Biology 3201 Unit 2 * Reproduction & Development
advertisement

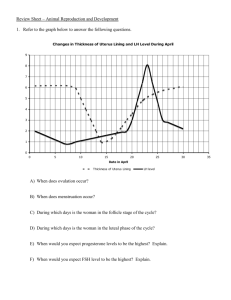
Biology 3201 Unit 2 – Reproduction & Development Chapter 15 Continuance of Human Life Ms. K. Morris 2010-2011 Section 15.1: The Human Reproductive System p. 486-499 The Human Male Reproductive System Male Sexual Structures • Sperm pass through the sperm duct (vas deferens) and connect to a short ejaculatory duct that connects to the urethra. • The urethra passes through the penis and opens to the outside. Secretions from the seminal vesicles add fructose and prostaglandins to sperm as they pass. • The prostate gland secretes a milky alkaline fluid. • The Cowpers (bulbourethral) gland secretes a mucus-like fluid that provides lubrication for intercourse. Sperm and secretions make up semen. • Testes are suspended outside the abdominal cavity by the scrotum, (for an optimal temperature for sperm development). • Seminiferous tubules are inside each testis, and are where sperm are produced by meiosis. Spermatocytes inside the tubules divide by meiosis to produce spermatids that in turn develop into mature sperm. • Sperm production begins at puberty and continues throughout life, with several hundred million sperm being produced each day. • Once sperm form they move into the epididymis, where they mature and are stored. • Four sperm are produced per meiosis. Sperm are small, motile and contain an enzyme filled acrosome that allows it to digest through the egg. • Testes- produces sperm and reproductive hormones. They hang outside the body cavity within the scrotum so that they have a cooler temperature for the formation of healthy sperm. Testes develop inside the body but descend during the last two months of fetal development. Sterility usually results if the testes fail to descend, but this can be corrected surgically. • Scrotum- sac that contains the testes outside the body. • Seminiferous Tubules- long coiled tubules which makes up the testes. It is here that spermatogenesis occurs. The lining of each of these tubules is composed of cells undergoing meiosis and sperm are continuously produced and released from the inner lining. • Epididymis- as sperm are formed they move to the epididymis where they mature and become motile. • Sperm Duct (vas deferens)- the tube that leads upward from the testes into the abdominal cavity where it joins the urethra. • Penis -male reproductive organ. • Cowpers Gland and Prostate Gland -produce an alkaline fluid which neutralizes acids in the female reproductive tract. • Seminal Vesicles- provide a mucus like fluid containing fructose which provides energy for the sperm. • Cowpers gland, prostate, and seminal vesicles secrete fluid into the urethra (also the tube where urine exits the bladder and combine with sperm to produce semen). Male Reproductive Hormones: (1) Follicle Stimulating Hormone (FSH)- stimulates spermatogenesis from the anterior pituitary. (2) Inhibin- released by the seminiferous tubules and forms a negative feedback loop with FSH. It acts on the hypothalamus to slow the production of releasing factors that control the release of FSH. Interaction of inhibin and FSH controls the rate of formation of sperm. (3) Luteinizing hormone (LH)- also from anterior pituitary, stimulates the interstitial cells of the testes that surround the seminiferous tubules to produce male sex hormones. (4) Testosterone - the major androgen (male sex hormone) and is responsible for the development of male secondary characteristics – – – – – enlargement of penis and testes enlargement of the larynx (Adams apple) inhibits fat and promotes development of muscle tissue stimulates formation of the face, chest, underarms and genitals levels of testosterone in the blood inhibits the production of LH Male Sex Hormones… • The anterior pituitary produces folliclestimulating hormone (FSH) and luteinizing hormone (LH). Action of LH is controlled by the gonadotropin-releasing hormone (GnRH). LH stimulates cells in the seminiferous tubules to secrete testosterone, which has a role in sperm production and developing male secondary sex characteristics. FSH acts on cells to help in sperm maturation. Negative feedback by testosterone controls the actions of GnRH. The Human Female Reproductive System • The ovary contains many follicles composed of a developing egg surrounded by an outer layer of follicle cells. Each egg begins oogenesis as a primary oocyte. • At birth each female carries a lifetime supply of developing oocytes, each of which is in Prophase I. • A developing egg (secondary oocyte) is released each month from puberty until menopause, a total of 400-500 eggs. • Ovary- production of female