Peanut and Other Food Allergies: From Diagnosis to Desensitization
advertisement

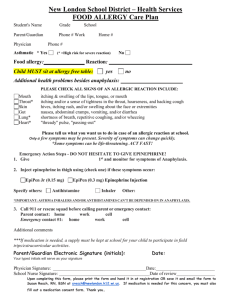
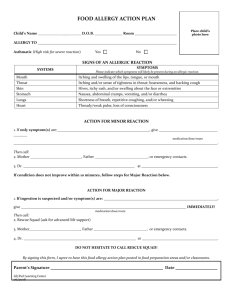
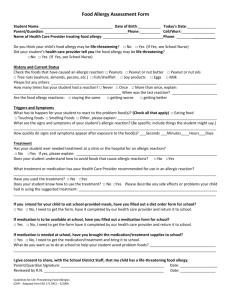
Peanut and Other Food Allergies: From Diagnosis to Desensitization Jeffrey M. Factor MD Associate Clinical Professor of Pediatrics University of CT School of Medicine March 29, 2012 Food Allergies: Epidemiology • Prevalence of food allergy has increased by 18% in past 15 yrs (4 million school-aged children) • Peanut allergy in US has tripled (0.4% to 1.4%) from 1997 to 2008 • Food allergy is now most common cause of anaphylaxis presenting to emergency departments • Hospitalizations have increased 3-fold in past decade in US • Fatalities do occur (~150-200/yr) majority due to peanut/tree nuts Hospital Discharges w/ DX of Food Allergy Adverse Reactions to Food A. Non-immunologic Toxic Reactions • Bacterial food poisoning • Scromboid fish poisoning • Caffeine • Alcohol • Histamine Non-Toxic Reactions Lactose Intolerance Galactosemia Pancreatic insufficiency Gustatory rhinitis Anorexia Nervosa Idiosyncratic Adverse Reactions to Food B. Immune Mechanisms-A Spectrum IgE-Mediated • Systemic (Anaphylaxis) • Oral Allergy Syndrome • Hives • Immediate GI allergy Non-IgE Mediated Eosinophilic Esophagitis (EoE) or Gastroenteritis (EG) Atopic dermatitis Protein-Induced Enterocolitis (FPIES) Celiac Disease Enteropathy Infant Proctocolitis Dermatitis Herpetiformis N Engl J Med Vol. 346, No 17 N Engl J Med Vol. 346, No. 17 IgE-Mediated Food Allergy Signs and Symptoms SKIN Hives/angioedema Flushing Papular red rash Pruritis GASTROINTESTINAL Itching or swelling of lips, tongue, mouth Nausea Vomiting or reflux Abdominal cramping Diarrhea IgE-Mediated Food Allergy Signs and Symptoms RESPIRATORY Mild-Congestion, itching, sneezing, runny nose, cough Severe-Laryngeal edema, hoarseness, drooling, wheezing, shortness of breath, CARDIOVASCULAR Feeling of faintness Syncope Tachycardia or bradycardia Hypotension/shock Arrhythmias Robby 8-year-old with peanut allergy since age 2 yrs. At age 2, he developed hives around the mouth and swelling after eating peanut candy. At age 6, he had a generalized rash and some difficulty breathing after eating a few bites of a peanut candy. At age 8, he developed an itchy mouth and lower lip swelling after eating a piece of chocolate candy (not known to contain peanut) which resolved by itself without any treatment. What would your prescribed Anaphylaxis Emergency Action Plan be for Robby? 1. Liquid diphenhydramine at start of next reaction; watch for 20 minutes; if it worsens, call 911. 2. Use self-injectable epinephrine at the start of the next reaction, even if only mild symptoms, and call 911. 3. Do nothing; the reaction will go away by itself. 4. Drive to the ER but have the self-injectable epinephrine ready for use in case things get worse. What would your prescribed Anaphylaxis Emergency Action Plan be for Robby? 1. Liquid diphenhydramine at start of next reaction; watch for 20 minutes; if it worsens, call 911. 2. Use self-injectable epinephrine at the start of the next reaction, even if only mild symptoms, and call 911. 3. Do nothing; the reaction will go away by itself. 4. Drive to the ER but have the self-injectable epinephrine ready for Food Anaphylaxis • Definition: an acute systemic allergic reaction that is potentially fatal • The opposite of prophylaxis “without or against protection” • Onset of symptoms seconds to minutes (up to 2 hrs) following ingestion • Prior reactions may have been milder • Very unpredictable in its clinical presentation and outcome Patterns of Anaphylaxis • Uniphasic – Rapid onset, symptoms resolve within hours of treatment • Biphasic – Symptoms resolve after treatment but return between 1 and 72 hours later (usually 1-3 hours) • Protracted – Symptoms do not resolve with treatment and may last >24 hours Lieberman, 2004 Uniphasic Anaphylaxis Treatment Initial Symptoms 0 Antigen Exposure Time Biphasic Anaphylaxis Treatment Initial Symptoms Treatment 1-8 hours 0 Antigen Exposure SecondPhase Symptoms Classic Model 1-72 hours New Evidence Time Protracted Anaphylaxis Initial Symptoms Time 0 Antigen Exposure Possibly >24 hours Features of Fatal/Near Fatal Reactions in Children (Sampson et al, NEJM, 1992) • Known allergy to causative food • Did not ask about ingredients, were misinformed or incorrect labeling of product • Injectable epinephrine not carried or administered in a timely fashion • Co-morbidity: asthma • Skin