v_REPRODUCTIVE SYSTEM_McC
advertisement

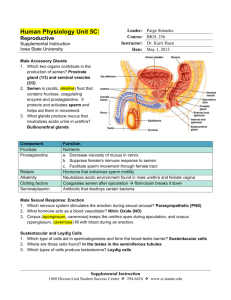
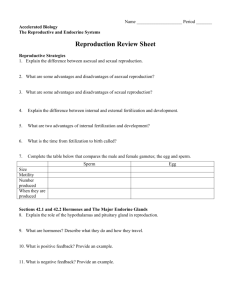
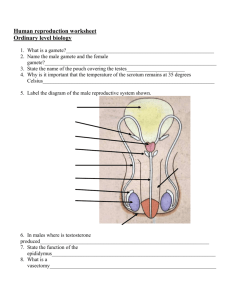
# Learning Outcomes Text Pages P1 P. 416-417 Identify and give functions for each of the following: testes (seminiferous tubules and interstitial cells), epididymis, ductus (vas) deferens, prostate gland, cowper's gland, seminal vesicles, penis. P2 Demonstrate a knowledge of the path of sperm from the seminiferous tubules to the urethral opening. P. 414-415 P3 List the functions of seminal fluid. P. 414-415 P4 Identify the tail, midpiece, head, and acrosome of a mature sperm and state their functions. P. 416-417 P5 Describe the functions of testosterone. P. 417 P6 Demonstrate a knowledge of the control of testosterone levels the endocrine system. P. 417 _____ Birth canal _____ Buffer _____ Bulbourethral gland _____ Cervix _____ Clitoris _____ Copulation _____ Corpus luteum _____ Cowper’s glands _____ Ductus (vas) deferens _____ Ejaculation _____ Endometrium _____ Epididymus _____ Erectile tissue _____ Estrogen _____ External genitalia _____ Fimbria _____ Follicles _____ Follicular phase _____ FSH ____ GnRH ____ Gonads _____ HCG _____ Implantation _____ Interstitial cells _____ Labia _____ Leutenizing hormone _____ Luteal phase _____ Menopause _____ Menstrual phase _____ Menstruation (menses) _____ Oogenesis _____ Ova _____ Ovaries _____ Oviduct _____ Ovarian cycle _____ Ovulation _____ Oxytocin _____ Pap smear _____ Penis _____ Placenta _____ Pregnancy _____ Progesterone _____ Proliferative phase _____ Prostate gland _____ Puberty _____ Scrotum _____ Secretory phase _____ Semen _____ Seminal fluid _____ Seminal vesicles _____ Seminiferous tubules _____ Spermatogenesis _____ Spermatogonia _____ Spermatozoa (sperm) _____ Testes _____ Testosterone _____ Urethra _____ Uterine cycle _____ Uterus _____ Vagina _____ Vulva _____ Womb Fertility facts. The largest cell in the human body is the female egg and the smallest is the male sperm. While you can’t see skin cells or muscle cells, the ovum is typically large enough to be seen with the naked eye with a diameter of about a millimeter. The sperm cell, on the other hand, is tiny, consisting of little more than nucleus. Dreams of pregnant women. The three things pregnant women dream most of during their first trimester are frogs, worms and potted plants. Many women also dream of water, and giving birth. Teething in the womb. Your teeth start growing 6 months before you are born. While some babies are born with teeth in place, the tooth buds that will eventually become teeth in young children (during their 1st year of life) are formed at 9 to 12 weeks in utero. All the blue-eyed babies. Babies are always born with blue eyes. The color of your eyes depends on the genes you get from your parents, but at birth most babies appear to have blue eyes. The reason behind this is the pigment melanin. The melanin in a newborn’s eyes often needs time after birth to be fully deposited or to be darkened by exposure to ultraviolet light, later revealing the baby’s true eye color. All the strong babies. Babies are, pound for pound, stronger than an ox. While a baby certainly couldn’t pull a covered wagon at its present size, if the child were the size of an oxen it just might very well be able to. Babies have especially strong and powerful legs for such tiny creatures, so watch out for those kicks. Infants with teeth. One out of every 2,000 newborn infants has a tooth when they are born. Nursing mothers may cringe at this fact. Sometimes the tooth is a regular baby tooth that has already erupted and sometimes it is an extra tooth that will fall out before the other set of choppers comes in. A fetus with fingerprints. A fetus acquires fingerprints at the age of three months. At only 6-13 weeks of development, the whorls of what will be fingerprints have already developed. Oddly enough, those fingerprints will not change throughout the person’s life and will be one of the last things to disappear after death. Single-celled people. Every human spent about half an hour as a single cell. All life has to begin somewhere, and even the largest humans spent a short part of their lives as a single celled organism when sperm and egg cells first combine. Shortly afterward, the cells begin rapidly dividing and begin forming the components of a tiny embryo. The goal of the reproductive system is to pass on your genetic code onto a new and unique generation. This is ultimately accomplished via fertilization. Terms you should know: 1. 