gametes (ova). • Follicles- tiny egg sac in ovary. They are composed of many groups of cells, each of which contains a single ovum. • Oviduct (Fallopian tube)- tube which carries the egg into the uterus or womb. The lining of each tube is ciliated to created a current that moves the egg toward the uterus. • Ova are released from different parts of the ovaries so the openings of the oviducts consist of finger like projections called fimbriae which sweep over the ovaries. They are also ciliated to sweep an ovum into an oviduct for its trip to the uterus. • Uterus- fist sized organ with thick muscular walls; receives a fertilized egg for further development (embryo implants inside the uterus). • Endometrium- lining of the uterus containing many blood vessels that can nourish the developing embryo. It is affected by the changing hormone levels during menstruation. • Cervix- forms the opening or exit to the uterus. • Vagina- what the cervix extends downward into the birth canal and leads to the outside of the female body. • Note: human female has two separate openings for urinary and reproductive function. Also the vagina has two functions: – (1) Allows entry of sperm into female body – (2) Exit of baby during birth Ovarian Cycles • After puberty the ovary cycles between a follicular phase (maturing follicles) and a luteal phase (presence of the corpus luteum). • These cyclic phases are interrupted only by pregnancy and continue until menopause, when reproductive capability ends. • The ovarian cycle lasts usually 28 days. During the first phase, the oocyte matures within a follicle. • At midpoint of the cycle, the oocyte is released from the ovary in a process known as ovulation. • Following ovulation the follicle forms a corpus luteum which synthesizes and prepares hormones to prepare the uterus for pregnancy. • The uterus has an inner layer, the endometrium, in which a fertilized egg implants. • At the lower end of the uterus the cervix connects the uterus to the vagina. Hormones and Female Cycles (FSH, LH – pituitary) (progesterone, estrogen – ovarian) • The ovarian cycle is hormonally regulated in two phases. The follicle secretes estrogen before ovulation; the corpus luteum secretes both estrogen and progesterone after ovulation. • The ovarian cycle covers events in the ovary; the menstrual cycle occurs in the uterus. The menstrual cycles’ first day of blood flow (day 0) known as menstruation. • During menstruation the uterine lining is broken down and shed as menstrual flow. FSH and LH are secreted on day 0, beginning both the menstrual cycle and the ovarian cycle. • Both FSH and LH stimulate the maturation of a single follicle in one of the ovaries and the secretion of estrogen. • Rising levels of estrogen in the blood trigger secretion of LH, which stimulates follicle maturation and ovulation (day 14, or mid-cycle). • LH stimulates the remaining follicle cells to form the corpus luteum, which produces both estrogen and progesterone. • Estrogen and progesterone stimulate the development of the endometrium and preparation of the uterine inner lining for implantation of a zygote. • If pregnancy does not occur, the drop in FSH and LH cause the corpus luteum to disintegrate. • The drop in hormones also causes the sloughing off of the inner lining of the uterus by a series of muscle contractions of the uterus. Female Hormone Treatments • With age there is a decrease in the number of functioning follicles and therefore a decrease of estrogen and progesterone in the blood. This signals the onset of menopause, characterized by the cessation (stopping) of menstruation. Menopause Characteristics: – cholesterol levels rise and bone mass declines – blood vessels alternately constrict and dilate causing “hot flashes” – mood changes Some doctors prescribe hormone replacement therapy in the form of low levels of estrogen and progesterone Benefits of hormone replacement: – relief of menopausal symptoms such as hot flashes, night sweats and sleep disruptions – prevention of bone loss (osteoporosis) – improved memory – decreased chance of urinary tract infection – decreased chance of macular degeneration (a leading cause of blindness) – the risks of hormone replacement vary with the hormone prescribed Potential side effects of estrogen replacement: – – – – – irregular vaginal bleeding stomach upset severe headaches formation of blood clots increased risk of breast and uterine cancer Potential side effects of progesterone replacement: – stomach upset – irregular vaginal bleeding – edema (water retention) Potential side effects of combined estrogen and progesterone replacement: – – – – – – formation of blood clots increased risk