File - Respiratory Therapy Files
advertisement
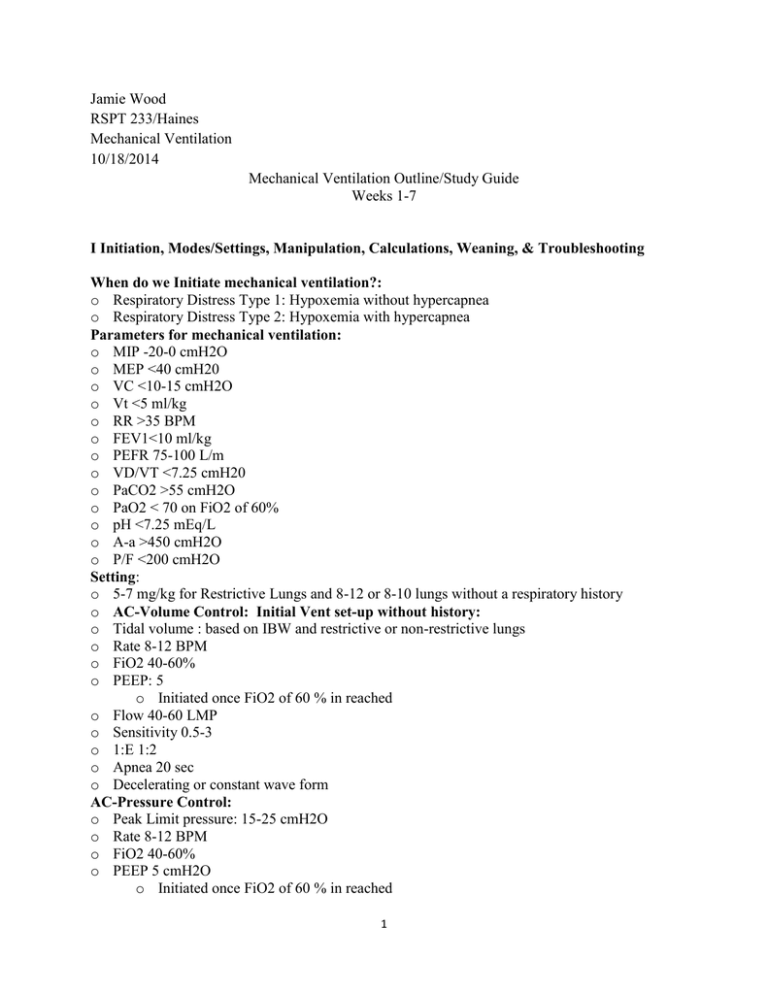
Jamie Wood RSPT 233/Haines Mechanical Ventilation 10/18/2014 Mechanical Ventilation Outline/Study Guide Weeks 1-7 I Initiation, Modes/Settings, Manipulation, Calculations, Weaning, & Troubleshooting When do we Initiate mechanical ventilation?: o Respiratory Distress Type 1: Hypoxemia without hypercapnea o Respiratory Distress Type 2: Hypoxemia with hypercapnea Parameters for mechanical ventilation: o MIP -20-0 cmH2O o MEP <40 cmH20 o VC <10-15 cmH2O o Vt <5 ml/kg o RR >35 BPM o FEV1<10 ml/kg o PEFR 75-100 L/m o VD/VT <7.25 cmH20 o PaCO2 >55 cmH2O o PaO2 < 70 on FiO2 of 60% o pH <7.25 mEq/L o A-a >450 cmH2O o P/F <200 cmH2O Setting: o 5-7 mg/kg for Restrictive Lungs and 8-12 or 8-10 lungs without a respiratory history o AC-Volume Control: Initial Vent set-up without history: o Tidal volume : based on IBW and restrictive or non-restrictive lungs o Rate 8-12 BPM o FiO2 40-60% o PEEP: 5 o Initiated once FiO2 of 60 % in reached o Flow 40-60 LMP o Sensitivity 0.5-3 o 1:E 1:2 o Apnea 20 sec o Decelerating or constant wave form AC-Pressure Control: o Peak Limit pressure: 15-25 cmH2O o Rate 8-12 BPM o FiO2 40-60% o PEEP 5 cmH2O o Initiated once FiO2 of 60 % in reached 1 o Rise-time 50% o I-Time: 0.8-1.2 o Sensitivity 0.5-3 o Apnea 20 sec o Decelerating waveform CPAP: o PS 10-12 cmH2O o Sensitivity 0.5-3 o Apnea 20 sec SIMV: o PS 10-12 cmH20 o Sensitivity 0.5-3 o Apnea 20 sec PRVC: o Targeted Vt based on IBW and restrictive or non-restrictive lungs o Pressure Limit 15-25 cmH2O o Rate 8-12 o FiO2 40-60% o Rise-time 50% o PEEP 5 o Sensitivity 0.5-3 Alarms: o High pressure/low pressure: 10/5 o High rate/low rate: 10:5 o High flow/low flow: 2L/2L o Vt: 200-100/100-150 Incremental Changes: o Vt: 50-100 o Rate: 2-6 o PEEP 1-2 cmH2O o Flow: 5-10 L o FiO2: 5-15% o Pressure: 2-5 cmH2O Manipulations: o Respiratory & Metabolic Acidosis: increase Vt first, then rate can be increased only if patient isn’t breathing over the backup rate. o Respiratory & Metabolic Alkalosis: Decrease rate first, then decrease Vt. o Hyperoxygenation: decrease FiO2 or PEEP o Hypoxygenation: increase FiO2 or PEEP Weaning: When is a patient ready for weaning? o Their underlying condition has been resolved o They are hemodynamically stable o Diagnostics: Labs, CXR and ABGs to determine issue is resolved o Check to see if the patient on sedation o Does the patient have the drive to breathe 2 o MIP: -20 cmH2O is the lowest acceptable o MEP: <50 cmH20 ? o VC: >10 cmH2O o RSBI: <105 or <100 being ideal/normal 50-100 Spontaneous Breathing Trials CPAP: o Pressure support 5-10 cmH2O o FiO2 o Flow ? o Sensitivity ATC (automatic tube compensation): o ATC delivers the exact amount of pressure required to overcome the resistance imposed by the ETT and reduces WOB o Provides variable pressure and variable inspiratory flow compensation o ATC increased pressure at the upper airway by the amount equal to the continuous calculated pressure drop across the ETT during inspiration SIMV: o Pressure Support o FiO2 o Flow o Sensitivity Trouble Shooting High rate/High Ve can be caused by o Pain, agitation, anxiety and fever : suggest possible sedation or other pain/fever medications o Low Vts: increase Vt or flow o Metabolic acidosis: change mode Low Rate o Over-sedation o Compensated metabolic alkalosis o Being over-ventilated with high Vte o Atrophy of the diaphragm o Neuromuscular impairment High PIP o Obstruction in the airway o Secretions o Bronchospasms o Patient is agitated o Kinked tubing, biting the tube o Agitation o Patient coughing Low PIP/Low Vte: o o o o Look for obvious leaks Does the patient have a chest tube Did the patient self extubate Check the integrity of the cuff 3 o Is the patient on spontaneous modes without PSV or support II Difference between static and dynamic compliance and do they relate to positive pressure ventilation: o Dynamic compliance is the movement of airflow through the upper airway. Dynamic compliance during positive pressure ventilation is related to resistance that airflow must overcome to move through the airway and obstruction that causes resistance to that airflow. o Static compliance is the measure of the volume of air not moving that the lungs can accept. Static compliance with positive pressure ventilation is measured to determine the volume of air that the lungs can accept and compliance of the lungs. Elastic and frictional resistance: o Elastic resistance is: The stiffening of the elastic system of the chest wall that produces an increase in PIP. PIP contributes to a decrease in compliance in the lungs. Decreased compliance in the lungs results in a decrease ability of the lungs to accept a desired volume to maintain adequate gas exchange and therefore oxygenation. o Frictional resistance: is simply airway resistance (Raw), which is opposition of the airways to flow and the tissues being displaced. The Opposition by the airways to flow results from excessive secretions, bronchospasms, and increase PIP, which inhibits the total gas filling that normally takes place in the alveoli, resulting in a decrease in gas exchange. III Effective Weaning Techniques: SBT: CPAP/SIMV, T-Piece and ATC CPAP/SIMV: o Progressively reduce the patients mandatory rate by 1-2 BPM at a pace that matches improvement of the patient at a RR of >8 BPM o Pressure support of 5-10 cmH20 for ,< 2-4 hours is provided to help unload the patients spontaneous breath and reduce the patients WOB against the vent, circuit and ETT. o If no lung disorders use 30 minute intervals instead o PEEP of 3-5 is maintained to compensate for changes in the FRC resulting from breathing through the ETT. o Apnea settings allow for additional support if needed T-Piece: o Is initiated if patient is able to spontaneously breathe o Patient is placed on a t-piece and off of vent support or places on CPAP, for increments if 510 minutes then place back on the vent for the duration of the hour. This is repeated once an hour. o Adjustments will continue until patient progressively reaches 30 minutes on and off of the vent. The 30 minute duration off the vent then is increased by an hour and progressively increased thereafter. o Humidification with a large reservoir, connected to air/O2 blended gas source that provides high flows of up to 10 L/min, at a desired FiO2 is connected to the t-piece. o On the exhalation port a large bore tube is connected to provide a reservoir. o If the patient remains stable for at least 2 hours, consider extubation 4 o Advantage of using CPAP is the available alarms, apnea back up, and ability to monitor the patients ventilation. o If patient is stable after 2 hours consider extubation PSV: Rate, timing and depth of breathing is determined by the patient: o Level of Pressure support is typically based on the patient’s Raw while on CMV and is set 10cm H2O above the patient’s Raw. o Normally PSV is set at 5-10 cmH2O for patient meeting weaning criteria o Also used to establish the patients baseline rate and Vt. o PSV is gradually reduced as long as spontaneous rate and Vt are maintained and no signs of distress occur Closed Loop Control Modes ATC (automatic tube compensation): o ATC delivers the exact amount of pressure