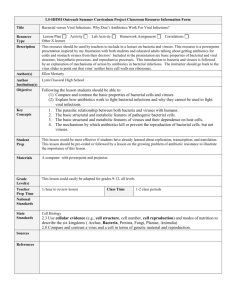
Magic Bullets LO's - PBL-J-2015
advertisement

Week 5 Magic Bullets Magic Bullets LO’s Mechanisms of antibacterial resistance Anatomy of the lower limb muscles Applied anatomy of muscles Pathogenesis of bacterial infections Infection and Host defence Respiratory Viruses Antibiotic and antibacterial agents Connective Tissues Antibiotic resistance Consent and Informed decision making Hypotheses of Disease causation Measuring Disease Frequency and association Communication Skills Week 5 Magic Bullets Methods of Antimicrobial Resistance Selection of Abx Treatment: Clinical Indication of Abx treatment: Bacteria vs. Virus Pathogen identification - microbiological diagnosis Empirical Treatment - based on the MOST LIKELY pathogen (before lab results are available) ? In vitro sensitivity/resistance of pathogen to Abx Site of infection Pharmacodynamics, pharmacokinetics, toxicity Host factors: compromised hepatic/renal function Availability and cost Likelihood of induced resistance Antibiotic Mechanisms: Summary Mechanism Abx Group Primary Effect Inhibition of Cell Wall Synthesis Penicillins Cephalosporins Vancomycin Bactericidal Bactericidal Bactericidal Inhibition of Protein Synthesis Aminoglycosides Tetracyclines Macrolides Chloramphenicol Bactericidal Bacteriostatic Bacteriostatic Bacteriostatic Inhibition of Nucleic Acid Synthesis Quionolones Fluroquinolones Rifampin Bactericidal Bactericidal Bactericidal Inhibition of Metabolism Sulphonamides Trimethoprim Isoniazid Bacteriostatic Bacteriostatic Bactericidal Cell Membrane Disruption Polymixin B Bactericidal Reasons for treatment failure: 1. Poor compliance 2. Poor absorption or penetration 3. Drug interaction 4. Microbial resistance 1. Identify, with examples, the mechanisms by which micro-organisms resist the action of antibiotics Forms of resistance: Intrinsic: predictable in genus/species - less of problem Acquired: unpredictable - mutliple - big problem Acquired Resistance: Gene encoding resistance o Mutations - e.g. chromosomal mutations o Evolved in response to environment: spontaneous transfer and spread of mutations Spreading of Resistance: Plasmids - exchanged/transferred/incorporated into other cells. Plasmids do not have to be incorporated/transformed into the chromosomal DNA in order to confer resistance, they may do specific things on their own which make the bacterium resistant. Conjugation: Week 5 Magic Bullets 'Bacteria Sex' - cell to cell contact and exchange of genetic material. How? Conjugative plasmids code for the production of surface tubules (?Fimbriae?) which connect two cells together: these conjugative plasmids pass quickly from one cell to another o Can occur in G+ or G- cells o Main mechanism for spreading of resistance. Tranduction o via bacteriophage - plasmid DNA is enclosed in virus/phage o plasmid DNA transferred to other bacterium of the same species as the virus 'infects' all the other cells o (?in vivo evidence?) Transformation: o Free/Naked DNA taken up from environment and incorporated into chromosomal DNA of bacterium via crossing over mechanisms o (?in vivo evidence?) Transposable elements: insertion sequences flanking genes - allows DNA movement. Can occur in 'cassettes' of resistance genes (multiple resistance genes). Comes from transposons Mechanisms of Resistance: 1. Exclusion of antibiotic from target binding site o Reduced/No entry into cell o Often intrinsic e.g. Penicillin/Gram Neg. - Penicllins are inaffective against gram neg. as G- do not have significant cell wall to synthesis e.g. aminoglycosides and streptococci 2. Antibiotic inactivation o Enzymes cleave/modify drug o Intrinsic OR acquired: e.g. B-Lactamases 3. Drug target alteration: o Alteration of penicillin binding position (PBP) on penicillin antibiotics 4. Antibiotic removal o Efflux pumps: removed Abx from cytoplasm 5. Drug Action Bypass o Use of alternate metabolic pathways o Important in Sulfonamides, Trimethoprim, Isoniazids (affect metabolic pathways) o o 2. Give examples of mechanisms of bacterial resistance to antibiotics Acquired Antibiotic Resistance occurs as a result of genes that encode for resistance: see above for information on how this can occur. Beta-Lactams Resistance: Beta Lactams enter bacteria to inhibit cell wall synthesis Intrinsic Resistance: cannot bind G- bacteria due to change in membrane charge Acquired Resistance: o Antibiotic Inactivation: B-Lactamase enzymes produce which inactivate the B-Lactam ring structure Bata-lactamases are produced by most bacteria Cell bound (G-) or external (G+) Encoded on plasmids, transposons or chromosome Inducible or constitutive Various forms: Week 5 Magic Bullets Penicillinases TEM1 and SHV1 types ESBL mutant types Amp C cephalosporinases Drug Target Alterations: o Penicillin Binding Protein alterations (found in S. Pneumoniae) Prevents penicillins binding to the bacteria o Outer Membrane Protein (OMP) changes: Prevents B-Lactam entry into cell Conferred to most G- Bacteria Requirement to add ESBL inhibitor such as clavuronic acid (inhibits beta lactamases) HOWEVER: this is not useful in vivo Glycopeptide Resistance Normally Glycopeptides bind to peptidoglycan precursors to inhibit cell wall synthesis Intrinsic Resistance: impermeability of glycopeptides across the outer membrane of Gbacteria Acquired Resistance: Transposon mediated Drug Target Alteration o Acquired Resistance: Replacement of DNA sequences from transposon encoded sequences: proteins produced no longer bind glycopeptides Aminoglycoside Resistance Aminoglycosides inhibit bacterial protein synthesis initiation Acquired Resistance: Drug target Alteration o Impaired transport o Reduced binding at ribosome target site Antibiotic Inactivation: o Production of drug modifying enzymes: most important plasmid borne phosphorylating enzymes adenylating enzymes Week 5 Magic Bullets acetylating enzymes Tetracycline Resistance Tetracyclines inhibit protein synthesis. Resistance is relatively common. Uses: U/L RTIs, minor sepsis, GIT, skin infections, and specific pathogens e.g. Chlamydia, Mycoplasma Acquired Resistance: Active Drug Efflux: Energy dependent pumping of drug from cell - reduces levels and ribosome inhibition Mechanism: o