of heart attack during first year of treatment headaches fluctuation of blood sugar level edema pre-menstrual like syndrome • Contraception is another application of female hormones. Birth control pills contain a combination of progesterone and estrogen or progesterone alone. Many of the risks associated with birth control pills are similar to risks associated with hormone replacement therapy. • One form of birth control contains synthetic forms of estrogen and progesterone. This pill is taken everyday for the first 21 days of each menstrual cycle, the combination of estrogen and progesterone suppresses secretions of FSH and LH as a result: – (1) Ovulation is inhibited – (2) The hormones cause the endometrium to develop abnormally so that if ovulation does occur the egg is fertilized, implantation cannot occur. Sexually Transmitted Infections (STI’s) p.496-499 (diseases spread through sexual contact ) • Most common STI’s are caused by viruses or bacteria. In the past bacterial infections such as gonorrhea and syphilis were deadly. Today they can usually be cured using antibiotics. Viral infections such as AIDS and genital herpes cannot be cured but can be treated. 1. AIDS and HIV • AIDS: acquired immunodeficiency syndrome. Caused by the virus HIV and attacks helper T cells of the immune system. Low helper T cells in blood leaves person susceptible to a variety of diseases and usually leads to sickness and death. Transmission of HIV: – – – – – vaginal or rectal intercourse oral/genital contact sharing needles among intravenous drug users blood transfusions (today blood is screened) children of mothers who are infected with HIV may be infected before or during birth Three Stages of AIDS: • Stage A- lasts about one year. No symptoms but may infect others, and as long as the body produces enough helper T cells the person remains well. • Stage B- 6-8 years. Begins when body cannot replace T cells fast enough • Stage C: Nervous disorders such as pneumonia and skin cancers. With no treatments the person will die in 6-7 years. 2. Hepatitis A, B and C • A- contracted by drinking contaminated water (sewage) or oral and anal contact • B- spread the same way as HIV • C- transmitted by infected needles or syringes Symptoms: • fever, headache, loss of appetite, abdominal pain and yellowish skin (jaundice) • may progress to cause infection of the liver, leading to liver failure, liver cancer or death • some people recover completely while others become asymptomatic and infect others • vaccines are available for A and B • hepatitis viruses may cross the placenta to infect the unborn child 3. Genital Herpes • Caused by herpes simplex 1 (HSV1) or herpes simplex 2 (HSV2) • HSV 1- commonly causes cold sores and fever blisters on the mouth • HSV 2- likely acquired through sexual contact and may cause genital herpes Symptoms: • tingling or itching, followed by blisters which rupture • blisters may appear on genitals, buttocks or thighs or internal tissues and sores may take from three to five weeks to heal • flu like symptoms • blisters may reoccur with varying frequency or none at all • lymph nodes swell and a person experiences weight loss, night sweats, fatigue, fever and diarrhea • infections such as thrush (fungal infection) and herpes • no cure for genital herpes and once infected you are infected for life • herpes sores mean a risk of aids infection • if a newborn baby encounters a sore during birth the infection can cause blindness, neurological disorders or even death • mothers with genital herpes are encouraged to have caesarean sections 4. Chlamydia • caused by bacteria • men experience burning during urination and discharge from the penis • women may have vaginal discharge and symptoms or urinary tract infection including pain on urination and fever • one of the main dangers of Chlamydia is that 75% of cases are asymptomatic which means that many suffers do not have any symptoms until irreversible damage is done • if undetected women may develop sores on the cervix and oviducts, the patient may develop pelvic inflammatory disease (PID) which is painful and may lead to blocked oviducts. • if infection is caught early enough it can be treated and cured with antibiotics • if a baby comes in contact with Chlamydia during birth it can develop inflammation of the eyes or pneumonia 5. Syphilis - caused by bacteria Stage one: chancre sores appear at infection site Stage two : rash appears (usually on palms or soles of feet but may appear anywhere on skin) this stage is extremely infectious Stage three: infection affects cardiovascular and nervous system and may develop blindness, mental illness, and heart disease • large