required to overcome the resistance imposed by the ETT and reduces WOB o Provides variable pressure and variable inspiratory flow compensation o ATC increased pressure at the upper airway by the amount equal to the continuous calculated pressure drop across the ETT during inspiration Volume targeted Pressure Support (VS): o Patient triggered, pressure targeted, flow cycled o Has not been shown to be an effective weaning method o VS adjust pressure so that within a few breaths the Vt is met. Mandatory Minute Ventilation (MMV): o Monitors the set parameters and adjust accordingly o Automatically adjusts support per the needs of the patient o Maintains a consistent minute ventilation, by increasing support if the patients spontaneous ventilation decreases o MMV provides this support by adjusting the rate or Vt o Problems associated with MMV: this mode can increase dead space in patient breathing rapid and shallow Adaptive Support Ventilation (ASV): o ASV provides pressure limited breaths that target a pressure and rate o ASV monitors pressure, flow, I-Time and E-Time, compliance, resistance and time constants to ensure a constituent set Ve. o Reduces WOB and auto-PEEP Artificial Intelligence Systems (SmartCare/PS system: o Monitors set volume, rate and ET-CO2 to adjust to the inspiratory pressure automatically to maintain the patients zone of comfort Clinical observations during weaning during the first 20 minutes: o The patient’s HR may increase o The patient may appear agitated o RR may also increase 5 o Diaphoresis may result IV APRV and its effectiveness in reducing mortality in ARDS patients o APRV provides two levels of CPAP(PEEP) o Used for patients that a hard to oxygenate (ARDS patients) o Provides a distending pressure called high pressure during inhalation for 80-95% of the total cycle time and a low distending pressure during exhalation for the remaining time. o Protects against shear stress that is associated with ARDS (opening and closing of the alveoli) to reduce progression of ARDS Settings: o o o o High-Pressure: 20-25 cmH2O High-Time: 3-6 seconds Low Pressure 0-5 cmH20 Low-Time 0.5-1 sec How to increase PaO2 o o o o Increase High-P Increase High-T Decrease Low-P To increase the Pressure gradient and allow for more volume delivery How to decrease PaCO2 o o o o Decrease High-P Increase Low-T Increase Low-P To decrease the pressure gradient to provide more diffusion When to reduce support and how?: o Once at a pressure of <20 cmH2O the high pressure can be reduced by increments of 2 cmH2O o increase High-time by 0.5 increments o Increase Low-P in increments of 2 cmH2O o Once High-p and Low-P reach 15/15 then the mode is like CPAP on one continues pressure. V High Frequency Ventilation (HFV): o Used for patients with oxygenation issues o Utilizes various gas distribution mechanisms o Convection, Bulk Flow, Direct ventilation: Warming, filtering and humidification, direct ventilation of the alveoli proximal to the tracheobronchial tree by bulk flow of gas o The Pendalluft effect: Asynchronous filling of slow and fast alveoli units o Taylor dispersion: turbulence of gases in motion o Asymmetry: gas moving in the opposite direction simultaneously 6 o Cardiogenic mixing: the heart producing additional pressure that provides movement and distribution of gases in the parenchymal o Molecular diffusion: The distending pressure provided to the alveoli allows for increase pressure gradients between the membrane, providing increased gas exchange o Collateral ventilation: diffusion of gases throughout the collateral pathways of the lugs (pores of Khan, the Canals of Lambert