Plasmid borne genes Macrolide Resistance: Macrolides inhibit protein synthesis by binding the ribosome. Intrinsic Resistance: low permeability Outer Membrane Acquired Resistance: Plasmid borne Drug target alteration: o Blocks binding of the drug by methylating adenine bases in rRNA so that the drug cannot bind o Gives cross resistance to all macrolides o Especially important in S. Aureus Quinolone Resistance: Quinolones bind to DNA gyrase (G-) and topoisomerase IV (G+) to disrupt DNA function & kill the cell Acquired Resistance: Drug target alteration: o Mutations in gyrases Active Drug Efflux: o Decreased intracellular accumulation Sulfonamide and Trimethoprim Resistance Sulphonamides and trimethoprim inhibit folate synthesis which inhibits nucleotide synthesis and inhibit metabolic pathway enzymes/substrates. Acquired Resistance: plasmid mediated Drug target alterations: o Altered metabolic p/ways in bacterium 3. Identify and briefly describe culture techniques for pathogens and the method of assessing antibiotic resistance in vitro. Determining: minimum bactericidal concentration minimum inhibitory concentration achievable dosage in vivo (pharmokinetic studies) determine breakpoints: maximum achievable safe concentration in vivo vs. amount needed to overcome bacteria Week 5 Magic Bullets calibrate methods to distinguish sensitivity/resistance 1. Broth Dilution: o MIC o MBC o Series of broths with bacterium and differing conc. of Abx prepared o MIC is lowest concentration that prevents growth of bacteria o MBC is determined by agar subculture growth of broths that showed no growths 2. Agar Diffusion: o As for broth dilution, using agar plates 3. Disc Diffusion: o Qualitative measure of Abx sensitivity: all give measures of the MIC CDS: Bacteria is mixed with sterile saline and washed around agar plate Plate is dried (bacteria should be distributed all over the plate) Series of Abx discs stamped onto the agar plate No growth: sensitive Growth: resistant E-test strip: diffusion from strip which contains a spectrum of Abx concetrations MIC is taken from elliptical zone of growth intersecting strip NCCLS: ? 4. Specific Resistance Testing Muscular System & Muscles ~ Lower Limb Week 5 Magic Bullets BE ABLE TO IDENTIFY THE MAJOR MUSCLE IN THE LOWER LIMB Muscles in the lower limb are grouped in 3 areas: 1. Muscles of the hip 2. Muscles of the thigh 3. Muscles of the leg MUSCLES OF THE HIP Muscles that attach to the hip Iliacus & Psoas MUSCLES OF THE GLUTEAL REGION Muscles of the gluteal region are grouped into superficial and deep layers The superficial layer comprises: Gluteus Maximus Gluteus Minimus Gluteus Medius The deep layer comprises: Piriformis Obturator internus MUSCLES OF THE THIGH Muscles of the thigh are grouped into anterior, medial and posterior muscle groups The Anterior compartment comprises: Vastus muscles (vastus lateralis and vastus medialis) Quadriceps Rectus femoris femoris Sartorius (can be considered to be in hip or thigh) The Medial compartment comprises: Adductor longus Adductor magnus Gracilis Obturator externus Tensor Facia lata The Posterior compartment comprises: Biceps femoris Semimembranosus Semitendinosus MUSCLES OF THE LEG Muscles of the leg are grouped into anterior, lateral and posterior (superficial and deep if you wish to be detailed!) compartments The Anterior compartment comprises: Tibialis anterior Extensor hallucis longus Extensor digitorum longus Peroneous tertius The Lateral compartment comprises: Fibularis brevis Week 5 Magic Bullets Fibularis longus The Posterior compartment comprises: Flexor digitorum longus Tibialis posterior Flexor hallucis longus Gastrocnemius Soleus Popliteus Tendocalcaneous Peroneus longus (at back of foot) Week 5 Magic Bullets ANTERIOR COMPARTMENT LEG MUSCLES: TIBIALIS ANTERIOR EXTENSOR DIGITORUM LONGUS EXTENSOR HALLUCIS LONGUS FIBULARIS (PERONEUS) TERTIUS POSTERIOR COMPARTMENT LEG MUSCLES: GASTROCNEMIUS SOLEUS PLANTARIS FLEXOR HALLUCIS LONGUS FLEXOR DIGITORUM LONGUS TIBIALIS POSTERIOR LATERAL COMPARTMENT LEG MUSCLES: FIBULARIS LONGUS FIBULARIS BREVIS COMPREHEND THE ORGANISATION OF MUSCLE WITHIN DIFFERENT COMPARTMENTS OF THE LOWER LIMB, THEIR NERVE SUPPLY AND ACTIONS Gluteus Maximus Nerve Supply Inferior Gluteal nerve Gluteus Minimus/Medius Superior Gluteal nerve Artery Supply* Inferior Gluteal artery Superior Gluteal artery Piriformis Branches of S1 and S2 Internal pudendal artery Thigh – Anterior (Thigh – Sartorius) Thigh – Medial Thigh - Posterior Femoral Nerve Deep profundus Obturator Nerve Sciatic nerve (except for the short head of the biceps femoris that is supplies by the common fibula nerve) Deep fibular nerve Superficial fibular nerve Tibial nerve Obturator Artery Perforating artery Adduction of thigh Knee flexion Tibial artery Fibular artery Extends ankle Everts foot Leg – Anterior Leg – Lateral Leg - Posterior Action Extends thigh Lateral rotation Abduct and medially rotate thigh Laterally rotate extended thigh, abduct thigh Knee extension (+ hip flexion) Posterior Tibial Flexes ankle artery * I think that these artery supplies are correct, however please let me know if you find errors with them and I will update the table Week 5 Magic Bullets Anatomy: Applied anatomy of the muscles. Upper/lower limb 1. Understand, demonstrate and discuss the muscles related to the shoulder, elbow, wrist joints and the back. Just repeating lecture notes here probably not useful. Everyone just needs to plough through these to try to learn it. Similarly, summarising anatomy as it has been presented is not particularly achievable or useful. There are a heap of tables etc that summarise site, action, attachments, nerve supply etc in neat fashion in virtually every textbook. Tried a functional/clinical approach instead. It may not mean much for exams but might be handy for you to come back to at some stage. Haven’t listed every muscle or even every group. Just the ones that link to certain conditions you will see time and time again in clinical practice. This is not meant to be a complete list of issues or disorders. Sometimes reading about a common condition can help reinforce the picture of the anatomical structure and its function and help you remember it. Shoulder Muscles: Scapular stabilising