Chapter 19
advertisement

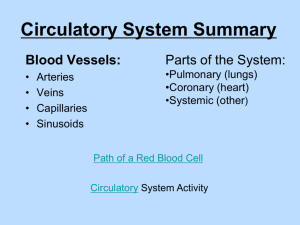
Chapter 19: The Cardiovascular System: Blood Functions of Blood ________________ Oxygen from lungs to cells, CO2 from cells Nutrients from GI tract Hormones Heat and waste ___________ Homeostasis of body fluids pH, temperature, osmotic pressure _______________- from excessive blood loss & disease Clotting WBC Proteins, Ab, interferon, complement Components, Fig 19.1, table 19.1 _____________ - 55% of whole blood Water, proteins, others __________________- 45% RBC = erythrocytes (4.8- 5.4 million/l blood) WBC = leukocytes, 5 types, (5-10,000/ l blood) Agranulocytes= Lymphocytes, monocytes Granulocytes= Neutrophils, eosinophils, basophils Platelets = thrombocytes; from megakaryocytes; (150-400,000/l) Plasma, specific components Water Solutes Proteins- albumin, globulins, clotting factors Antibodies are _________________- produced during immune responses against bacteria & viruses Nutrients- simple sugars, amino acids, fats Electrolytes- various salts Gases- oxygen and carbon dioxide Waste products- byproducts of metabolism: urea, uric acid, creatinine, ammonia, bilirubin Normal blood smear Physical characteristics Denser, more viscous than water Temp = 38°C = 100.4°F Slightly alkaline pH = 7.35 - 7.45 ___________________________ is blood 8% body mass _____________ (1.5 gal) in average male 4-5L (1.2 gal) in avg. ♀ Formation of blood cells Fig 19.3 ____________- how formed elements are made Before birth- in yolk sac of embryo In fetus- liver, spleen, thymus and lymph nodes Red bone marrow - 1° site last 3 months of fetal development & continues to be thru out life Highly vascularized Microscopic spaces in spongy bone From pluripotent stem cells Rate of production in adulthood and becomes predominantly yellow bone marrow Marrow sinusoids (enlarged, leaky capillaries) circulation Red Blood Cells = Erythrocytes General Structure: biconcave disk, 7-8 μm Function: ____________________ Hemoglobin (Hb) – oxygen carrying protein that gives blood it’s red color, binds 4 oxygen molecules ______________- % of total blood volume that is occupied by RBC Normal range adults: ♀ 38-46%, ♂ 40-54% Testosterone stimulates erythropoietin- hormone that stimulates RBC production Production – new mature RBC must enter the bloodstream at least 2 million/ second to = their rate of destruction Structural Characteristics RBC Physiology ____________________ for oxygen transport No nucleus, all space for oxygen storage Lack mitochondria for ATP generation do not USE any of the O2 they transport Shape facilitates function ↑ surface area ↑ surface for gas diffusion 280 million Hb / RBC, each Hb can bind 4 O2 120 day life–wear & tear, no nucleus no repair Destroyed in spleen and liver & recycled ________ on plasma membrane account for ABO blood types & Rh factor Hb = 2α, 2β chains; 1 heme with Fe2+ /chain Figure 19.5 formation & destruction Erythropoiesis Figure 19.6 Production of RBC Start in RB marrow w/ proerythroblast Divides several times Ejects nucleus reticulocyte = immature Loss of nucleus causes indentation ______________ pass from RB marrow to bloodstream- squeeze thru endothelial cells of capillaries called sinusoids RBC destruction Fig. 19.5, 6 If erythropoiesis ≠ destruction, neg. feedback loop to ↑ RBC production If cellular oxygen is deficient = _________, stimulates kidney to release erythropoietin High altitude – lower O2 content in air Circulatory problems ________- # RBC or Hb content low (some causes:) • Lack of iron • Lack of certain a.a. • Lack Vitamin B12 Breakdown & recycling at liver, spleen, or RB marrow Erythrocyte Disorders ________________ – disorder characterized by > normal hematocrit (>55%) in which hypertension, thrombosis (clot in an unbroken vessel), & hemorrahage (bleeding) can occur Anemias- O2 carrying capacity reduced, fatigued, intolerant to cold, may appear pale: Iron deficiency Megoblastic- inadequate Vitamin B12 or folic acid Pernicious- insufficient hemopoiesis Hemorrhagic- excessive loss of RBC Hemolytic- RBC rupture prematurely Thalassemia- Hb deficiency Aplastic- destruction of RB marrow Erythrocyte disorders (2) Fig 19.14 Sickle-Cell Disease (SCD) – RBC contain Hb-S, an abnormal Hb Hb-S gives up oxygen to interstitial fluid it forms a long, rod-like structure, sickle shape Some degree of ____________ Mild ____________- yellowness of skin, eyes, membranes due to build up of bilirubin Joint, bone pain; breathlessness, rapid h.r., fever, fatigue due to tissue damage & oxygen debt __________________ 2 defective genes = severe one gene = minor problems Leukocytes = WBC Fig. 19.7, 8 Types: granular and agranular All have nuclei, no Hb Functions- each of 5 have specific functions See table 19.3 Far less numerous than RBC Avg 5-10,000 cells / μl of blood ________________________ > 10,000 cells / μl of blood • Normal protective response: microbes, strenuous exercise, anesthesia, surgery ________________________ < 5,000 cells / μl of blood • Never beneficial– caused by radiation, shock, chemotherapy Cell life = hours to few days, but T & B memory can live for many years once established Granulocytes fig 19.7, table 19.3 ______________________= 60-70% Phagocytosis destruction of bacteria w/ lysozyme, defensins, & strong oxidants ______________________= 2-4% combat histamine effects in allergic rxns phagocytize A-Ab complexes destroy certain parasitic worms _______________ = 0.5-1% liberate heparin (prevents clotting) histamine (vasodilate, ↑perm of bv, constricts airway) serotonin in allergic rxns Agranulocytes fig 19.7, table 19.3 __________________ = 20-25% mediate immune responses- A-Ab rxns B cells develop into plasma cells, secrete Ab T cells attack invading viruses, cancer cells, transplanted tissue cells Natural killer cells attack wide range of infectious microbes & certain spontaneous arising tumor cells ___________________ = 3-8% Phagocytosis transform into fixed or wandering macrophages Emigration (aka diapedesis) Fig 19.8 How WBC leave bloodstream Rolling along the endothelium, stick to it, squeeze between endothelial cells Precise signals stimulate, vary for different types Adhesion molecules- ____________ tether neutrophils to endothelium & assist in movement to ECF Neutrophils & macrophages are phagocytic _____________ -microbe secretions attract phagocytes Neutrophils- quick responders: Lysozyme, strong oxidants, defensins- proteins that exhibit broad range antibiotic activity bacteria & fungi Phagocytosis (in ch 22) Inflammation Immunity State of being resistant to injury, particularly by poisons, foreign proteins, & invading pathogens ______________– due to an individual’s biological makeup Antibodies, skin, stomach acid, mucous, coughing, enzymes in saliva & tears, skin oils ______________ – acquired due to injection of vaccine, dead or attenuated pathogens or immunoglobulins ______________ – resistance to disease or infection due to one’s immune system functioning to produce antibodies ______________ – acquired by transfer of serum from another animal produced by sensitized lymphocyte, or mother to fetus Antigen - Antibody _____________ (A) – substance provoking immunogenicity and reactivity (react w/Ab or cells that result from immune response) On RBC = agglutinogens = glycoproteins or glycolipids Categorized the blood groups: A, B, AB, O; also Rh ____________ (Ab) - protein produced by a plasma cell to specific antigen Combine with Antigen to neutralize, inhibit or destroy it __________________ – clumping of microorganisms or blood cells due to A-Ab rxn MHC Antigens Major _________________ (MHC) antigens – surface proteins on WBC & other nucleated cells that are unique to each person (except identical twins) Used for tissue typing Leukemias group of RB marrow cancers, abnormal WBC multiply uncontrollably accumulation of cancerous WBC interferes w/production of RBC, WBC & platelets O2 carrying capacity , more susceptible to infection, abnormal clot Cancerous WBC spread to lymph nodes, liver, & spleen causing enlargement Anemia, weight loss, fever, night sweats, excessive bleeding, recurrent infections Cause- unknown, risk factors: radiation, chemotherapy, genetic disorders, environmental factors, microbes Acute- symptoms develop rapidly (adults or children) Chronic- take years to develop (usually just adults) Treatment- chemotherapy, radiation, stem cell transplant, interferon, Ab, blood transfusion Platelet formation Hemostasis Fig 19.11 1. _____________ – smooth muscle contraction in rxn to damage 2. ______________________ – platelets adhere, activate, liberate contents, aggregation forms plug 3. ___________________ – fibrin threads form 4. ________________________ - contraction of fibrin threads to tighten clot, release factors to strengthen 5. ______________ – enzyme digests clot Fibrinolytic system – dissolves small inappropriate clots Streptokinase – first thromolytic agent for dissolving clots in coronary arteries, approved 1982 Coagulation time Time required for blood to coagulate, 2-6 min Can be prolonged due to the following: __________________ – X chromosome linked disorder resulting in deficiency of clotting factor VIII (type A) or deficiency of factor XI (type B & C) Spontaneous or traumatic subcutaneous intramuscular hemorrahaging, nose bleeds, blood in urine Obstructive jaundice – obstructing bile flow Some anemias and leukemias Some of infectious diseases Blood typing Fig 19.12-19.14 Human Blood Groups ABO Blood Groups Rh Blood Groups Transfusion rxns: Agglutination Hemolysis Blood Typing Table 19.5 - frequency of types Table 19.6 - group interactions Transfusion RBC only or blood plasma only is transferred into the bloodstream or directly into red bone marrow INCOMPATIBLE BLOOD TYPE: Agglutination rxn – recipient’s ____________bind to the _____________ A-Ab complex activate plasma proteins to the complement family Make the plasma membrane of donated cells leaky _________________ – rupture of cells, loss of Hb Rh factor Fig 19.13 Antigen discovered in Rhesus monkey Rh+ have antigen, Rh- do NOT have antigen Normally, plasma does not contain anti-Rh Ab If Rh- person receives Rh+ transfusion immune system will start to make anti-Rh Ab that will remain in blood. Problem: _____________ of Rh+ occurs later, Anti-Rh Ab that have been building can cause agglutination of donated blood hemolysis Hemolytic disease of newborn (HDN)- if fetal blood (Rh+) leaks across placenta, exposure to Rh-A mother (Rh-) making anti-Rh, prob – 2nd baby RH+