and Martin Types of HFV o o o o High frequency oscillatory ventilation High frequency jet ventilation High frequency percussive ventilation High Frequency Flow Interruption VI New Modes of Ventilation: sophistication and complexity (are they beneficial or do their complexity decrease proper application: PRVC: Pressure Regulated Volume Controlled: Provides a breath by breath analysis Also called: APV, VTPC VC+: Used in AC and SIMV o o o o o o o o Patient triggered, pressure targeted, flow cycled Good for trending static compliance changes (patients entering into ARDS) Pressure limit is set in the alarms at 35-40 cmH2O The pressure will adjust per to achieve the targeted volume If volume is met pressure remains the same If volume is higher than targeted, pressure will decrease by 1-3 cmH2O If volume is lower than targeted, pressure will increase by 1-3 cmH2O Once the pressure comes within 5 cmH2O of the set pressure limit, the vent will dump the volume o The first breath is a test breath: o 5-10 above PEEP Inspiratory hold to measure the static compliance The next 3 breaths pressure will increase to 75% o Complications with this mode: not used for patients with irregular breathing patterns, because they will not be able to achieve consistent volumes APRV: Adapted Pressure Release Ventilation: 2 levels of CPAP (PEEP) o Used for patients that a hard to oxygenate (ARDS patients) o Provides a distending pressure called high pressure during inhalation for 80-95% of the total cycle time and a low distending pressure during exhalation for the remaining time. o Protects against shear stress that is associated with ARDS (opening and closing of the alveoli) to reduce progression of ARDS Settings: o High-Pressure: 20-25 cmH2O o High-Time: 3-6 seconds 7 o Low Pressure 0-5 cmH20 o Low-Time 0.5-1 sec How to increase PaO2 o o o o Increase High-P Increase High-T Decrease Low-P To increase the Pressure gradient and allow for more volume delivery How to decrease PaCO2 o o o o Decrease High-P Increase Low-T Increase Low-P To decrease the pressure gradient to provide more diffusion When to reduce support and how?: o Once at a pressure of <20 cmH2O the high pressure can be reduced by increments of 2 cmH2O o increase High-time by 0.5 increments o Increase Low-P in increments of 2 cmH2O o Once High-p and Low-P reach 15/15 then the mode is like CPAP on one continues pressure. Adaptive Support Ventilation (ASV): o ASV provides pressure limited breaths that target a pressure and rate o ASV monitors pressure, flow, I-Time and E-Time, compliance, resistance and time constants to ensure a constituent set Ve. o Reduces WOB and auto-PEEP HFOV: High frequency Oscillatory Ventilation o Used for Adult and neonate with oxygenation issues (ARDS and patients predisposed to Shear Stress) o Provides active inhalations and exhalations Settings: o PEEP/MAP pressure is used as a baseline pressure: MAP normally 15-18 cmH2O o Amplitude is generated around the PEEP and is maintains the inspiratory/expiratory volumes generated by each frequency wave o Frequency (Hz) = The Rate 1 Hz =60 Breaths/sec. o 15 Hz= 900 BPS typically used for neonates o 10 Hz= 600 BPS typically used for termed infants o 8 Hz=480 BPS typically for children 6-10 kg o 6 Hz= 360 BPS typically for children above 10 kg o <5 Hz=300 BPS typically for adult patients o IT% set normally at 33% o I:E normally 1:2 8 o Good chest and abdominal wiggle should be seen to be sure HFOV is working MMV: Mandatory Minute Ventilation o Monitors the set parameters and adjust accordingly o Automatically adjusts support per the needs of the patient o Maintains a consistent