muscles: Rhomboids, trapezius, serratus anterior, pec minor (with the exception of pec minor I think this is what the objectives mean by “back muscles”). Function: As a group - to control, anchor the scapula to the chest wall. The shoulder is only attached to the skeleton via one joint, the sternoclavicular joint. Thus, the shoulder relies heavily on the muscles securing the scapula (shoulder blade) to the thorax, to give it a stable base upon which to move. The scapula presents a very shallow “socket” ( the glenoid ) to the head of humerus. This is, by design, a very mobile joint to allow us to position our hand in all sorts of weird and wonderful positions. Clinical Relevance: The cost for the mobility described above is relative instability of the “passive system” (bony configuration, ligaments, capsule). Disuse of scapula stabilisers due to direct/ indirect injury or neuromuscular disorders may result in wasting or disturbed patterns of recruitment of these muscles. Rehabilitation aims to restore strength and bulk to these muscles, but also to retrain patients in restoring normal control or coordination of these muscles. Again - this is to provide a solid, well controlled platform from which the shoulder can “do its thing”. NB: Strength and control are two different things. One is about developing the force/power abilities of the muscle – the other is about retraining neuromuscular patterns of recruitment. Understanding these recruitment patterns is becoming more and more relevant in terms of understanding why injuries occur and how we can prevent them happening in a rehabilitative sense. Week 5 Magic Bullets Shoulder Stabilisers Deep Layer: Rotator Cuff: Anterior : Posterior: Supraspinatus Infraspinatus Teres Minor Function: Subscapularis NB: Deep muscles are best positioned to confer stability to joints. They attach close to the centre of rotation so aren’t designed as prime movers. Along with the ligaments, they are designed to limit (but allow) glides or translations within the joints and approximate the surfaces throughout range as the more shallow/superficial prime movers and their assistants produce the actual movement available at the particular joint. You can divide most of the muscles acting over the major articulations of the body into deep and shallow muscles to consider their function similarly. Exceptions are probably the joints in the feet or hands. The cuff pretty much keeps the humeral head approximated in the centre of the glenoid whilst the more superficial deltoid, bicep, tricep, coracobrachialis, pec major, lat dorsi, teres major produce the movements. Contraction of the discrete parts of the cuff will cause movement ( see “action” of these muscles). So in part, they are thought of as assisting or helping to initiate movement. Their main function, however, is to control movement and confer stability to an otherwise relatively unstable joint. Clinical Relevance The cuff, or it’s parts, can be injured acutely in collision incidents, falls, or during dynamic overhead activities in the home, work or sporting environment. Dislocations or partial dislocations (subluxations) will often occur in these incidents and underlying damage can occur to joint structures. At presentation, pain and disability can be quite considerable. Loss of joint integrity = relative instability = ↑demands on an already damaged cuff, = poor cuff function = relative instability ↑ = ↑cuff demands *A vicious cycle You will probably see relatively more chronic injuries when it comes to the rotator cuff. These can occur when this vicious cycle is allowed to continue after acute, traumatic incidents. Alternatively, overuse of the cuff in any setting – but particularly at work or in the sporting environment with overhead patterns of use. “Overuse” is a relative term. Any significant change in loading (volume and /or intensity) may induce changes within the cuff “quality”. These changes usually take the form of a degeneration (rather than inflammation) of the cuff tendons as they approach the humeral head. We will see this described as Week 5 Magic Bullets tendinopathy. It is now thought that compressive load upon these tendons is what induces degenerative change – deformation of collagen and proliferation of ground substance. Think of this as less bricks and more mortar within the tendon tissue. The tenocytes (cells) within the tissue have a maintenance/repair function. So the “maintenance man/person” is run off his/her feet trying to repair damaged tissue – gets more and more ineffective and eventually “leaves the building” People with chronic rotator cuff dysfunction will have less pain compared to the acute setting. They attend with nagging pain, more intense with elevation primarily. They can limit/avoid pain by avoiding such positions. So they attend more due to dysfunction. Bicep At shoulder (also acts over elbow), assists in flexion and also in adduction when shoulder elevated ie across body (sometimes called horizontal flexion). Clinical Relevance: Degenerative changes to tendon of long head in later life. Picture its course in bicipital groove where it takes a turn over top of humerus to its attachment on glenoid. Easy to see why it might be under load ++. Also acute or chronic injuries related to dynamic overhead activities – particularly throwing sports. Ruptures are common in older age due to such degeneration and poor tissue nutrient supply. Patients will present with pain (if acute) and a “popeye deformity” in cases of rupture of this tendon. Rehab includes rehab of proximal musculature – scapula stabilisers and cuff. Repair is rarely preformed.as the muscle can function well (despite some loss of power) using the existing anchor point of the short head to the coracoid process. Elbow / Wrist: There are rarely problems with the muscles acting over the elbow. Acute ruptures of the distal attachment of biceps can occur in a traumatic “wrestling” type incident or with a “catching” event with a suddenly changing or shifting load. Degenerative changes would predispose one to such an incident. However tendon attachments at the elbow can be problematic. Medial and lateral elbow pain often stems from: tendinopathy of the wrist extensors attaching at