2. 3. 4. 5. Haploid Diploid Zygote Gamete Gonad Label these on the diagram Human reproduction employs internal fertilization, and depends on the integrated action of hormones, the nervous system, and the reproductive system. Male gonads are the testes, which produce sperm and testosterone. estrogen Female gonads are the ovaries which produce eggs and 2 hormones: estrogen and progesterone. http://www.youtube.com/watch?v=WEzcK-OKd10 Male Anatomy The male external genitalia are the scrotum and penis. The scrotum is a fold of skin that encloses the male gonads (testes) The testes are a pair of tightly coiled tubes surrounded by several layers of connective tissues. These tubes are the SEMINIFEROUS TUBULES, where sperm are produced by meiosis. About 250 meters of tubules are packed into each testis. The INTERSTITIAL CELLS are scattered between the seminiferous tubules in the testes. These cells produce testosterone. Sperm production cannot occur at normal body temperature. So just before birth, the testes descend to hang outside the abdominal cavity in the scrotum, a fold of skin. The temperature in the scrotum is ~2oC below body temperature. SPERMATOGENESIS This, the production of mature sperm cells, is a continuous and prolific process in the adult male. Spermatogenesis occurs in the seminiferous tubules of the testes. The spermatogonia undergo repeated mitoses to produce large numbers of potential sperm or spermatocytes (approximately 3 million/day). SPERMATOGENESIS Next, Meiosis occurs to create 4 haploid spermatids. The sertoli cells transfer nutrients to the spermatids, and the developing sperm are gradually pushed toward the center of the seminiferous tubule and make their way to the epidymis. When the spermatids reach the epidymis, they acquire motility (mature), and are stored. SPERMATOGENESIS The process from spermatogonia to motile sperm, takes 65-75 days in the human male. Each ejaculation of a human male contains about 400 million sperm cells. Sperm production begins at puberty and continues throughout life, with several hundred million sperm being produced each day. SPERM CELLS The structure of a sperm cell fits its function. The thick head contains the haploid nucleus and is tipped with a special body, the acrosome. The acrosome contains enzymes that help the sperm penetrate the egg. The neck contains large numbers of mitochondria that provide ATP for movement. The tail is a flagellum which moves the sperm. During ejaculation, the sperm are propelled from the epididymis through the muscular VAS DEFERENS ducts, which run from the scrotum around and behind the bladder, where they join to form a short EJACULATORY DUCT. This duct opens into the URETHRA, the tube which drains both the excretory and reproductive systems (never both at the same time). The urethra runs through the penis and opens to the outside at the tip of the penis. In addition to the testes and ducts, the male reproductive system contains three sets of glands that add their secretions to the SEMEN (the fluid ejaculated). 1. SEMINAL VESICLES: contribute about 60% of the total volume of semen. This pair of glands lies below and behind the bladder and empties into the ejaculatory duct. The fluid is thick and clear and contains mucous, amino acids, and large amount of fructose (which provides energy for the sperm). These vesicles also secrete PROSTAGLANDINS, which once in the female reproductive tract, stimulate contractions of the uterine muscles that help move the semen up into the uterus. Proteins in the seminal fluid cause the semen to coagulate after it is deposited in the female, thus, making it easier for uterine contractions to move the semen. 