minute ventilation, by increasing support if the patients spontaneous ventilation decreases o MMV provides this support by adjusting the rate or Vt o Problems associated with MMV: this mode can increase dead space in patient breathing rapid and shallow APV: Adaptive Pressure Ventilation o o o o o o o o o Used in AC and SIMV Patient triggered, pressure targeted, flow cycled Good for trending static compliance changes (patients entering into ARDS) Pressure limit is set in the alarms at 35-40 cmH2O The pressure will adjust per to achieve the targeted volume If volume is met pressure remains the same If volume is higher than targeted, pressure will decrease by 1-3 cmH2O If volume is lower than targeted, pressure will increase by 1-3 cmH2O Once the pressure comes within 5 cmH2O of the set pressure limit, the vent will dump the volume o The first breath is a test breath: o 5-10 above PEEP Inspiratory hold to measure the static compliance The next 3 breaths pressure will increase to 75% o Complications with this mode: not used for patients with irregular breathing patterns, because they will not be able to achieve consistent volumes ATC (automatic tube compensation): o ATC delivers the exact amount of pressure required to overcome the resistance imposed by the ETT and reduces WOB o Provides variable pressure and variable inspiratory flow compensation o ATC increased pressure at the upper airway by the amount equal to the continuous calculated pressure drop across the ETT during inspiration VS: Volume targeted Pressure Support o Patient triggered, pressure targeted, flow cycled o Has not been shown to be an effective weaning method o VS provides pressure to allow the desired Vt to be reached in a few breaths PAV: Proportional Assist Ventilation o o o o Ideal for patient unable to maintain spontaneous ventilation Provides, pressure, flow and volume assistants in relation to the patients effort The greater the patient effort the more assistance provided Capable of providing 5-95% of the support 9 o o o o Used on ETT and Tracheostomy airway types Expiratory sensitivity flow will cycle the next breath The patient controls the TI, PIP, TE, and VT Disadvantages: Auto-PEEP may develop with increased triggering effort, also a leak will cause the machine to auto cycle. VAPS: Volume Assured Pressure Support: o o o o o o o o Helps to reduce the work of breathing, and maintain a minimum Vt and Ve Settings: P-Limit, RR, Peak flow, PEEP, FiO2, Min. Ve. If pressure is too high, then all breaths will be pressure limited If Ve is not delivered, then the peak flow will maintain the volume until the volume limit is reached Once the Vt or more is delivered then the breath will end The Vt set is the minimum that the patient will receive The set pressure is the minimum of what the patient will receive VAPS adds flow until the minimum Vt is met and is used if patient is unable to meet the minimum Vt. VII Critical Care Monitoring, ETCO2, Hemodynamic monitoring and Capnography: Danny’s Lecture ETCO2: o Provides quantitative information on effectiveness of CPR compressions o ETCO2 should increase with sufficient CRP Critical Care Monitoring: No color change: o o o o o o o o o o Look at HR, Sat., skin color Auscultate stomach CXR for expansion Inadequate perfusion rhythm: assess ETCO2 for defects Cardiopulmonary arrest: Lethal arrhythmias will stop perfusion Maintaining Alkalodic pH to prevent vasoconstriction with patients that have increased ICP (neuro. Pts) Statusasthmaticus: increase peak pressure VIDD: Ventilator Induced Diaphragm Deficiency o Keep pt. triggering above the set rate at all times to avoid VIDD