or about the lateral epicondyle of the humerus (lateral epicondylitis – “tennis elbow”). tendinopathy of the wrist flexors attaching at or about the medial epicondyle of the humerus (medial epicondylitis – “golfers’ elbow”). Rehab (in this case and with tendinopathy in general) involves manipulating load (many variables to consider) upon these structures to firstly allow them to recover/repair (reduce load) and then to condition them to cope with future loading (increase load in progressive step-wise fashion). Hand / Fingers: Week 5 Magic Bullets Muscular function at the wrist and hand is very detailed and complex. Ligament and bony injuries are quite common in relative terms. In terms of musculo – tendinous function, injuries to the finger joints are probably the most significant. Damage to these joints can cause specific loss of function and often deformities due to a resting imbalance of forces across joints – see “mallet finger”, “boutonniere (button hole) deformity” and “swan neck deformity” as examples. “Carpal Tunnel Syndrome” can cause widespread muscular dysfunction (thenar muscles - - opponens pollicis, abductor pollicis brevis, flexor pollicus brevis, and the lateral lumbricals due to compression of the median nerve as it passes through a narrow channel in the wrist. The median nerve shares this channel with several tendons. Changes in bony, tendon, or neural tissue can cause degenerative and or inflammatory changes within this confined space and thus compressive neuropathy. 2. Understand, demonstrate and discuss the muscles related to the hip, knee and ankle joints. Hip: The hip is a relatively stable joint in terms of bony configuration, ligaments and capsular attachments. Tears and muscle strains about the gluteal area are uncommon. Like the shoulder, the tendons of the muscular network about the hip are subject to tendinopathy as they approach their distal attachments after crossing the joint. Treatment for lateral and posterior hip pain has often focused on bursitis about the greater trochanter, ischeal tuberosity and deep to gluteus medius. It is now thought this issue of tendinopathy plays a more significant role than previously thought. Control of movement at the hip has implications for function and loading not only at the hip joint itself, but also for the structures proximal (sacroiliac joints, lower spinal joints and tissues) and distal (knees ,ankles and associated musculature) to the hip. Lectures have emphasised the stabilising role of the ilio tibial tract and its muscular attachments, gluteus maximus and tensor fascia lata. Along with other deep (stabilising) muscles in the hip, strength and control work is often employed when treating people with low back pain for example and also knee pain. If hip control is poor, repetitive movement patterns in a sporting or occupational sense will cause excessive load on these distal and proximal structures (not to mention the hip itself). Knee: When we consider the forces operating about the knee (tibio-femoral and patellofemoral joints), the way in which the muscular system controls movement and loading here really is quite extraordinary. Pain about the patello-femoral joint is one of the more common knee presentations, particularly in active, growing adolescents. Consider all the muscles crossing the knee and how they contribute to stress upon the patellafemoral joint. Simplify this to just the medial and lateral forces acting upon the patella as it tracks up and down upon the femur as the knee flexes and extends during walking, running, squatting, jumping etc. The iliotibial tract and hence gluteus maximus and tensor facia lata will tend to hold the patella laterally. The vastus medialis and vastus lateralis will exert forces upon the patella as their name suggests. The hamstring and adductor muscles will have an impact Week 5 Magic Bullets on the angulation of the knee relative to the hip and foot and thus the relative alignment of the patella with respect to the femur. Acute injuries or chronic conditions about the knee can change the way in which these muscles function where they might become weak or tight for example. The coordinated actions of the muscles as a group in terms of timing and speed of contraction will have consequences for patella-femoral function and stress upon its weight bearing surfaces. Thinking about the attachments and actions of the muscles, and trying to picture what happens to the joints that they relate to can be useful. Going beyond that and reading about injuries or conditions that you, your friends or family experience will help cement the anatomy involved with those injuries in your memory. When you get some spare time! Week 5 Magic Bullets PATHOGENESIS OF BACTERIAL INFECTIONS 1. Identify the key differences between prokaryotic and eukaryotic organisms Eukaryotes Algae, protozoa, fungi, plants and animals >5μm Diploid genome, nuclear membrane Ribosome 80S (60S + 40S) Cytoplasmic organelles: mitochondria, golgi body, ER Cytoplasmic membrane: sterols Cell wall absent/chitin Sexual/asexual reproduction Respiration via mitochondria Prokaryotes Bacteria <5μm Haploid, circular double-stranded DNA Ribosome 70S (50S + 30S) NA Cytoplasmic membrane: no sterols Cell wall: peptidoglycan, proteins & lipids (complex) Asexual reproduction (binary fission) Respiration at cytoplasmic membrane 2. List different categories of infectious agents and outline their differences. Viruses: Obligate intracellular parasites that lack compliment enzymes necessary for their replication and therefore rely on their host cells’ metabolic machinery for replication. Viruses consist of a nucleic acid genome surrounded by a protein coat (capsid) that is sometimes encased in a lipid membrane. Viruses may contain a nucleic acid genome of DNA or RNA, but not both. For human purposes they are divided into two main groups, the RNA viruses and the DNA viruses. Bacteria: Bacteria are prokaryotes, meaning they have a cell membrane but lack membrane-bound nuclei and other membrane-enclosed organelles. Most bacteria are bound by a peptidoglycan cell wall (a polymer of long sugar chains linked by peptide bridges). There are two forms of cell wall structures, a thick wall that retains