2. PROSTATE GLAND: This is the largest of the accessory glands. Prostatic fluid is thin, milky, and quite alkaline, which balances the acidity of any residual urine in the urethra and the natural acidity of the vagina. 2. PROSTATE GLAND: This gland is the sources of some of the most common medical problems of men over 40. A benign enlargement of the prostate occurs in more than ½ of all men in this age group. That is why it is important to get tested annually after the age of 40. 3. BULBOURETHRAL GLANDS (cowper’s gland): These are a pair of small glands along the urethra below the prostate. They secrete a viscous fluid before emission of the semen. It has been suggested that this fluid lubricates the penis and vagina, but the volume (just one or two drops) seems insufficient to be very effective for this function. This fluid does carry some sperm released before ejaculation,. This is one factor in the low success rate of the withdrawal method of birth control. The penis is composed of spongy tissue derived from modified veins and capillaries. During sexual arousal, this erectile tissue fills with blood from the arteries. As it fills, the increasing pressure seals off the veins that drain the penis, causing it to engorge with blood. The resulting erection is essential to insertion of the penis into the vagina (rodents, raccoons, walruses, and several other mammals also possess a baculum, a bone that stiffens the penis). The main shaft of the penis is covered by relatively thick skin, whereas the head (or glans penis) has a much thinner covering and is consequently more sensitive to stimulation. The human glans is covered by a fold of skin called the foreskin (or prepuce). Foreskin Glans penis Viagra is used for the treatment of male impotency. The active ingredient in Viagra is an inhibitor which allows for increased blood flow into the penis, which may result in an erection. Normally, sexual stimulation in the male is followed by release of nitric oxide (NO) in the penis. Nitrous oxide activates an enzyme which allows for the relaxation of the penile arteries and an increase flow of blood into the penile cavity. The effect of Viagra is to magnify the effect of Nitrous Oxide release. One of the curious side effects of Viagra is an effect on the visual discrimination of certain colors. MALE SEX HORMONES The principal male sex hormones are the androgens, of which, testosterone is the most important. Androgens are steroid hormones produced by the interstitial cells of the testes, and are directly responsible for the primary and secondary sex characteristics of the male. Androgens are also potent determinants of behaviour in mammals. In addition to specific sexual behaviour and libido (sex drive), androgens increase general aggressiveness. CONSEQUENCES OF USE: *ROID RAGE (extreme uncontrollable aggression) * Irritable and depressed. * Low sex drive * Possible cancer & liver damage * Feminizing effects in males (growth of breast tissue)… * Shrunken testicles… * Limb loss… * Heart disease/heart attacks… * HIV/AIDS from the sharing of needles… CONSEQUENCES OF USE: * Reduced sperm count… * Impotence & Infertility… * Baldness… * Pain & difficulty urinating… * Enlarged prostate… * Adolescents experience stunted growth… MALE SEX HORMONES Primary sex characteristics: development of the vas deferens and other ducts, the external genitalia, and sperm production. All babies start as female. If testosterone is present, they will become male, if not, they will be born female. Sex is determined by 13 weeks, sex is determined. MALE SEX HORMONES Secondary sex characteristics: features we associate with maleness such as: deepening of the voice, the male distributions of axillary (armpit), facial, and pubic hair, and muscle growth (androgens stimulate protein synthesis). The hypothalamus makes a hormone called GnRH (the gonadotropin-releasing hormone). GnRH control the release of two hormones from the anterior pituitary: 1. Follicle-stimulating hormone (FSH) 2. Luteinizing hormone (LH) LH stimulates the interstitial cells in the seminiferous tubules to secrete testosterone. Testosterone has a role in sperm production and developing male secondary sex characteristics. FSH acts on the epidymis to help in sperm maturation. Negative feedback by testosterone controls the actions of GnRH. Hypothalamus - GnRH Hypothalamus - GnRH Anterior Pituitary LH & FSH Hypothalamus - GnRH Anterior Pituitary LH & FSH FSH Follicle stimulating hormone Hypothalamus - GnRH Anterior Pituitary LH & FSH FSH Follicle stimulating hormone Epidydimis Hypothalamus GnRH - Anterior Pituitary LH & FSH FSH Follicle stimulating hormone Epidydimis Matures the sperm (makes it motile) Hypothalamus GnRH - Anterior Pituitary LH & FSH FSH Follicle stimulating hormone Epidydimis Matures the sperm (makes it motile) Fish swim Hypothalamus - GnRH Anterior Pituitary LH & FSH LH luteinizing hormone FSH Follicle stimulating hormone Epidydimis Matures the sperm (makes it motile) Hypothalamus - GnRH Anterior Pituitary LH & FSH LH luteinizing hormone FSH Follicle stimulating hormone Interstitial Cells Epidydimis Matures the sperm (makes it motile) Hypothalamus - GnRH Anterior Pituitary LH & FSH LH luteinizing hormone FSH Follicle stimulating hormone Interstitial Cells Epidydimis Testosterone Matures the sperm (makes it motile) Hypothalamus GnRH - Anterior Pituitary LH & FSH LH luteinizing hormone FSH Follicle stimulating hormone Interstitial Cells Epidydimis Testosterone Sperm production 2o sex characteristics deep voice, body hair, more muscle, libido… Matures the sperm (makes it motile) Hypothalamus GnRH - Anterior Pituitary LH & FSH Teens have a Love Hate relationship with testosterone LH luteinizing hormone FSH Follicle stimulating hormone Interstitial Cells Epidydimis Testosterone Sperm production 2o sex characteristics deep voice, body hair, more muscle, libido… Matures the sperm (makes it motile) # Learning Outcome Text Pages P7 P. 418-419 Identify and give a function for each of the following: ovaries (follicles and corpus luteum), oviducts (fallopian tubes), uterus, cervix, vagina, clitoris. P8 Describe the functions of estrogen. P. 421-424 P9 Describe the sequence of events in the ovarian and uterine cycles. P. 420-423 P10 Demonstrate knowledge of the control of the ovarian and uterine cycles by hormones. P. 420-423 P11 Demonstrate knowledge of a positive feedback mechanism involving oxytocin. P. 208, 394 P12 Describe the hormonal changes that occur as a result of implantation. Page 424 The female gonads, ovaries, are located within the lower abdominal cavity, below most of the digestive system. Each ovary is enclosed in a tough protective capsule and contains many follicles. A FOLLICLE consists of one egg cell surrounded by one or more layers of follicle cells, which nourish and protect the developing egg cell. All of the 400,000 follicles a woman will ever have are formed at birth. Of these, only several hundred will be released during the woman’s reproductive years. After puberty, one (or rarely two or more) follicles matures and releases its egg during each menstrual cycle. The cells of the follicle also produce the primary female sex hormones, ESTROGEN. When ovulation occurs, the egg is expelled from the follicle (like a small volcano). http://images.google.ca/imgres?im gurl=http://embryology.med.unsw.e du.au/notes/images/week1/ovary/o vulation2.jpg&imgrefurl=http://embr yology.med.unsw.edu.au/notes/we ek1_3a.htm&usg=__pB3lCLviCh_ XmsldLUuEKzfEfv4=&h=240&w=3 20&sz=6&hl=en&start=4&tbnid=vN xEKu8b8a3nQM:&tbnh=89&tbnw= 118&prev=/images%3Fq%3Dovula tion%26gbv%3D2%26hl%3Den The remaining follicular tissue grows within the ovary to form a solid mass called the CORPUS LUTEUM. The corpus luteum secretes PROGESTERONE (the hormone of pregnancy) and additional estrogen. If the egg is not fertilized, the corpus luteum degenerates and a new follicle matures during the next cycle. The female reproductive system is not completely closed. The egg cell is expelled into the abdominal cavity near the opening of the OVIDUCT (or fallopian tube). The fimbriae on