Triggering represents 30-40% of the WOB Hemodynamic compromised patient (we don’t want to trigger the vent) Establishing Peep Levels: o Optimal PEEP: is the PEEP that is a given that has the least amount of hemodynamic effects on the patient. o Is determined by trending the adjustments made 10 Waveform Capnography: o Assessment of: Perfusion and CO Time constants (Kt): o Is the rate at which alveoli fill and empty o Emphysema Pts have a high Kt and require a longer expiratory time to empty o Exhalation levels o Zone I: is the start of expiration and is the content of CO2 relative to flow o Zone II: is mid-expiration and is mixed alveolar gas with CO2 o Zone 3: is the end of expiration and contains rich CO2 If Auto-PEEP occurs in the rich CO2 Zone III: o Hypercapnia o Decrease ability to trigger o WOB is increased Auto-PEEP prevention and management: o o o o o Check the HME Suction Decrease TI to increase TE Sedation is recommended for acute scenarios Increase set PEEP to match the auto-PEEP (don’t exceed 75-80%) Evaluating Asynchrony: o Pt/Vent. Relationship o Pt triggering can be achieved if less amount of pressure is needed to trigger o Flow trigger: flow 2 L/min is sensed via the circuit. The vent then senses the flow and initiated a breath to the patient o Pressure time product: the higher the PTP the harder it is for the patient to trigger the vent o Seen as air-starvation PSV: o PS is cycled off on the basis of flow o Defaults on most vents at 25% of the total flow o E-sensitivity VPS: noisy pressure support o PS set at 10 +/- 2 o Ideal for ARDS Pts NAVA: o Picks up diaphragmatic movement signal from the brain to the diaphragm and provides support determined by the 11 NM3 (NICO monitor): o o o o o o Analyzes the Ve and PaCO2 to determine dead space ventilation < 40% min. dead space calculation <10 norm, minute Ve > 40 Absence or pulmonary disease/airflow limited A large waveform gradient on the Capnography wave indicated large PaCO2 to ETCO2 Mechanical VD o Normal=15-25% o On CMV=40-50% Volumetric CO2: o Limitations to ETCO2: only measures at that point in time o VCO2 measures shows vol. of CO2 removal o Occurs in three phases: o ETCO2 32 o VT 600 o VCO2 50 ml/min o ETCO2 and VCO2 have an inverse relationship with each other o VCO2 gives faster results in regards to how the patient’s ventilation is: VD/VT: o Can be used as a predictor of mortality o >5% = increase in mortality by 45% o Decrease the VD/VT by Increasing PEEP Sutter’s PM Study: o Predicts the success of extubation o Corrugated tubing connected to the patient port, connected to the device that measures: o VC o Flow o Ve o Pulse ox also attached o Works like the Swan o Set base line, adds VD to increase return and increase CO o Not indicated for COPD pts. VIII Hemodynamics continued: Mike’s Lecture Physiology of BP: o High BP strains the heart 3 factors control BP o Heart o Blood 12 o Vessels Factors causing cardiomyopathy: o o o o Pericardium: covering Pericardium: visceral layer Myocardium: the musculature Endocardium: what lines the chambers The cardiac cycle: o Preload: ventricular stretch imposed by volume o HR o CVP o Ventricular compliance o Aortic pressure o Atrial contraction o Thoracic venous pressure (PEEP) o Afterload: the resistance to ejection of blood during systole What affects BP?: o Electrolyte imbalances o Cardiac Tamponade o Endocardium: caused by oral hygiene, drug abuse, diabetics using dirty needles. Causes the valves to rot, leads to regurgitation and decreases the ejection fraction o Normal EF= 60-70% o <20% is bad Hemodynamic calculations: o o o o o o o Normal CO= 5L or 4-6L (60ml/beat) BP=CO