crystalviolet stain (gram-positive bacteria) or a think wall sandwiched between two phospholipid bilayer membranes (gram-negative bacteria). Bacteria are classified by their gram stain (positive or negative), shape (spherical ones and cocci; rod-shaped ones and bacilli) and need for oxygen (aerobic or anaerobic). Many bacteria have flagella that enable movement and some possess pili, another kind of surface projection that can attach bacteria to hots cells. Most bacteria synthesize their own DNA, RNA and proteins, but they depend on their host for favourable growth conditions. Other infectious agents include prions, fungi, protozoa and helminths. The table below gives examples. Taxonomic Size Site of propagation Examples Disease Prions 30-50kD Intracellular Prion protein Creutzfeld-Jacob disease Viruses 20-300nm Obligate intracellular Poliovirus Poliomyelitis Bacteria 0.2-15 μm Fungi 2-200 μm Protozoa 1-50μm Helminths 3mm-10m Obligate intracellular Extracellular Facultative intracellular Extracellular Facultative intracellular Extracellular Facultative intracellular Obligate intracellular Extracellular Chlamydia trachomatis Streptococcus pneumonia Mycobacterium tuberculosis Candida albicans Histoplasma capsulatum Trypanosoma gambiense Trypansoma cruzi Leishmania donovani Wucherria bancrofti Trachoma, urethritis Pneumonia Tuberculosis Thrush Histoplasmosis Sleeping sickness Chagas disease Kala-azar Filariasis Week 5 Magic Bullets Intracellular Trichinella spiralis Trichinosis 3. Describe the structure and characteristics of bacteria. Nuceloid: site of double stranded circular DNA. In the cell it is condensed and looped into a coiled state. Essentially haploid organisms with only one allele of each gene per cell. Nucleoid lies within the cytoplasm. Ribosomes: Slightly smaller than those of eukaryote cells. Ribosomes are microscopic ‘factories’ found in all cells including bacteria. They are responsible for protein synthesis. Bacterial ribosomes are never bound to other organelles as they sometimes are (bound to the ER) in eukaryotes, but are freestanding structures distributed throughout the cytoplasm. The differences between bacterial ribosomes and eukaryotic ribosomes mean that some antibiotics will inhibit the functioning of bacterial ribosomes, but not a eukaryote's, thus killing bacteria but not the eukaryotic organism they are effecting. Cell wall: Supports the weak cytoplasmic membrane against the high osmotic pressures (survival). The chemical composition differs considerably between the different bacteria species but the main component is peptidoglycan. The thickness of this peptidoglycan layer is what is used to distinguish between the thick gram positive (20-80nm) and the thinner gram negative cell walls (5-10nm). Cell membrane: is a phospholipid bilayer allowing selective permeability. A key feature differentiating prokaryotic cytoplasmic membranes to eukaryotic cell membranes is their multifunctional nature. Protein secretion, packaging and processing, electron transport and oxidative phosphorylation, all must be performed by the cytoplasmic membranes in prokaryotes (unlike eukaryotic cells). The membrane is therefore extremely protein rich allowing very little space for phospholipids. Capsule: some species of bacteria have a third protective covering. This capsule is made up of polysaccharides (complex carbohydrates). The capsule keeps the bacteria from drying out and protects from phagocytosis. The capsule is a major virulence factor in the major disease-causing bacteria, such as E. coli and s. pneumoniae. Non-encapsulated mutants of these organisms are avirulent, i.e. they don't cause disease. Slime layers: Like the capsule, the slime layer protects the bacteria from environmental damages such as antibiotics. The slime layer also allows bacteria adherence. Periplasmic space: Site of nutrient processing. This is a very active region, between plasma and cell wall and is only present in gram-negative bacteria. Week 5 Magic Bullets Inclusion bodies: Are nuclear or cytoplasmic aggregates of sustainable substances, usually proteins. Vacuole: gas vacuoles allow for buoyancy in aquatic environments. Flagella: Motile bacteria possess filamentous appendages known as flagella, allowing locomotion. They are 2-3 times the length of the bacterial cell. The flagella rotates and pulls bacteria forward. Pili (fimbriae): Filamentous appendages much more numerous than flagella and much shorter in length. They are important in securing adhesion between the bacteria and host cell, although they are not the only way bacteria adhere to host cells. Involved in bacterial mating and DNA transfer. Endospores: survival in hostile environment; very resilient, can exist in dormant state for long periods and germinate later. CHARACTERISTICS a) Metabolism Growth phases: lag phase, exponential growth phase, stationary phase (nutrient deficit), death phase. Reproduction (binary Fission): uncoiling of DNA, replication of DNA, cell elongation, septum formation and separation. Results in two daughter cells, identical to each other and parent cell. b) Temperature and Growth Hyperthermophiles: 65-105° Thermophiles: 40-80° Mesophiles: 15-45° (grow at body temperature, almost all human pathogens) Psychrotrophs: 2-35° (food microorganisms that can survive in fridge- food spoilage) Psychrophiles: 5-18° c) Sources of carbon, energy and hydrogen/electrons Carbon sources Autotrophs: CO2 sole or principle C source. Heterotrophs: reduced, preformed organics (sugars, amino acids). Energy Sources Phototrophs: light Chemotrophs: oxidation of organic/inorganic compounds Hydrogen or Electron Sources Lithotrophs: reduced inorganic molecules Organotrophs: organic molecules d) Antigens: Initial division on basis of haemolysis on blood agar. α-haemolysis: 1-3mm greenish zone of incomplete haemolysis. β-haemolysis: zone of clearing/complete lysis without a market colour change. γ: no haemolysis. e) Genetic characteristics: Ribosomal RNA: 16S (most eukaryote size is 18S) found in all bacteria. Genes: some common to all bacteria, others pathogen specific. Week 5 Magic Bullets Molecular diagnostics permits detection and identification without culture (quicker, can be used even if pathogen can’t