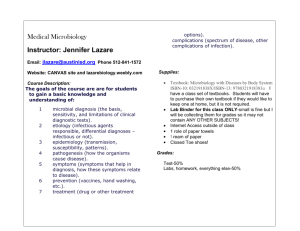
Microbiology
advertisement

Microbiology - Chapter 14 Non-Specific defenses to invasion and infection Lines of defense against infection or invasion – both non-specific and specific Microbiology - Chapter 14 Know for test Microbiology - Chapter 14 1st – body systems that normally keeps microbes out of tissue and prevent disease a. intact skin 1. outer epidermis of dead epithelium cells, dry and unfavorable environment 2. keratin protein resist invasion 3. normal flora of skin microbes only a threat if skin is damaged (opportunists) Microbiology - Chapter 14 b. mucous membranes and secretions 1. epithelium tissue lining the respiratory, GI tract, and genitourinary tract 2. have specialized goblet cells that secrete stick substance called mucous 3. respiratory tract have ciliated epithelial cells that move mucous up – mucous traps microbes and particles, cilia move the material up - ciliary escalator-very efficient at protecting delicate tissues that are more easily invaded Microbiology - Chapter 14 4. sweat glands on skin produce perspiration that wash the skin 5. lysozyme in the sweat breaks down cell wall of gram positives 6. sebum in the skin is acidic-oily substance, pH of 3 to 5, inhibits growth of some microbes 7. stomach secretions, very acidic, kills most pathogens, some toxins are resistant Microbiology - Chapter 14 c. normal microbial flora – microbial antagonism, ecosystem on cellular level, 1. normal balance, keeps pathogens in check 2. if upset in balance, then microbe imbalance can result in problems – yeast infections, or in broad spectrum antibiotics, organisms grow that usually wouldn’t grow – C.difficile, diarrhea Microbiology - Chapter 14 Clostridium difficile is a bacterium that can be found in the colon. It can cause low-grade Diarrhea or severe colitis. It most commonly occurs when an individual is placed on antibiotics. The antibiotics kill off the good bacteria in the colon, and allow room for Clostridium difficile bacterium to grow. In addition, it can be contagiously spread from one person to another, especially in hospital and nursing homes Microbiology - Chapter 14 2nd line of defense, system elements, non-specific, go into action if 1st line is breached a. PHAGOCYTES – VERY IMPORTANT, these cells engulf and destroy invaders and particulate matter 1. All of the phagocytes are types of white blood cells 2. circulating in the blood and found to some extent in tissue (modified forms), ready to respond to invasion 3. more later Microbiology - Chapter 14 b. Inflammation and fever – if tissue is damaged, inflammation reaction occurs and it is characterized by redness, pain, heat, swelling 1. non-specific response to tissue damage or invasion to limit and stop the infection or damage 2. many things cause an inflammation reaction – infection, injury, even chemical action 3. purpose of inflammation reaction a. to destroy and remove the disease agent if possible b. limit the effect of the invading agent c. repair the damage at the site of injury Microbiology - Chapter 14 4. Several specialty proteins are involved at the injury site that aid in the processes that limit the invader and help destroy the invader, even help clean up and repair the damage complement, kinins, interferon, fibrin Blood cell formation illustrated on next slide Microbiology - Chapter 14 3rd line of defense - this is specific, a production of specific counteracting chemicals, called antibodies that can recognize and act on invaders to destroy them a. usually proteins b. produced by specialized lymphocytes (B and T cells) c. Cover in detail in chapter 15 Microbiology - Chapter 14 Process of Phagocytosis – simplify into 4 stages 1. Chemotaxis – phagocytes are chemically attracted to a site where invaders are present a. chemotactic mediators – peptides from damaged tissues, microbial waste products, components from white blood cells b. these chemicals released at site of infection or injury attract the phagocytes (some in the tissue already, some circulating in the bloodstream) Microbiology - Chapter 14 2. Adherance – attachment of phagocyte to invader or particle, a. opsonization – some particles or agents are coated with serum proteins, thus allowing the phagocyte to more easily attach, some of the complement proteins act as opsonins b. some microbes produce capsules or proteins that resist phagocytic adherance, more virulent Microbiology - Chapter 14 3. Ingestion – pseudopods of phagocytes surround invader or particle, once completely surrounded, the particle is said to be enclosed in a phagosome 4. Digestion – a cellular organelle, a lysosome, fuses with the phagosome and the digestive enzymes of this new phagolysosome kill the microbe quickly (lipases, proteases, lysozyme, other digestive enzymes, plus strong oxidants and other radicles that can kill the microbe and break it down) a. the