reactions (hives, swelling) were not present in most cases Treatment: Epinephrine • Treats all symptoms of anaphylaxis and prevents progression (antihistamines DO NOT) • Intramuscular injection in lateral thigh produces most rapid rise in blood level – 0.01 mg/kg in children, 0.3-0.5 mg in adults • Patients who receive epinephrine and have symptoms other than hives should be lying down with feet elevated • Up to 20% of time, more than one dose needed • Newer recommendations: have 2 devices Side Effects of Epinephrine • Tachycardia • Tremor • Pain at injection site • Nausea • Vomiting IM vs SQ Epinephrine Intramuscular epinephrine + - 8 (Epipen®) 2 minutes Subcutaneous epinephrine 34 + - 14 (5 – 120) minutes p < 0.05 0 10 20 30 40 Time to Cmax after injection (minutes) Simons: J Allergy Clin Immunol 113:838, 2004 Additional Treatment of Anaphylaxis • Oxygen • Fluid replacement (10-20 cc/kg) • H-1 antagonists (eg. Diphenhydramine) and H-2 antagonists (eg. Ranitidine) • Corticosteroids-but no proven benefit • Severe cases: IV epinephrine, vasopressors • Observe for 4-24 hrs after initial symptoms have subsided High Risk Population: Adolescents • More likely to eat meals and snacks outside the home • More likely not to carry their epinephrine autoinjector on their person • Take more chances with food…do not think about mortality • Keep their food allergy issues to themselves • Are afraid to use their epinephrine autoinjector-less empowered Kaitlyn 14-year-old with spring allergic rhinitis who complains of mouth itching and lip swelling every time she eats an apple. Also, complains of similar symptoms with peaches, cherries and raw carrots. Mom thinks she is “making it up.” The Most Likely Diagnosis Is 1. Child is a Hypochondriac 2. Oral allergy syndrome 3. Celiac Disease 4. Systemic Food Allergy (early symptoms) Oral Allergy Syndrome (Pollen/Food Allergy Syndrome) • Very common form of IgE-mediated food allergy • Occur in 40%-50% of pollen allergic individuals • Itching of lips, mouth, throat due to cross-reacting proteins in pollen and fruit • Uncommon to progress to severe reactions but occasionally occurs (throat tightness/hoarseness are not mild symptoms) • Treatment: heating, peeling fruit or avoidance during pollen season, immunotherapy (allergy shots to related pollen) may lessen reactions Oral Allergy Syndrome Examples: Pollen Birch Ragweed Grass Foods Apple, peach, cherry, kiwi, plum, hazelnut and almond Banana, melon, watermelon Carrot, celery, peach, potato, tomato Food-dependent Exercise-induced Anaphylaxis • Requires food ingestion followed by exercise to occur • Anaphylaxis occurs when patient exercises within 2 to 4 hours of ingesting a food • Can be a specific food (common examples: celery, shellfish, wheat) or could be ANY food • Females>Males (2:1) more in teens, young adults • Management: Identifying specific foods, if possible, avoiding exercise after eating, and carrying epinephrine during vigorous activity Factors which may increase risk of allergic reactions • Preparation: roasting vs. boiling of peanuts • Chemical properties of food: heat stable vs. heat labile proteins (the oral allergy syndrome) • Concurrent viral illness esp. w/fever • Medications: beta blockers, ACE inhibitors increase anaphylaxis risk • Alcohol consumption Disorders Not Proven to be Related to Food Allergy • Migraines • Behavioral / Developmental disorders • Arthritis • Seizures • Inflammatory bowel disease Diagnosis: History / Physical • History: symptoms, timing, reproducibility – Acute reactions vs chronic disease • Diet details: specific causal food(s) or hidden ingredients • Physical examination: look for other allergic conditions (eczema, asthma) • Identify the type of reaction: – Is it food related at all? – Allergy or intolerance? – IgE type reaction or non-IgE type reaction? Diagnosis: Laboratory Evaluation • Suspect IgE-mediated (allergy) – Prick skin tests – ImmunoCAP /RAST test (IgE levels in blood) • Suspect non-IgE-mediated – Allergic gastrointestinal conditions -- Elimination diets may be helpful • Suspect not allergic, consider: lactose intolerance, toxic reactions, celiac disease (gluten-sensitivity) Skin Testing • Provide rapid screening for sensitivity to allergens • Less discomfort and cost compared to blood tests • Size of skin test may be helpful in predicting likelihood of reacting • Negative skin tests strongly suggest the absence of IgE-mediated allergy • May need to skin test with fresh foods Blood Tests for Foods • ImmunoCAP/RAST test measure