be grown, can use very small amounts). Information encoded in: chromosomes, plasmids and transpoons. -Constitutive genes: expressed all the time -Inducible genes: expressed when needed. Regulation of gene expression ensures adaptation to environment and avoidance of overproduction/waste. Genetic diversity achieved by: mutation, recombination, gene transfer/exchange (important in virulence (degree of pathogenicity) and antimicrobial resistance). Mutations: Spontaneous or external physical chemical factors. Involve point mutations (single nucleotide change), deletions or insertions. Consequences may be lethal, phenotypic change, no change, selective advantage, repair, spontaneous loss over Subsequent replication cycles. Recombination: Process by which new genetic material is inserted into the genome via conjugation (direct cell to cell contact mediated by fertility plasmids), transformation (naked DNA from environment) or transduction (from a bacteriophage). Plasmids: Small circular DNA molecules that are not part of the bacterium’s chromosome. They have their own replication origins. Transpoons: Segments of DNA that can move about chromosome within single organism or between different organisms. Differ from plasmids in that they are unable to reproduce independently. 4. Identify, and discuss the functions of, the structural components of bacteria which are involved in the pathogenesis of infection. Adhesions: specialized structures on the cell surface of bacterium that bind to complementary receptor sites on host cell surfaces. Allow adherence with high specificity for certain tissues. Two types of adhesion: cell recognition by the bacterial fimbriae and non-fimbrial adhesions regulated primarily by a large range of surface proteins. Capsule: well organised polysaccharide layer outside cell wall. Many bacterial pathogens require a capsule to avoid phagocytosis and production of an extracellular capsule is the most common mechanism by which this is achieved. Resist phagocytosis by reducing interactions with complement and specific antibodies. Glycocalyx: network of polysaccharides extending from bacterial surface, aids in attachment to tissue. Week 5 Magic Bullets S-layer: structured protein/glycoprotein layer. Protects against ion and pH fluctuations, osmotic stress and enzymes. Helps maintain shape and rigidity and may promote cell adhesion to tissues. Once inside cell, bacteria are lysed and the bacteria are released into the cell cytoplasm, multiplying rapidly with inhibition of the host cell protein synthesis. 5. Describe the various mechanisms by which bacteria and viruses cause disease. Whether it is viral or bacterial, for a disease process to be harmful to humans some form of interaction between the infecting agent and the cell must occur. Week 5 Magic Bullets BACTERIA 1. Bacteria maintain a reservoir (before and after infection). 2. Transport of pathogen to host: direct contact (coughing, sneezing, body contact); indirect contact (via soil, water and food). 3. Attachment and colonisation by pathogen- establishment of site of reproduction. Depends on ability to compete with host for nutrition. 4. Invasion of pathogen: entry into host cells and tissue -Production of lytic substances, alter host tissue by attacking ground substance, basement membranes, degrading carbohydrate-protein complexes between cells or on cell surface; disrupting cell surface. -Passive entry: breaks, lesions in mucous membranes, wounds, burns. -Once under mucous membrane, pathogen can penetrate deeper tissues and spread. 5. Growth and multiplication: must find appropriate environment (pH, temp, nutrients) will depend on body site. 6. Leaving the host: most employ passive mechanisms of escape (faeces, urine, saliva). VIRUSES 1. Entry: via body surfaces (skin, respiratory, GIS, urogenital, conjunctiva) Other (needle stick, blood transfusion, insect vector). 2. Replication: at site of entry or spread then replicate. 3. Viral spread: commonly bloodstream and lymphatics. Sometimes via nerves. 4. Tropisms: specificities for cell, tissue or organ. 5. Cell injury and clinical illness: -Destruction of virus: infected cells in target tissue and alterations in host physiology are responsible for disease. -Lytic infections: virus multiplies and kills host cells immediately; new virions released. -Persistent infections; virus lives in host cells and releases virions over a long period with little damage to host cell. -Latent infections: virus resides in cell but produces no virions; activated later and lytic infection occurs. -Virus transforms cell into a cancer cell (eg HPV). 6. Host immune response. 7. Recovery- host will either succumb to virus or recover. 8. Virus shedding- shedding of virus back into environment; stage where host is infectious and can spread the virus. Week 5 Magic Bullets Infection and host defense 1. Identify the function of epithelial barriers and the innate non-specific defences in the prevention of infection Infection Control: External Defenses: Epithelium o Skin + Mucous Membranes o Physical, chemical and biological barrier to the entry of microorganisms o E.g. skin - shedding of corneal layer of epidermis with abrasion to rid microorganisms from the skin Secretions: o Mucous secretions: contact barrier, block CHO ligand receptor interactions o Sebaceous secretions: antibacterial, antifungal o Defensins: antibacterial peptides produced in GIT - control colonisation o Tears: antibacterial - contain lysozome o Stomach acid - lethal to most bacteria o Commensal organisms - compete against each other thus act as their own biological control mechanism Peristaltic movement (stagnate area encourages growth) Mucociliary escalator (removes bacteria captured in mucous) Vomiting and Diarhorrea - reduces adhesion to mucous membranes Urine flow Coughing Internal defenses: 'Innate Immunity' CELLULAR COMPONENTS OF INNATE IMMUNITY Phagocytic cells: o Phagocytosis: eating Week 5 Magic Bullets o o o o Produce antimicrobial reaction oxygen species Secrete inflammatory mediators Antigen presenting cells (to T cells) Types Monocyte/Macrophage:eaters Dendritic Cells: antigen presenters Neutrophils: NOT antigen presenters, eaters + killers ?Eosinophils? What happens inside