x SVR CO=SV x HR SV is dependent on the preload and inotrophy of the heart DO2= Hb x 1.34 x CO x SaO2/100 MAP= SBP- 2 x DBP/3 Ohm’s law of hemodynamics: MAP-CVP=CO x SVR or MAP≈CO x SVR Oxygen delivery Diagram: DO2 Hgb SpO2 CO BP 13 SVR Stroke volume Preload Inotropy Heart Rate Afterload Everything below the DO2 effects the DO2 o Preload: (the volume of blood present in the ventricles), Inotropy (the force of contractility by the heart related to the stretch of the myocardial cells) and afterload: the volume of blood remaining in the ventricles after ejection), affect the stroke volume (the volume of blood ejected from the heart with each beat) and the rate of contractility. o SV and HR affect the CO: (the volume of blood pumped/min.) o CO affects the Systemic vascular resistance and blood pressure o Hgb, SpO2 and CO affect he delivery of oxygen Hemodynamic disaster and treatments: o Hypovolemic shock: loss of blood volume. Treat with IV fluids and positive inotropic medications (epi). o If it is hypovolemic shock then addition then this treatment should work o A clinical assessment of hypovolemic shock is to lift the patients legs to assess if the SV increases. o If so underloaded volume exists then SV will go up o If not then the patient is overloaded and SV will decrease o Cardiogenic shock: Damage to the heart: treat with positive Inotropic medication or a pace maker to regulate the rhythm o Septic Shock (anaphylactic shock): Infection in the blood: give antibiotics to treat the underlying condition o Neurological Shock: Brain injury Blood pressure and ventricular filling curve: Heart failure o o o o Normal: 40 Mild heart failure: 45 Sever heart failure: <20 Ideally when increasing volume, we need to also increase the Force of contractility to ensure the heart can unload the volume given. If not the volume will remain in the ventricles causing increase work on the heart and a backup of blood in the heart o Finding the optimal volume, includes finding the variations of inotrophy that work o BP= SRV x HR X SV: SV x HR x CO o Fluid loading o Inotrophy or Preload (volume) must be given to increase BP (PEEP can also help reduce preload to improve inotrophy o Insufficient Inotrophy can cause overload and increase the afterload o Afterload is also dependent on Vasodilation or Vasoconstriction 14 o When if a patient in range of mild to severe failure, increasing inotrophy can their position on the curve instead of fluids. Types of Catheters: Arterial catheter: o Used to measure systemic Artery pressure, To collect an ABG inline, o Insertion site: radial, brachial, femoral, pedal (umbilical cord for Neonates) o Wave forms: up: is the increase of BP during systole, the dicrotic notch: is the closure of the aortic valves, and the bottom is arterial end-diastolic pressure. o Normal pressure= 120/80 mmHg: Systolic contraction = 100-140 mmHg: Diastolic 60-90 mmHg o Increase Arterial pressure: for better circulatory volume and function, Sympathetic stimulation, vasoconstriction and administration of vasopressors o Decrease arterial pressure in the presence of: Hypovolemia (shock/vasodilation) and Cardiac failure. o Arterial Catheter/Pulse pressure: is the difference between atrial systolic and atrial diastolic pressure o Bradycardia: causes a lower diastolic pressure caused by low rates, that allows blood volume more time for diastolic run off o Tachycardia: causes a higher diastolic pressure caused by high rates, that allows blood volume less time for diastolic run off o Causes of decreased pulse pressure: o Increased SV(Hypovolemia) o Decreased blood vessel compliance (atherosclerosis) o Bradycardia Central Venous catheter: o For assessment of right ventricular function and intravascular volume, for administration of medications, nutrients or blood and an emergency route for temporary pacemaker insertion o Decreases in CVP: absolute Hypovolemia (blood loss) and Relative Hypovolemia (Shock/vasodilation) o Increased CVP: increased venous return (volume overload) and increased thoracic pressure (PPV/Pneumothorax) o Complications: Infection o Bleeding o Pneumothorax Pulmonary Artery catheter (Swan Ganz): o o o o o For assessment of cardiopulmonary issues Typically 110cm Length Is a flow directed balloon catheter Measures pulmonary artery pressure Aspirate mixed venous samples 15 o Inject medication o Continuous monitoring of SvO2 o Balloon: 1.5 cc is the maximum inflation vol. Indications: o Hemodynamically unstable Pts, complex acute heart disease and acute severe pulmonary disease Measures: o o o o o o o CVP PAP PCWP Mixed venous blood Venous Saturation CO Provides cardiac pacing Insertion site: o at the subclavian internal or jugular vein, superior vena cava or right atrial o Normal Pressure: 0-6 mmHg Pressures in the heart: o Right ventricle: 20-30/0-5 mmHg o Occurs when the tricuspids open and blood flow into the ventricles causing the pressure wave to increase Pulmonary artery: 20-30/6-15 mmHg o Where mixed venous blood samples are drawn o Where the balloon on the catheter wedges a the small branch of the pulmonary artery o The forward flow of the artery is occluded and pressure measured: normal 4-12 mmHg Normal PA-wave form should return after the balloon is deflated Pulmonary Wedge pressure: at the branch of the pulmonary artery o Normal 4-12 mmHg (8 mmHg) o PAP: can increase as a result of many issues in the lungs: hypoxia, pulmonary vasoconstriction can cause blood to shunt o Assesses left heart issues: (Pressure, Preload, end-diastolic pressure, ventricular filling pressure) Changes in the PAWP is: o Decreased: Right heart failure, Cor Pulmonale, pulm-embolism, pulm-hypertension, air embolism, Hypovolemia 16 o Increased: Left heart failure, mitral stenosis, CHF/pulm-edema, High PEEP, Hypervolemia PA-catheter complications: o Infection, bleeding, pneumothorax, pulm-artery hemorrhaging, pulmonary infarction, air embolism, cardiac arrhythmias What increased the PAP: o o o o pulm-blood flow is decreased increased pulm-vascular resistance pulmonary embolus compression caused by disease that restrict the pulmonary vasculature What decreased the PAP o decreased volume of blood ejected by the right ventricle o Dilation of pulm-vasculature Clinical assessment: o Lung disorders: o CVP Increased o PAP Increased o PCWP normal/decreased o CO normal/with large PE o Right Heart Failure: o CVP Increased o PAP normal/decreased o PCWP normal/decreased o CO normal/decreased o Left Heart Failure o CVP normal/increased in late stage o PAP increased o PCWP increased o CO decreased o Hypovolemia: everything is decreased o CVP o PAP o PCWP o CO Other value to know: o o o o o Pulse Pressure: 40 mmHg SV: 60-130 ml/beat EF: 65-75% SVR: <20 mmHg/L/min PVR: <2.5 mmHg/L/min 17 Pressure Dampening: o The waveform doesn’t show a sharp wave form (no dicrotic notch) o The catheter may be obstructed or kinked ICU monitoring and equipment: o o o o o o Chest tubes: fluid and air evacuation Foley Catheter: urine drainage Eye Tape: to maintain moisture in pts. eyes GI Tube: to induce liquids, food or meds. ICP monitor: determines pressures in the brain Shunt: surgically placed tube in the ventricle that drains fluids into either (abdominal cavity, heart or large veins of the neck 18