destructive ulcers may develop on skin or internal organs • can be treated with antibiotics it can be diagnosed with a blood test, symptom recognition or microscopic identification of bacteria • it must be treated early before the bacteria causes permanent damage • syphilitic bacteria may cause birth defects or stillborn 6. Gonorrhea • caused by bacteria • causes infection of the urethra, rectum, cervix and throat • pain on urination and thick greenish yellow discharge from the urethra • some people have no initial symptoms • women may develop PID and become infertile • infection may spread to heart valves, joints, or brain • many strains are resistant to traditional antibiotics • babies passing through the birth canal of infected mothers may develop eye infections leading to blindness. Therefore, eye drops are given to newborns as a means of prevention Section 15.2: Reproductive Control p. 500-505 Identify the causes of human infertility. (p. 501-502) In Females: (i) Blocked Oviducts – often caused by PID (pelvic inflammatory disease) which is often caused by STI’s. (ii) Failure to Ovulate – caused by hormonal imbalances that occur for a variety of reasons, including being underweight or overweight. (iii) Endometriosis – a painful condition in which the endometrium grows outside the uterus. (iv) Damaged Egg – which may be caused by environmental factors, such as exposure to chemicals. In Males: (v) Obstruction in the Vas Deferens or Epididymis – which may be caused by complications arising from STI’s or from varicose veins in the testicles. (vi) Low Sperm Count – caused by numerous factors, including overhead testicles, smoking, and alcohol intake. (vii) Abnormal Sperm – caused by factors including overheated testicles, exposure to toxins, and infections, such as STI’s. Technological solutions to human infertility: (p. 501, Table 15.1) (i) Artificial Insemination (AI) – Sperm is placed into the vagina by a physician. Used by: an infertile couple, men with low sperm count, women without male partners. (ii) In Vitro Fertilization (IVF) – Fertilization takes place outside the body, in a laboratory procedure. The fertilized oocytes are implanted in the uterus. Used by: a woman who has damaged or blocked oviducts. (iii) In Vitro Maturation (IVM) – Primary follicles are removed from the uterus and induced to mature into secondary oocytes. IVM is used to produce numerous oocytes for in vitro fertilization. Used by: a woman who will undergo in vitro fertilization. (iv) Surrogate Motherhood – A fertilized oocyte from an infertile couple (obtained by IVF) is placed in the uterus of a surrogate mother. Alternatively, a surrogate mother undergoes AI, using sperm from the male of the infertile couple. Used by: a woman who cannot bring a child to term, or a couple who is infertile due to unknown factors or factors that cannot be overcome by other technologies. (v) Superovulation (using fertility drugs) – Used to produce multiple eggs for in vitro fertilization, to increase the chance of pregnancy. FSH (follicle stimulating hormone) injections stimulate the development of multiple follicles. Cont’…. …HCG (human chorionic gonadotrophin) stimulates ovulation. Used by: a woman who is undergoing in vitro fertilization, or a woman who does not ovulate regularly, frequently, or at all, to increase her chances of pregnancy. (vi) Embryo Storage (Cryopreservation) – Oocytes, semen, and even embryos are preserved by freezing. Used by: a male or female cancer patient, who may become infertile or sterile due to radiation therapy, or a sperm bank that supplies semen for AI. Evaluate the design of birth control technologies and the way they function. Include: (p. 502) A) Barrier Methods: 1. Male Condom – about 85% effective. A latex sheath that fits over the erect penis. It traps the sperm. Risk is a reaction to latex. 2. Female Condom – about 85% effective. A polyurethane pouch that is inserted into the vagina. It prevents the sperm from contacting the vagina and cervix. No known risks. 3. Diaphragm – about 90% effective. A large latex cup that fits over the cervix and prevents sperm from entering. It is usually used with spermicidal jelly or foam. Sperm is blocked at the cervix. Risks are reaction to latex. 4. Cervical Cap – almost 85% effective. Must be used with the jelly. A latex cap is attached to the cervix by suction. Sperm is blocked, and killed by the spermicide, at the cervix. Risks are reaction to latex. 5. Spermicidal Jellies & Foams – about 75% effective. These products are inserted into the vagina before intercourse. They are often used with a condom or diaphragm. A large percent of sperm are killed. Risk is reaction to spermicide. 