the Phagocyte after Phagocytosis? How does cell killing result? Phagolysozome: membrane-enclosed organelle inside the phagocyte - where digestion of phagocytosed material occurs Oxygen independent killing Effector Molecule Function Cationic proteins (cathepsin) Damage to microbial membranes Lysozome Hydrolyses mucopeptides in the cell wall Lactoferrin Deprives pathogens of iron Hydrolytic enzymes (proteases) Digests killed organism Oxygen dependent killing: all methods of oxidising phagocytosed pathogen. Oxidised pathogen = dead pathogen Phagosome-oxidase fusion Generation of H2O2 Myeloperoxidase activity Peroxynitrite production Natural Killer Cells: o Phagocytes release interferons (cytokines) to activate the NK cells o NK cells cause programmed cell death in affected self-cells React to stress molecules from affected cells React to non self cells or tumour cells (do not produce normal self recognition molecules) o Recognises and responds to antibodies Eosinophils: o Anti-parasitic o Protection of mucousal surfaces: Involved in allergy Basophils: o ?Antigen presenting cell? o Protection of mucousal surfaces: involved in allergy Mast cells: o Protection of mucousal surfaces: involved in allergy HUMORAL COMPONENTS OF INNATE IMMUNITY Complement system: o Circulating proteins secreted by the liver, macrophages/monocytes OR epithelial cells which become 'activated' under specific circumstances o Activation: Mediated by Antibodies (Classical Pathway) Mediated by Antigens/Pathogen surface (Alternative Pathway) Mediated by Mannose-binding lectin (MB-Lectin pathway): Week 5 Magic Bullets Mannose is a sugar found on the membrane of the invader Lectin binds to it Activation o Activated complement proteins cleave off specific parts of themselves and these parts aid in the killing of pathogens: Act as chemokines to recruit more inflammatory cells Opsonise pathogens (stick to them to enhance phagocytosis) Kill pathogens Antimicrobial proteins o Released by innate immune cells: causes swelling and lysis of cell Inflammatory proteins: o Instigates innate immune response to pathogen invasion o e.g. IL-1, TNF-α, IL-8, histamine, bradykinin (pain), etc Antimicrobial reactive oxygen species o Oxidises bacteria 2. Describe the inflammatory response to infection Week 5 Magic Bullets 1.Upon contact with pathogen - 'non self proteins' - the epithelial cells are activated (due to damage, etc: PAIN) 2. Activated >>> cytokine and chemokine release E.g. Interleukins, Leukotrienes, Bradykinin, Prostaglandins, Histamine, Tumour Necrosis Factor Alpha (TNF-α), etc, etc Cytokines and chemokines have paracrine (short distance cell-cell) and autocrine (self) signalling effects on surrounding tissues Can be produced by any cells Highly pleiotrophic effects (many biological activities) Central to inflammatory response 3. Histamine, IL-1 and TNFα modulate changes to the endothelial cells (blood vessel walls) Increased permeability (swelling) Increased capillary diameter (redness + heat) Increased adhesive properties Changes result in increased cell traffic and diffusion of fluid and cells through the capillary wall 4. Phagocytic Neutrophils respond to chemokine IL-8: Cell Migration Cytokine activated endothelial cells express adhesion molecules: selectins Selectins recognise glycocalyx (sugar/CHO coating of cell membrane - specific to each cell for 'recognition' purposes) of the innate immune cells and then tether and roll them onto the affected endothelial cells Phagocytic Neutrophil is then ACTIVATED Epithelial cytokines activate ICAM (Intracellular Adhesion Molecule) expression Selectin is shed to become an Integrin Cell activation changes integrin to high affinity ICAM 5. Cell migration and diapedesis: Neutrophil adheres and flattens to migrate between the endothelial cells Follows chemokine gradient towards site of infection Migrate readily to IL-8 made by epithelial cells that have encountered pathogens 6. Action of the Innate immune cells : recognise patterns and communicate with adaptive immune system o DAMPs (damage associated molecular patterns) o PAMPs (pathogen associated molecule patterns) involved in cell killing: o phagocytosis: Non-Opsonic: cell recognition of PAMPs Opsonic: recognition of pathogens via antibodies o reactive O2 species o antimicrobial peptides Picture: Tethering and Rolling Week 5 Magic Bullets 3. Describe the cells and their functions involved in phagocytosis of invading micro-organisms Neutrophils: Phagocytosis Antimicrobial reactive oxygen species Antimicrobial peptides Short life span Rapidly produced in response to infection Involved in very initial, acute stages Monocytes/Macrophages: PRIMARY signallers and eaters! Monocyte = immature macrophage Migrate into tissue >>>> become macrophage Different names in different areas of body Functions in immunity: o Phagocytosis o Antimicrobial reactive oxygen species o Secrete inflammatory mediators o Antigen presenting cells Dendritic Cells: PRIMARY Antigen presenting cells Phagocytosis Secrete cytokines 4. Describe the role of: antimicrobial peptides, reactive oxygen species and the complement system Information as covered above: Antimicrobial proteins o Released by innate immune cells: causes swelling and lysis of cell Week 5 Magic Bullets Antimicrobial reactive oxygen species o Oxidises bacteria Complement system: o Circulating proteins secreted by the liver, macrophages/monocytes OR epithelial cells which become 'activated' under specific circumstances o Activation: Mediated by Antibodies (Classical Pathway) Mediated by Antigens/Pathogen surface (Alternative Pathway) Mediated by Mannose-binding lectin (MB-Lectin pathway): Mannose is a sugar found on the membrane of the invader Lectin binds to it Activation o Activated complement proteins cleave off specific parts of themselves and these parts aid in the killing of pathogens: Act as chemokines to recruit more inflammatory cells Opsonise pathogens (stick to them to enhance phagocytosis) Kill pathogens 5. Identify the cytotoxic action of NK cells against infected target cells: As above: Natural Killer Cells: Phagocytes release interferons (cytokines) to activate the NK cells NK cells cause programmed cell death in affected self-cells o React to stress