaining new parent visits – early childhood outreach; Universal early childhood programs/early access to babies and moms for early education; Early childhood development centers; Fort Peck - Made a goal that is about the kids/focused; Managing stress and incorporate exercise, especially positive for youth Collective Impact Model/Framework/Application (8): Engage with others; apply and grow knowledge base; importance of partnerships; culture of collaboration; community of support Livingston Food Resource Center (7): Creativity of services; keep asking questions; training for jobs, food bank became community quarterback; developing a solution to a need; concept of intersectionality Speaking/Learning the same language (7): Break down silos by having conversations; Who needs to be at the table; Alarming lack of community development conversations in field of public health; With a shared vision, anything is possible, especially with personal actions empowering the community; Putting aside personal agenda, attending another’s party Community Feedback (4): Community input – make community own idea; Community driven – remember to ask Funding (4): Diversify funding; Partner - money and clinical on writing grants, other materials; Health talking about finance; Creativity Leadership (5): Leadership is important; Taking risk of leadership; Leadership of local government Community Quarterback (3): Need core community group Centralizing services/programs (2) Missoula Poverello Center (2): Combined services; On site housing centers and health clinics Defining “health” (2): Healthy communities isn’t just healthcare Other: The small healthcare world in MT works in our favor to get started and do something quickly New collaboration – focus on non-biometric, worksite wellness content experts Where is demand? Consistent messaging public benefit programs Healthy By Design – Food in Southside Billings – Community Impact Data for specific county and reservation, lack of service Accessing services – give people an opportunity to contribute in services Paying a coordinator (Billings position paid) Heather Commerce of health Impact of physical buildings from social change Saddened that N.A feel so segregated and trapped Nutrition importance Examples illustrated willingness to think differently Quality of programs Training of staff- important reducing stress of participants and staff Business skills needed by healthcare providers Farmers market partnership with SNAP Good examples of grass roots Have to stop waiting for anyone else to fix out healthcare programs Have to keep asking ourselves, “What is it that I don’t know?” Stepping out of being so structured So many opportunities for connecting and impacting; so many interested in working together Charter school Mayor walking path United way- connectives match maker Not duplicate efforts Adult mentorship programs Health improvement = community development Self-surfacing matrix Discharge planning Service navigation Social determinants Selling vs. buying State and local awareness of need to connect to CD CD locating services Creating measurements that make sense for MT What are the factors of “readiness” to dive into collaborative work for a community Social impact bonds/pay for success model 2. What specific needs in your community could be addressed through collaboration between community development and health? Any ideas for specific projects or other actions that could meet those needs? Housing (12): Transit housing; Manufactured housing; Journey home; Wellness into where people live; Housing – chronic inebriation – mental illness; Supportive housing; Homelessness affect downtown business Transportation/Walkability (11): Sidewalks; Transportation planning – impact on neighborhoods/health; Alternate transportation models, organize hierarchy of routes; Multi model transit walkways; Public transportation continues to be a need; Poor bike systems, connectivity, sidewalks etc. Early childhood/Youth/Family (9): Issues investment; Focus on kids/families; After school programs; Child abuse; Team up mother and baby home visits with oral health info; Improving youth education; Co-locating housing of childcare services; Parenting place Food (8): Zoning food access; Food security; Food bank; Mobile grocery store (Food Share, United Way); Access to healthy food downtown- our food bank is not very accessible; Addressing senior citizen rural health nutritional needs Partnerships (7): Coordination between overarching goals – centralized services; Take information, share it; Specific needs - getting two worlds together; Awareness of another’s work; Missoula Homeless Shelter/Poverello Center - partners with partnership; Information share; Provide support for research Mental Health (5): Community care teams; NAMI; Mental health issues and social determinants to mental health issues – general practitioners deal with all issues Aging Population (2): Addressing basic needs Community Health Workers (2): More CHWs and CHCs Public Safety Initiative (2): Injury prevention (intentional and unintentional) Education (2): Education is the key; Culturally relevant Built environment (2): Need liaison – public health Other: How to organize for it Nature Best practices Community-based counselors Workforce development Act with sense of urgency and look beyond lifetime Know who players are, good models and success stories in MT Helena – building needs – schools/jails/nonprofits Developing trust at the top of the agenda Dental/Oral Health – funding for students in Children – reduce future cost in Medicaid, increase school attendance improved long term health Explore social enterprise or social impact bonds Mall repurpose – swimming pool, indoor soccer fields/basketball courts Use non-profits/service agencies Decreasing obesity, suicide rates, especially in rural communities Marketing – how to reach the target audience Develop the collective impact model Access Policy Low income people don’t advocate self- can’t talk to media- be yourself Make more workable- doesn’t encourage health- cant cross street sidewalks A good intake form Substance abuse inpatient for low income? Fatalities Current tobacco use by Native Americans- not being addressed very well People/ kids having a sense of worth/ hope that they will find a place in their community Compassion fatigue – mind and body wellness Build recreational center Providing legal aid at CHC’s Social isolation Collaborative community needs assessment 3. What are some steps that community development and health professionals in your community could take together now to build relationships and be more effective in their work? Data (12): Research; Data driven; Multi-dimensional collected cross sectors; Way to convene and share; Data analysis and data share; Data party; Data sharing –obstacles; Use evidence, be open to what evidence says; Look at your work (data) and work with people who apply data; Coffee meetings Awareness/Community Involvement (12): Learn more about existing programs/services; Make projects more well know across state; Share information in communities; Community discussion and support; Awareness of resources; Preventing duplication of work; Basic understanding of what others do; Learn what others do – get different perspectives; Understand resources in each world and how they work - bring people together; Make sure that new community development initiative have health in mind; Collaborative community issue determination; Ask the people most affected Partnerships (9): Continue conversation; Collaboration partners; CHNA – great place to start relationship building – Hospital and public health; Seek out the champions; Getting the right people to the table; Keep this conversation going – expand to nonprofit assoc. – community foundation involved in planning; Keeping local coalitions focused – bring more coalitions together; “Train the trainers” to change dialogue to be more inclusive; Better collaboration between community development and health sector in CHNA Funding (7): Resource and refund organizer – 211 directory; Financial resources and correct grant language; Change the perspective on financing projects of value to the community; Finding resources for a paid facilitator; Engage funders in conversation from the start; Funding for small projects for staff is critical Strategic Planning (4): Strategic planning – including funders, government business – pooling funding and resources (How to figure out who those are?) Accessible; Strategize – gap analysis; Plan set goals; Determine one goal – then move it Other: Social impact bond (pay for success) Prototype – small investment – pilot- paralyzation on planning Centralized services – one stop shop Health impact study – (like environmental impact study) What does a “healthy community” mean? Health impact assessments – special training like an environmental assessment Collective impact – Pay for Success Model – Root cause Community Assets Inventory – Community Capitals Look at super utilizers of healthcare Inclusive of stakeholders (IHS & tribal MSU Extension agents, 4-H State and Tribal Colleges Pow-wow events Workforce training, development, keeping them Address root causes – more than symptoms, prevention is key Structure systems/ integration mechanisms More events like today’s conference- structured to bring different sectors together Involve transportation orgs in conversation from start Medicaid expansion for housing in MT Project launch 0-8 year olds mental health consultants Are there companies willing to employ people who have struggled? Can we merge housing for mental health with local found resiliency/ micro enterprise farm, and food is sold to diabetes patients or served in hospital City health department convenes H.C. coalition- quad county Tracking chronic disease portion (health improvement plan) 1st step is creating a shared vision Be involved with our passions Built consortium of landlords Changing attitudes to doing more broader engagement Start small Success breeds success Create a special session at industry and association trade events