6. IUD (interutine device) – over 90% effective. An IUD is a plastic coil or armature that is inserted into the uterus. It lasts about 5 years. Implantation (of the egg) is prevented. Risk is PID (pelvic inflammatory disease). B) Hormonal Methods: 7. Birth Control Pill – close to 100% effective (if used correctly). A daily hormone medication taken orally. FSH and LH are not released. Risks include blood clots (especially in smokers), and hormonal side effects. 8. Morning After Pill – close to 100% effective (if taken properly). It can be taken up to 3 days after possible fertilization but the sooner it is taken the higher the success rate. Contains high doses of estrogen and progesterone. Prevents or delays the release of oocyte from ovary and if fertilization occurred it stops embryo from implanting in the endometrium. Side effects: nausea and vomiting. 9. Norplant (implant) – over 90% effective. Hormones are implanted under the skin. FSH and LH are not released. Risks are hormonal side effects. 10. Depo-Provera (needle) - 99% effective. A woman is given one hormone injection every three months. FSH and LH are not released. Risks are hormonal side effects. C) Surgical Methods: 11. Tubal Ligation – close to 100% effective. The oviducts are cut and tied. The eggs do not reach the oviduct or uterus. Risks are that it is permanent, irreversible, and sterility. 12. Vasectomy – close to 100% effective. The sperm ducts are cut and tied. There is no sperm in the ejaculate. Risks are that it is permanent, irreversible, and sterility. D) Other: 13. Rhythm Method – about 70% effective. The date of ovulation is determined by record keeping and temperature measurements. Intercourse is avoided at the most fertile times. No risks. 14. Abstinence - 100% effective. The woman must refrain from sexual intercourse. Sperm does not contact the vagina. No risks. • Assess the effects of birth control technology on the population demographics of developed and underdeveloped countries & debate the merits of funding solutions to human fertility problems versus human population control. (Read p. 503-505) – Investigate the methods of population/birth control of various countries around the globe and assess the effects of these conception control population technologies on the demographics of these countries. • China: 1 child per family rule • Selection of 1 gender (usually male) and abortion of females in some developing countries Recall: Demographic Transition… • Stage 2 is a period of rapid population growth and in stage 3 birth rates begin to decline. • Moving from stage 2 to stage 3 depends largely on contraceptive technologies. • More industrialized countries are in stage 3 of demographic transition, whereas many less industrialized countries (like some in Africa and Asia) remain in stage 2 (rapid population growth). • The reason for this is the availability of improved contraceptive technologies. • Drop is birth rate is possible with improved contraception, but yet some countries remain in stage 2. Why? – It is not enough for effective contraception to exist. – People must know that it exists and they must know how to use it. – It must be accessible to the people who want to use it (and this is not the case in less industrialized nations, especially poor people). – People must also want to have fewer children (cultural attitudes must change). – A power and education imbalance between women and men can affect contraception use as well. Section 15.3: Development & Differentiation p. 506-514 • Explain the processes of fertilization and development in human reproduction. Trace the journey of sperm and egg from their origin until fertilization and implantation. - Describe the following basic stages of embryonic development. (p. 508) – – – – – – (i) cleavage (ii) morula (iii) blastocyst (blastula) (iv) gastrula (v) germ layers (vi) neural development p. 509 • Development (fertilization, cleavage, blastulation, gastrulation, neurulation, organogenesis) • Fertilization - Contact between sperm and egg; entry of sperm into the egg and fusion of egg and sperm nuclei (upper third of the oviduct). • One sperm fuses with receptors on the surface of the secondary oocyte, triggering a series of chemical changes in the outer oocyte membrane that prevent any other sperm from entering the oocyte. • The entry of the sperm initiates Meiosis II in the oocyte. • Fusion of the egg and sperm nuclei forms the diploid zygote. • Cleavage converts a single-celled zygote into a multicelled embryo by mitosis. • The blastula is produced by mitosis of the zygote, and is a ball of cells surrounding a fluid-filled cavity (the blastocoel). • Gastrulation