specific IgE antibody levels to different foods in the blood • Are helpful in predicting whether an allergic reaction will occur • High levels less likely to outgrow allergy • Newer blood tests (component diagnostics) should be able to predict the severity of the allergy (eg. peanut-Ara h 2 vs Ara h 8) Limitations of Tests • Blood test ‘screening’ not advised because may lead to unnecessary or harmful dietary restriction which can frustrate and confuse parents/patients • Size of skin test and numerical value (ie. absolute # or level I-IV) of the blood test do not predict severity of the clinical reaction • A blood test level of <0.35Ku/L is not necessarily negative, but rather the lowest level that the assay can measure • Patients can have food reactions with levels of <0.35Ku/L • So false positives and false negatives do occur and these tests must be looked upon in the context of the history 812 Sampson J Allergy Clin Immunol May 2004 Oral Food Challenge • The definitive test for food allergy diagnosis • Identify what foods can be safely consumed when there are many positive skin or blood tests • To try foods suspected of causing allergic reactions despite negative testing • To monitor patients who have food allergies which are more likely to be outgrown • Performed under close supervision (with emergency medications and equipment immediately available to manage reactions) Why is there more food allergy? • Genetics: peanut allergy 7x greater in sibs of high risk children, 64% in identical twins • Earlier exposure of peanut in childhood may associated w/lower prevalence of PN allergy • Vitamin D deficiency: Lower levels due to less sunlight may be responsible for increase in allergy in temperate areas (evidence: more Epi Rx written in northeast US than in south, more eczema too) • Hygiene hypothesis: Birth by CS associated with increase risk of food allergy (bacterial exposure during vaginal delivery may be protective) Consequences of A Food Allergy Diagnosis • Special precautions required at home, schools, restaurants, friends/relatives, on vacations, etc. • The need for stringent dietary restrictions • Difficulty comprehending food labels • The continual threat of accidental ingestions • The risk of severe or fatal reactions • Significant anxiety, psychosocial stress, and economic burden Standard of Care for Food Allergy • Every food (esp peanuts and tree nuts) allergic reaction has possibility of developing into life-threatening reaction • May depend upon how much of the food is eaten, other ‘co-factors’ • Long-standing principle of complete avoidance of even minute exposures and ready access to self-injectable epinephrine. Natural History of Food Allergy • Most children w/ food allergies will eventually tolerate milk, egg & wheat (many not until teenage years) • Peanuts, tree nuts, fish and shellfish usually not outgrown • High initial allergen blood test numbers associated with lower rate of outgrowing the food allergy • Resolution of atopic dermatitis may be a useful marker for food allergy tolerance • Skin tests to food can remain positive after tolerance has developed, but a decrease in size may be indicator of loss of allergy Effect of Cooking & Digestion on Food Proteins M I M I L 1 K M I L L K K Processing K L 2 Children who “outgrow” milk or allergy will often tolerate baked-milk or baked-egg products M I Treatment of Food Allergies: Recent Approaches • I Allergen non-specific treatment 1) Anti-IgE therapy (an injection every few weeks of a monoclonal antibody which binds to and blocks IgE) 2) Chinese Herbs (inhibits food anaphylaxis in mice, studies in humans ongoing) • II Allergen-specific treatment (directed at individual foods) 1) Oral immunotherapy (OIT) 2) Sublingual immunotherapy (SLIT) 3) Epicutaneous patch Does strict avoidance speed resolution? • For years, recommendation was that strict avoidance was best for tolerance to develop • Principle that lack of exposure will result in deletion of immunologic memory • Many children do outgrow food allergy when instructed to avoid exposure • The concern that accidental ingestions can delay /prevent tolerance development • Maybe this concept is NOT ACCURATE…… Does avoidance trigger increased reactivity? • 7 children who tolerated fish but were instructed to avoid based on positive skin tests. After 2 years of avoidance/reintroduction induced acute reactions in all 7 children. • Case report of teenage girl who died from milk protein anaphylaxis due to loss of tolerance from milk avoidance diet. • Late