the oviduct sweep the ovary for the egg, and the cilia on the inner epithelium lining the duct help collect the egg cell by creating a current to draw fluid into the duct. The oviduct is the site of fertilization. The cilia in this duct also convey the egg cell down the duct to the UTERUS (womb). The UTERUS is a thick, muscular organ (shaped like an upside down pear). It is remarkably small; the uterus of a woman who has never been pregnant is about 7 cm long and 4-5 cm wide at its widest. The unique arrangement of muscles that make up the uterine wall allow it to expand to accommodate a 4 kg (9 lb) fetus. The inner lining of the uterus, the ENDOMETRIUM, is richly supplied with blood vessels, in which a fertilized egg implants and develops. The narrow neck of the uterus is the CERVIX, which opens into the VAGINA. The vagina is a thin-walled chamber that forms the birth canal through which the baby is expelled; it is also the receptacle for the man’s penis. The vagina is the terminal portion of the female reproductive system, but it is covered by two pairs of skin folds. The female external genitals are collectively known as the vulva. The labia minora are the inner folds of skin just outside the vaginal opening. They are composed of erectile tissue and enlarge during arousal/intercourse. The labia majora, a pair of thick, fatty ridges, cover and protect the genital area. At the top of these two folds is a small bulb of erectile tissue called the glans clitoris, which is the female equivalent of the glans of the penis. Like that organ, it is one of the most sensitive points of stimulation in sexual response. The mammary gland (breast) is another structure important to mammalian reproduction, although it is not part of the reproductive tract itself. The secretory apparatus consists of a series of alveoli, small sacs of epithelial tissue that secrete milk. The aveoli drain into a series of ducts that open at the nipple. The lack of estrogen in males prevents the development of both the secretory apparatus and the fat deposits, so the breasts remain small and the nipple is not connected to the ducts. OOGENESIS The ovary contains many follicles composed of a developing egg surrounded by an outer layer of follicle cells. Each egg begins oogenesis as a primary oocyte. The development of ova (mature, unfertilized eggs) differs from spermatogenesis in three ways. 1. During meiotic divisions of oogenesis, cytokinesis is unequal, as only 1 of the four cells will develop into an ovum, the other 3 are called polar bodies (which help to nourish the egg). 2. At birth each female carries all of the egg cells it will ever have, though still in an immature state. 3. Oogenesis is cyclical. It has long ‘resting’ periods before the process is complete. After puberty, a developing egg is released each month from puberty until menopause, a total of 400-500 eggs. THE FEMALE HORMONES The pattern of hormone secretion controlling female reproduction differs strikingly from the male pattern, mostly due to its cyclical nature. Whereas the male produces sperm continuously, females ovulate only one or a few eggs at one time during each cycle. The control of this cycle is complex. THE FEMALE HORMONE CYCLES Two different types of cycles occur in the female mammals: 1. The menstrual cycle 2. The ovarian cycle The Menstrual Cycle The human menstrual cycle refers specifically to the changes that occur in the uterus. It lasts an average of 28 days, but only ~30% of women have cycle lengths within a day or two of the statistical 28 days. Cycles vary from about 20 to 40 days. In some women the cycles are usually very regular, but in other individuals the timing varies from cycle to cycle. MENSTRUAL CYCLE : This cycle occurs in the uterus. There are 3 phases in this cycle. Day 1 is the first day of a woman’s ‘period’ (1st day of menstruation) THREE PHASES OF THE MENSTRUAL CYCLE 1. The Flow phase: Menstrual bleeding usually persists for a few days (day 2-8). 2. The Proliferative phase: the endometrium begins to thicken for a week or two (until ovulation). 