involves a series of cell migrations to positions where they will form the three primary cell layers: – Ectoderm forms the outer layer - skin, epithelium, brain and nervous system – Endoderm forms the inner layer - digestive and respiratory systems – Mesoderm forms the middle layer - body muscles, cartilage, bone, blood • Organ formation occurs in the next stage of the development of the embryo. • Induction is the process in which one cell or tissue type affects the developmental fate of another cell or tissue. Induction affects patterns of gene expression through physical contact or chemical signals. Formation of the vertebrate eye is a well known example. Travels of a Young Zygote • Cleavage of the zygote begins while it is still in the oviduct, producing a solid ball of cells (morula). The morula enters the uterus, continuing to divide and becomes a blastocyst. Identify chemical control hormones associated with implantation, birth and lactation. Include: – (i) progesterone – (ii) estrogen – (iii) oxytocin – (iv) prolactin – (v) human chorionic gonadotropin (HCG) – This outcome is addressed in the notes that follow… Implantation • The uterine lining becomes enlarged and prepared for implantation of the embryo in the trophoblast layer. • Twelve days after fertilization, the trophoblast has formed a two-layered chorion. • Human chorionic gonadotropin (hCG) is secreted by the chorion, and prolongs the life of the corpus luteum until the placenta begins to secrete estrogen and progesterone. • Home pregnancy tests work by detecting elevated hCG levels in the woman's urine. p. 509-510: The First Trimester (Weeks 1-12) • The three embryonic tissue layers form (ectoderm, mesoderm and endoderm). Cellular differentiation begins to form organs during the third week. During the second month most of the major organ systems form, limb buds develop. The embryo becomes a fetus by the seventh week. The Second Trimester (Weeks 13-24) • The fetus increases in size during this trimester, and bony parts of the skeleton begin to form. Fetal movements can be felt by the mother. The Third Trimester (Weeks 25-38) • During this trimester the fetus increases in size. Circulatory and respiratory systems mature in preparation for air breathing. Fetal growth during this time uses large parts of its mother's protein and calcium intake. Describe the process of childbirth. Include: • (i) dilation stage • (ii) expulsion stage • (iii) placental stage Birth (p. 512-513) • Birth is a positive feedback hormonal mechanism. During birth, the cervix dilates to allow passage of the fetus. Uterine contractions propel the fetus through the birth canal, usually head first. Hormonal control of the birth process involves the release of oxytocin and prostaglandins. 1) Dilation - dilation of the cervix. Membranes of the amniotic fluid rupture, lubricating the vagina. 2) Expulsion - Strong uterine contractions of a minute in duration separated by two to three minute intervals propel the fetus down the birth canal. 3) Placental –The placenta (or afterbirth) in expelled through the vagina. • Secretion of milk does not occur until delivery, and the action of prolactin. Suckling by the infant causes production of oxytocin to promote release of milk into the ducts emptying into the nipple. Explain how fraternal and identical offspring are produced: p. 507 Fraternal Twin • more than one egg is released from the ovary at the same time • two eggs become fertilized at the same time • two children will be born at the same time but they will be different since they developed from two different egg and sperm Identical Twin • zygote splits into two separate bodies during early development • these children will be the same and are genetically equal since they developed from the same zygote Describe the functions of primary membranes during the embryonic development of animals: Development of the fetus can be compared to a chick embryo: 1. Chorion is the layer located just inside the shell. It surrounds the embryo and other membranes. It controls the exchange of gases. 2. Allantois is a sac-like structure that grows out of the digestive tract of the embryo. It exchanges gases and collects the waste material of the embryo. 3. Amnion is a sac that surrounds the embryo. It is filled with fluid and keeps the embryo moist. It also cushions the embryo for protection. 