onset peanut allergy developing in adults who were told to avoid based on positive tests • Peanut recurrence rate ~8%. Seems to affects patients who avoid peanut after resolution of allergy Recent data has challenged the long-standing idea of strict avoidance, instead, attempting to incorporate small amounts of the food into the diet. BAKED GOODS Changing from Avoidance to Limited Diet • 70% of children with egg allergy and 75% of children with milk allergy tolerate these foods in baked goods • Recent studies show ability to eat foods with heated milk/ baked in egg are good prognostic indicators of tolerance • Regular ingestion associated with decrease skin test size • Studies suggest regular ingestion may induce tolerance (loss of allergy) Focus on Treatment of Peanut Allergy • Only about 15-20% will outgrow peanut allergy • Accidental exposures are common • Diagnosis has significant adverse effects on quality of life • Allergic reactions becoming more severe: ER visits and hospitalizations • Currently can’t reliably predict severity of the allergy using skin and blood tests • Oral immunotherapy (OIT) an emerging option Kurihara K. Allergol Int 2010; 59: 9-14. ORAL DESENSITIZE Desensitization – change in threshold dose of food needed to cause an allergic reaction while on ongoing therapy TO INDUCE ORAL TOLERANCE. Tolerance – resolution of allergy without ongoing treatment Historical Case • 1908 – “ A Case of Egg Poisoning” – Schofield described case of 13 y/o boy who had severe egg allergy; treated w/ daily pill containing raw egg starting w/ 1/10,000th of an egg; 8 months later, could eat whole egg • First case reports of oral desensitization appeared ~20 years ago. Case Report of Peanut Oral Desensitization • 2006 – Letter to Editor: 6 y/o girl with severe peanut allergy, RAST >100 IU underwent oral desensitization; Goal: to ensure that child would not have reaction to unintentional modest exposures not to make her eats peanuts as a normal food Final dosing was 2 whole peanuts twice daily Mansfield L. Ann Allergy Asthma Immunol 2006; 97: 266-7. Peanut OIT Study • 4 severely peanut allergic boys, aged 9-13 y/o, underwent oral immunotherapy (OIT) • OIT was administered as peanut flour from 5 to 800 mg (1/2 tsp peanut butter) • Challenges done in medical facility/doses were taken at home once daily x 2 weeks • Continued on 800 mg for additional 6 weeks; 3 tolerated 12 peanuts, 1 tolerated 9 peanuts • Children continued to take 1/2 tsp peanut butter or 5 peanuts as maintenance Clark AT, et al. Allergy 2009; 64: 1218-20. Peanut Oral Immunotherapy – Duke /Univ of Arkansas • Multi-center group studying children with peanut allergies, double-blinded placebocontrolled • 29 children <16 y/o w/ peanut allergy • Protocol: 3-phases: initial dose escalation day, buildup phase, home dosing phase followed by oral food challenges • Goal: Daily maintenance dose of 300 mg of peanut protein Hofman AM, et al. J Allergy Clin Immunol 2009; 124: 286-91. Peanut OIT resulted in clinical desensitization • 27/29 children reached the total peanut dose; 1 stopped due to parent anxiety and other due to hives/vomiting • Oral food challenges with peanut were conducted in all 29 patients after they were on OIT for 12-24 months • Total dose tolerated = 3.9 grams of peanut protein ~16 peanuts Jones SM, et al. J Allergy Clin Immunol 2009; 124: 292-300. Desensitization or Tolerance • Increased daily dose to 4000 grams of peanut • Patients who passed oral food challenges increased daily dose to 19 peanuts/day • After 2-3 years on treatment-tolerance studies were performed • Discontinued therapy for 4 weeks and rechallenged • Only 41% passed (were tolerant to peanut) New England Food Allergy Treatment Center (NEFATC) • Facility in West Hartford designed for treating food allergies by oral immunotherapy • Staff of physicians, nurses, a pharmacist experienced in food allergy management • Treatment focused with upmost concern for safety and comfort of patients/families Goal of Therapy (NEFATC) • Clinical desensitization to peanut • Creating a ‘safety net’ • Minimize the likelihood of an allergic reaction upon accidental ingestion • Substantially improve quality of life as measured for children, adolescents, and parents perception of their children Peanut OIT Protocol at NEFATC Dose escalation, build-up, home maintenance phases (use peanut flour, measured with high precision scale) Initial day, 5-6 hours, IV inserted, 0.1 mg (1/2000 peanut) increased every ½ hour to 6 mg dose Return every 2 weeks