waste products are kept packaged b. the waste particles are expelled c. some microbes survive inside the phagocyte, get a free ride and phagocyte may actually help spread the agent to other tissues – Shigella and Listeria, HIV virus, tubercle bacilli Microbiology - Chapter 14 5. Expulsion: End products are expelled and filtered out and removed by other organ (liver) See next slide for diagram Process of phagocytosis Microbiology - Chapter 14 Acute Inflammation – Remember this is a non-specific reaction to the breach of the body primary defense barriers. The reaction is general and can be used to combat most all of the body invaders (bacteria, viruses, helminthes, protozoans) see slide to follow – we will follow that diagram 1. injury or invasion, at site chemical signals are released 2. blood vessels dilate, opening up of diameter of blood vessel, increase blood flow, causing redness (erythema) and heat 3. Vasodilation and increased permeability of blood vessels are caused by chemicals released by damaged tissues Microbiology - Chapter 14 i. histamine- found in mast cells of connective tissue, ad other tissue elements (a histamine reaction can be very serious – in hypersensitivity reactions – more later) ii. kinins – several varieties, also increase permeability and vasodilation iii. prostaglandins are also released by damaged cells – these chemicals allow more phagocytes to be attracted to the site and they in turn produce more chemicals that attract more phagocytes to the damaged area (mobilization of defenders) The movement into the damaged tissues of these cells is vital to stop the invaders at the local site. Microbiology - Chapter 14 iv. Leukotrienes – Chemicals produced by mast cells and basophils, they increase permeability of blood vessels (more phagocytes can leave blood to get into tissue that has the invader). They also help the phagocyte to attach to the invader cells. v. increased permeability allows blood elements that result in clot formation to exit into tissue to wall off area and prevent further invasion or tissue damage (fibrin net) vi. pus forms – collection of dead cells and tissue fluid vii. localization of the site and walling off to prevent the spread of infection often produces an abscess (like a boil, or pustule) (remember what a fire ant bite looks like) Microbiology - Chapter 14 4. This acute inflammation activity, producing swelling , redness, pain, heat etc. limits and stops the invasion. The cells that migrate to the site then destroy the invaders and even begin the process of clean up repair. Ultimately healing of the site occurs. a. Mast cells (fixed tissue macrophages, contain histamine, very important in inflammation and repair of damaged tissue) are real involved in clean up and repair. Microbiology - Chapter 14 b. Role of the group of chemicals called generally – Complement. Complement is a series of proteins found circulating in blood plasma. These chemicals are inactive until needed and then activated to perform their role in helping prevent further invasion by microbes. Injury or infection triggers their activation. They then help trigger the body’s inflammation reaction. Microbiology - Chapter 14 Complement 1. affect blood vessels – permeability and dilation 2. actually attract leukocytes (phagocytes), activate phagocytes 3. produce inflammatory mediators 4. actually can act on microbes and cause them to lyse (rupture) cytolysis 5. the activation of complement is complicated and proceeds in a step wise process called a cascade see pg 441, 6. The complement cascade happens quickly and then is quickly shut off to prevent host cell damage. 7. Opsonization – one complement cascade results in a fragment that attaches to invader cells and oposonizes them – making them easier for phagocytes to attach to and thus destroy them Microbiology - Chapter 14 INTERFERONS – non-specific antiviral proteins produced by host cells when host is infected by a virus 1. general – not specific 2. 3 types - alpha, beta, gamma 3. alpha and beta IF cause uninfected cells to produce antiviral proteins (inhibit some function of the virus – mRNA synthesis, or viral protein synthesis 4. gamma IF can cause neutrophils to kill bacteria 5. Recombinant DNA technology, production of interferon by bacteria in pure form and in large quantities to treat some diseases (herpes, hepatitis B and C) INTERFERONS – non-specific antiviral proteins produced by host cells when host is infected by a virus 1. general – not specific 2. 3 types - alpha, beta, gamma 3. alpha and beta IF cause uninfected cells to produce antiviral proteins (inhibit some function of the virus – mRNA synthesis, or viral protein synthesis 4. gamma IF can cause neutrophils to kill bacteria 5. Recombinant DNA technology, production of interferon by bacteria in pure form and in large quantities to treat some diseases (herpes, hepatitis B and C)