3. The Secretory phase: usually about 2 weeks long, the endometrium continues to thicken, becomes more vascularized and secretes a fluid rich in glycogen to prepare for a fertilized egg. MENSTRUAL CYCLE *If an embryo has not implanted in the uterine lining by the end of the secretory phase, a new menstrual flow commences. *If an embryo is implanted before the end of the secretory phase, the endometrium will remain until birth. THE OVARIAN CYCLE: This cycle occurs in the ovaries. There are THREE phases in this cycle THREE PHASES OF THE OVARIAN CYCLE: 1. This cycle begins with the FOLLICULAR PHASE, during which several follicles in the ovary begin to grow and release estrogen. The maturing follicle develops an internal fluid-filled cavity and grows very large, forming a bulge near the surface of the ovary. THREE PHASES OF THE OVARIAN CYCLE: 2. The follicular phase ends with OVULATION when the follicle and adjacent wall of the ovary rupture, releasing the egg cell. The egg cell is transported into the oviduct and is transported into the uterus. THREE PHASES OF THE OVARIAN CYCLE: 3. The last phase is the LUTEAL PHASE. During this phase, the follicular tissue that remains in the ovary after ovulation is transformed into the corpus luteum. The corpus luteum is an endocrine tissue that synthesizes and secretes hormones to prepare the uterus for pregnancy. The next cycle begins with growth of new follicles. These cyclic phases are interrupted only by pregnancy and continue until menopause, when reproductive capability ends. THE FEMALE SEX HORMONES Hormones coordinate the menstrual and ovarian cycles in such a way that growth of the follicle and ovulation are synchronized with preparation of the uterine lining for possible implantation of an embryo. 5 hormones participate in both (+) and (-) feedback cycles: 1. Gonadotropin-releasing hormone (GnRH): secreted by the hypothalamus 2. Follicle stimulating hormone (FSH): secreted by anterior pituitary 3. Luteinizing hormone (LH): secreted by anterior pituitary 4. Estrogen: secreted by ovary (follicle) 5. Progesterone: secreted by ovary (corpus luteum) 1. During the follicular phase of the ovarian cycle, the hypothalamus releases GnRH. 2. This causes the anterior pituitary to secrete small quantities of FSH and LH. 3. At this time, the follicles in the ovary have receptors for FSH, but not for LH. The FSH causes the follicles to grow. 4. The follicles release estrogen as they grow. The amount of estrogen secreted during this time is small. 5. When the [estrogen] secretion begins to rise, it causes the hypothalamus to release more GnRH (positive feedback). 6. GnRH causes even more LH and FSH to be released from the anterior pituitary. 7. This causes the LH SURGE. 8. By now, the follicles have receptors for LH and can respond to this hormonal cue. The LH SURGE induces final maturation of the follicle. 9. Ovulation occurs on day 14, about one day after the LH surge. 10. After ovulation, LH will stimulate the follicle to become the corpus luteum. 11. LH will also stimulate the corpus luteum to start secreting estrogen and progesterone. 12. The corpus luteum reaches its maximum development about 8-10 days after ovulation. At this point there is very high [progesterone] and [estrogen] in the blood. 13. High levels of these hormones exerts negative feedback on the hypothalamus. 14. This causes a severe decrease in the amounts of LH and FSH. 15. When [LH] plummets, the corpus luteum begins to degenerate. 16.This causes a sharp decrease in the [estrogen] and [progesterone]. 17. Without these hormones, the endometrium layer is sloughed off and day one of the cycle begins again. 18. As these hormones drop off, the hypothalamus and pituitary are not inhibited anymore. 19. So the anterior pituitary begins to secrete enough FSH to stimulate growth of new follicles in the ovary. 20. This initiates the follicular phase of the next ovarian cycle. How is the ovarian cycle synchronized with the menstrual cycle? 