for build-up dose Ingest highest tolerated dose given daily at home Dosage goal = 450 mg/day of peanut (2-3 peanuts) Time to reach maximum dose approximately 5-6 months, depending on patient/symptoms Experience to Date: NEFATC 140 peanut allergic patients have been enrolled Largest population of PN-allergic patients currently receiving OIT Ages 4-24 yrs Many with severe allergy (by history), also serum IgE levels to peanut >100 kU/L in 40% patients Seventy-five patients have reached maintenance dose of 3 peanut M and M’s daily Peanut OIT: Adverse Effects • GI upset, mostly lower doses , often hours after dose, also itchy throat common • Often requires cutting back on dose and desensitizing using very low dose to start • Several have had to discontinue due to persistent symptoms (5 patients) • Systemic reactions on home maintenance have occurred- uncommon but unexplained, possibly concurrent illness Effects of Food Allergies on Quality of Life • Food allergies have a significant impact on quality of life • Measures of general health, emotional impact and limitation on family activities • Impairment greater than children of similar age with a diagnosis of diabetes • Validated questionnaires have been developed and used as measures to assess the benefits of interventions Quality of life results: Parents perception of children • Less anxious about food, going to new places and to restaurants • Less concerned they will have a reaction • Less physical and emotional distress • Feel safer when going to vacation destinations • Less concerned about being left out Quality of Life: Children • Less frightened of eating wrong food by accident or eating something never tried • Less disappointed because of having a food allergy or when others don’t take seriously • Les concerned that they will never get rid of food allergy • Less troublesome over limitations in buying foods they like Quality of Life : Adolescents • Less concerned about reading labels, and refusing treats at school or work • Are able to eat more foods and spontaneously accept an invitation to go out for a meal with friends • Less frightened about eating the wrong food or having an allergic reaction (needing EpiPen) Who are candidates for desensitization? • History of peanut allergic reaction and elevated serum IgE to peanut and/or large skin test result • Even if not ‘very concerned’ now, measures of QoL tell another story • Pre-adolescents and high school students • Anyone with as peanut allergy because we have shown safety and efficacy (if only for piece of mind) Allergen Specific OIT: Milk • Cow’s milk allergy most common and affects 23% of population • Majority outgrow allergy by age 3 years, but more have persistent allergy and tolerance in teens • High levels of specific IgE to milk associated with a lower likelihood of out-growing allergy • OIT has been effective for milk, but adverse events are common 35-60% , some severe • Severity of reactions greatest on initial days and least when high doses reached (risk of EoE) Allergen Specific OIT: Egg • Resolution of allergy, takes longer-4% by 4 yrs, 37% by 10 yrs, 68% by 16 years • Children with serum IgE >50, unlikely to develop tolerance • OIT to egg was shown to be successful in a small number of patients with a history of allergy • Adverse effects-common Peanut Oral Immunotherapy Generally Safe but not w/o Risk • Should be performed in a facility designed primarily for these procedures • Trained staff (one to one) with keen knowledge of food allergies and management of reactions • Equipment, emergency medications and procedures in place • Utilize experience of others to assist in developing similar and safer protocols Unanswered Questions • • • • • What is the optimal dose of PN immunotherapy ? What is the ideal duration of treatment? How to determine degree of protection provided? Factors leading to inducing tolerance (cure)? Efficacy for different ages, severity and type of food allergy? • Why are GI symptoms common and how can we prevent them? Is oral immunotherapy a treatment option that will eventually become a standard of care? • Yes, but more experience necessary to understand causes of adverse reactions • Clear benefit in psychosocial impact due to food allergy on patients and families • Patients are very motivated to come in for visits and maintain daily treatment • Potential for tolerance induction (cure) in some What the experts think… • “When performed by experienced investigators in an appropriate setting, peanut OIT is a safe, allergen-specific