4. Yolk sac holds the yolk. The yolk is food for the embryo. The embryo consumes all of the yolk before hatching. Describe the roles of the placenta and umbilical cord during pregnancy: • During three trimesters, the fetus needs to be nourished, get oxygen and get rid of waste. These functions are performed by the placenta and the umbilical cord. • Maternal and embryonic structures interlock to form the placenta, the nourishing boundary between the mother's and embryo's systems. • The umbilical cord extends from the placenta to the embryo, and transports food to and wastes from the embryo. • Placenta - a blood vessel-rich organ which is present only during pregnancy. • Begins to form from the chorion once fully implanted. • Chorion develops projections which extend into the uterine wall serving as an anchor. These projections contain blood vessels which, with the chorion, form the placenta. • Placenta is fully formed after the tenth week. • During and after development it produces estrogen and progesterone (prevents any new follicles from maturing and maintain uterine lining). • No ovulation or menstruation due to high levels of progesterone and estrogen in the blood. • The placenta is what the embryo of the fetus depends on for survival. It is where it gets all the nutrients and oxygen and all wastes are removed. • Umbilical Cord - it is a lifeline, connecting the developing embryo and fetus to the placenta. • The mother’s blood and the fetus’s blood never mix, but the transfer of nutrients and oxygen from the mother to the fetus, and the transfer of carbon dioxide and other waste substances from the fetus to the mother take place across plasma membranes. Examine the effects of teratogens on the development of the embryo: • Teratogen- any agent that causes a structural abnormality due to fetal exposure during pregnancy. 1. Cigarette Smoke - may constrict fetus’s blood vessels preventing the fetus from getting enough oxygen. • Mothers who smoke or who are exposed to a lot of second hand smoke may have babies that are under weight. • Also, the babies may suffer convulsions. 2. Alcohol - can affect the fetus’s brain, CNS, and physical development. • Babies that are born to women who drink frequently or heavily during pregnancy are likely to have fetal alcohol syndrome (FAS). FAS babies: • decreased height, weight and head size • head and face may be deformed • may show varying degrees of mental retardation • may show unusual aggression or have personality disorders 3. Prescription Drugs • For example, thalidomide. Prescribed to pregnant women in the 1950's to prevent morning sickness. • At that time it was thought to have no side effects. Doctors did not know it was teratogenic. • Thalidomide caused the babies to be born with deformed or missing limbs. • Pregnant women should always check to see if medication is safe for her developing baby. • Other teratogenic factors: – radiation (x-rays) – pollutants 4 techniques used to monitor various stages of embryonic or fetal development: 1. Ultrasound • Sound waves beyond the level of human hearing are sent through amniotic fluid. • Waves bounce off the developing fetus and are used to create a black and white, cross-sectional image of the fetus. • Image can be studied for physical abnormalities such as a missing limb, malformed heart, or cleft palate. 2. Amniocentesis • As a fetus moves inside amniotic sac some of its cells are sloughed off and become suspended in amniotic fluid. • A sample of this will give enough cells so that a karyotype which can be used to check chromosomes for number. • Cannot be done before the 14th week of pregnancy due to possible injury to the fetus. • A sample is taken with a long thin needle after the position of the baby is determined by ultrasound. • The sample of fluid is extracted, placed in a nutrient rich solution and allowed to multiply until there are enough fetal cells to get a good picture of all the chromosomes and create a karyotype. 3. Fetoscopy • Direct observation of the fetus occurs because of the insertion of an endoscope (long tube with a camera on one end) into a small incision in mother’s abdomen. • Enables procedures to take place inside womb such as removal of excess brain fluid and fetal blood transfusions. • Also provides a way to get blood samples to create a karyotype or to test genetic conditions such as Rh factor or sickle cell disease. 4. Chorionic Villi Sampling (CVS) • Amniocentesis cannot be done until 14th week and there is potential danger involved and it may take weeks to obtain results. Therefore: • Chorionic villi sampling may occur after the 9th week and cells can be removed from the chorion. • The chorion surrounds amniotic sac and is one of the tissues which makes up the placenta, which connects mother’s blood with fetal blood. • The chorion is made of fetal cells and also contains genetic information about the fetus. • Removed cells are grown in a special medium and a karyotype allows a diagnosis to be made.