1. Follicular phase/proliferative phase: Estrogen (which is released by follicles in the follicular phase) is a hormonal signal to the uterus, which stimulates the development of the endometrium (proliferative phase). FOLLICULAR PHASE e s t r o g e n PROLIFERATIVE PHASE How is the ovarian cycle synchronized with the menstrual cycle? 2. Luteal phase/secretory phase: After ovulation, estrogen and progesterone secreted by the corpus luteum stimulate continued development and maintenance of the endometrium (secretory phase) as the body prepares for the possibility of a fertilized egg. LUTEAL PHASE p r o g e s t e r o n e SECRETORY PHASE How is the ovarian cycle synchronized with the menstrual cycle? 3. A rapid drop in the level of estrogen and progesterone hormones when the corpus luteum degenerates causes spasms of the arteries in the uterine lining that deprive the endometrium of blood. Degeneration of the endometrium results in menstruation and the beginning of a new menstrual cycle. In the meantime, ovarian follicles that will stimulate renewed thickening of the endometrium are just beginning to grow. Corpus luteum dies L o w E & P MENSES Day 1 Review of female cycles: http://images.google.ca/imgres?imgurl=http://www.msnbc.com/news/wld/graphics/menstrual_cycle_dw.jpg&imgrefurl=http://ww w.msnbc.com/news/wld/graphics/menstrual_cycle_dw.htm&usg=__xUXLpPolNSPez1cMkDlGK_zxU4w=&h=400&w=520&sz= 30&hl=en&start=24&tbnid=Wua0J3g_usMtPM:&tbnh=101&tbnw=131&prev=/images%3Fq%3Dmenstrual%2Bcycle%26start% 3D20%26gbv%3D2%26ndsp%3D20%26hl%3Den%26sa%3DN In addition to their role in coordinating reproductive cycles, estrogens are also responsible for the secondary sex characteristics of the female: 1. Deposition of fat in the breasts and hips 2. Increase in water retention 3. Affects calcium metabolism 4. Stimulates breast development 5. Mediates female sexual behavior 6. Initiates female libido 7. PMS 8. Mood swings 9. Cravings (chocolate, cheese, milk…) 10. Growth of hair (not as much as men) If the egg is fertilized, the resulting embryo will start to release a hormone called human chorionic gonadotropin (HCG). HCG acts like LH to maintain the corpus luteum and this allows the levels of progesterone and estrogen to remain high. Thus, the endometrium layer is NOT sloughed off and is maintained by the high levels of hormones. The levels of HCG are so high, that some is excreted in the urine, where it can be detected in pregnancy tests. HCG Other changes for the mother in the first trimester include: •Increased mucous in the cervix to form a protective plug. •Growth of the placenta •Enlargement of the uterus •Morning sickness •Mood swings •Weight gain of ~1kg •Cessation of ovulation and menstrual cycling •Breasts become large and tender Oral contraceptives (birth control pills) usually contain a combination of estrogen and progesterone. High levels of these hormones prevent the release of FSH and LH, and thus inhibit the development of any new follicles. And this means no eggs released and no fertilization possible. This tricks your body into thinking you are pregnant. The days that you take a placebo, would be the days you have your period. OTHER OPTIONS? 1. Time-release capsules (Norplant) can be implanted under the skin and offer long-term suppression of ovulation. May double the risk of blood clots. 2. There is also an injection available, which you receive once every 3 months (it acts similarly to the pill). 3. RU-486, the ‘morning after pill’, interferes with implantation of the blastula into the uterine wall. Its use as a contraceptive is very controversial. 4. Barrier methods: physical (condom, diaphragm) or chemical (spermacides) means to separate the sperm from the egg. 5. Physical prevention (most effective) include vasectomy and tubal ligation. Male fruit bat of the species Rousettus aegyptiacus have testes that are 2.15 % of body mass, whereas their brains are only 1.70 %. The males in some bat species can have testes that are up to 8.5 % of their body mass. It is a baculum, or penis bone, of an extinct species of walrus. The 12,000 year old fossil was discovered in Siberia. What remains is a 4 ½ foot piece of dry muscle tissue and weathered skin.