therapy effective in inducing desensitization and providing protection against accidental ingestion with ongoing therapy” Varshay P.,Jones SM, Scurlock AM, et al. J Allergy Clin Immunol 2011;127:654-60 Getting more information • Speak to parents/patients who are going thru the process at this time (we can help facilitate) • Call NEFATC-talk to staff and physicians about the treatment(860) 986-6099 • See website: www.nefoodallergy.org and Facebook • Visit our Center: 836 Farmington Avenue, Suite 138, West Hartford, CT • Review the literature Food Allergies in Schools • Food reactions are not rare in schools/day cares • 16% of children with a food allergy will experience an allergic reaction • Almost 25% of Peanut/nut allergic reactions occurred in school/day care before a diagnosis made • A survey of anaphylaxis in school showed epinephrine was necessary in many children without any prior experience of food allergy Contact reactions from peanut: an issue? • Soap and water removes peanut protein from hands and surfaces • Hand sanitizers/dishwashing liquid alone do not • Peanut protein relatively easy to clean with conventional cleaning methods • Contact exposure can be prevented and typically not a significant risk at schools Myths: Inhalant and contact exposure • Allergic reactions to foods are immunologic responses to protein allergens • Odors are neurologic responses triggered by organic compounds • Study: 30 children w/ severe peanut allergy had an inhalation challenge for 15 minutes • None had an reactions • Also, after applying peanut butter to the skin for 10 minutes -occasional local redness, there were no systemic reactions Should peanuts be banned in schools? • No controlled studies have been done on subject so subject to individual judgment • Milk resulted in more allergic reactions per capita than peanut or other nuts • Peanut-free tables, isolate, ostracize, create more anxiety and do not mimic the real world • 79% of food reactions occurred in classroom, only 12% occurred in cafeteria • Classroom projects with peanut butter a concern • PN protein not found in the school air even when peanut butter was consumed in the Problems exist in recognition and management at schools • Deficiencies exist nationally in protocols for managing food anaphylaxis • Emergency Action Plans (EAPs) in place only 33% of cases • During a reaction, plans when present, were frequently not followed • In a survey of parents/school personnel, of the students who had food anaphylaxis 14% had no physician orders Recognizing/treating reactions • According to national peanut/tree nut registry, gaps in care exist in recognizing and treating anaphylaxis in schools • In 32% cases of food anaphylaxis in schools , symptoms of an allergic reaction were not recognized • Where trained personnel know what to do, there often were no trained back-up staff • Only 26% with a history of an allergic reaction to a food had epinephrine available Management in Schools • Everyone makes mistakes • Accidents are never planned • All children must have a food allergy treatment form or EAP which reviews symptoms and treatment of anaphylaxis • Review your emergency action plans regularly • Educate others on what to do in case you need their help or are not available Referral for Food Allergy Evaluation • • • • • • History of severe reactions to any food Atopic dermatitis that may be food related Allergy to peanut, tree nuts, fish, shellfish Unexplained episode(s) of anaphylaxis Clarifying status of food allergic patient The patient with multiple food allergies for nutritional guidance • Intervention: Oral immunotherapy Conclusions • Prevalence of food allergy has increased in recent years for peanut and other foods • More severe reactions/anaphylaxis observed • Recognizing risks at schools: separating fact from fiction • Understanding anaphylaxis and optimal treatment can be improved • Oral immunotherapy is an effective treatment for peanut and other food allergies and substantially improves quality of life References • • • • • • • • • Lack, G. NEJM 2008;359:1252-60. Sicherer, SH, Burks, AW, JACI 2008;122 Lemon-Mule, H, et.al., JACI 2008;122:977-83 Sicherer, SH, Burks, AW, JACI, (in press) Burks, AW, AAAAI Mtg 2009 (Lecture) Longo, G, et.al., JACI 2008;121:343-7 Clark A., Annals of Allergy (in press) Jones, SM, AAAAI Mtg. 2009 (Lecture) Keet CA, and Woods, RA, Immun Aller. Clin. Of NA, /2007:27 (2) • Du Toit, et. al., JACI 2008;122:984-91 • Lack, G. JACI 2008;121. • Sampson, HA, AAAAI Mtg 2009 (Lecture)