molecules from affected cells o React to non self cells or tumour cells (do not produce normal self recognition molecules) Recognises and responds to antibodies Week 5 Magic Bullets RESPIRATORY VIRUSES 1. Outline the major groups of viruses infecting the respiratory system, including influenza, paramyxoviruses, rhinoviruses, coronaviruses and adenoviruses. Viruses are obligate intracellular parasites. The most fundamental characteristic of a virus is that it is absolutely dependent on a living host (cell) for its reproduction. Virus Family VIRUS Orthomyxovirus Paramyxoviridae Picornaviruses Coronaviridae Adenoviridae Influenza A, B, C (RNA virus) Respiratory syncytial virus (RNA virus) Rhinovirus (most common cause of the common cold) (RNA virus) Coronaviruses (cause 15% common colds) (RNA virus) Adenoviruses (DNA virus) Airborne particles (small) eg sneezing. Widely spread by school children Inhalation of large aerosol droplets Inhalation of droplets, contact with contaminated hands Inhalation of droplets, contact with contaminated hands Transmission by aerosol, close contact, faecal-oral route, or fingers and ophthalmologic instruments (eye infections) Adults, children, elderly, immunecompromised, elderly with cardiac and respiratory problems at risk Ubiquitous: global pandemics, local epidemics. More common in winter Infants, children (most common cause of RT infection in children), adults All ages All ages coming into contact with animal carriers Children, day care centres, military camps, swimming clubs. Ubiquitous Incidence seasonal Disease more common in early autumn, late spring Disease more common in winter, early spring Ubiquitous, no seasonal incidence VACCINES Influenza A + B vaccine (annually) Antiviral drugs (eg amantadine) No vaccines. Antiviral drugs No vaccines. Antiviral drugs for infants No vaccines Live, attenuated vaccine. LOCATION AFFECTED URT, LRT (others outside RT) Respiratory tract, most commonly LRT Mostly limited to URT, replicate in the nasopharynx URT URT, LRT (also affect eye, GIT) CLINICAL SIGNS Sore throat, cough, nasal congestion. Systemic: muscle aches, fever, chills, malaise, Most commonly in children: Bronchiolitis, pneumonia Adults: generally common cold symptoms. Common cold, major factor in asthma exacerbations. Common cold (afebrile), SARS. Infants: associated with gastroenteritis Febrile. Bronchitis, common cold, sore throat, conjunctivitis, diarrhoea, pneumonia TRANSMISSION RISK FACTORS DISTRIBUTION OF VIRUS 2. Identify the steps in the viral infection cycle with particular reference to infection of the respiratory epithelium. Respiratory Tract as site of entry The respiratory tract in the most common route of entry for viruses. Other common sites of entry include mucosal linings of the alimentary, and urogenital tract, the outer surface of the eye and the skin. The cell imposes multiple barriers to virus entry. Viruses must overcome the mechanical barrier of the mucosal lining. This mucosal lining traps Week 5 Magic Bullets microorganisms where they may be carrier to the back of the throat via cilia and either coughed or swallowed (digested and degraded). However, viruses exploit fundamental cellular processes to gain entry to cells and deliver their genetic cargo. Virus entry pathways are largely defined by the interactions between virus particles and their receptors at the cell surface. These interactions determine the mechanisms of virus attachment, uptake, intracellular trafficking, and, ultimately, penetration to the cytosol. Micro-organisms can avoid this by: Adhesions: specialised molecules, which enable binding to the receptor cell. Inhibiting the action of cilia. The Human Respiratory Tract Mucus layer Brush border Most transmission via the respiratory tract occurs through sneezing and coughing which allows movement of mucosal secretions. Increased nasal secretions that accompany many respiratory infections assist by increasing the number of virus carrying droplets available to transmit the micro-organism. 1. Attatchment: The virus binds to the surface of the cell through adhesions. 2. Penetration: Fusion of the viral and host membranes, or uptake via a phagosome, results in the virus carried across the plasma membrane and into the cytoplasm. 3. Uncoating: The viral envelope and/or capsid are shed and the viral nucleic acids released. At this point the virus is no longer infective. Not until the virus has replicated and exits cell. 5. Transcription and/or translation. 4. Virus replicates: Viruses contain either DNA or RNA (never both). Viruses containing DNA, mRNA can form using the host’s RNA polymerase. Viruses with only RNA must use their own RNA polymerases. 6. Assembly: Combining the replicated nucleic acid with newly synthesized capsomeres. 7. Release: Exit from the host cell. The epithelium may be left compromised. For example in a rhinovirus the DNA is replicated within the cytoplasm and exists via cell lysing instead of budding. This results in epithelial damage, and thus prone to secondary infection. This was seen in Mrs A’s case in Magic Bullets. Week 5 Magic Bullets 3. Identify the location in the respiratory system typically infected by these agents, and the clinical pattern invoked. Upper Respiratory Infections: Common Cold, Sinusitis, Pharyngitis, Epiglottitis and Laryngotracheitis. Most upper respiratory infections are of viral aetiology. Common Cold Aetiology: Common colds are the most prevalent entity of all respiratory infections. Rhinoviruses are the most common pathogens. Coronaviruses, Parainfluenza viruses, respiratory syncytial virus, adenoviruses and influenza viruses have all been linked to the common cold. Pathogenesis: direct invasion of epithelial cells of the respiratory mucosa, but destruction and sloughing of these cells or loss of ciliary activity depends on the specific organism involved. There is an increase in both leukocyte infiltration and nasal secretions. Clinical Manifestations: After an incubation period of 48-72 hours, classic symptoms of nasal discharge, obstruction, sneezing, sore throat and cough. Myalgia and headache may also be present. Fever is rare. Diagnosis: based on symptoms (lack of fever combined with symptoms of localization to the nasopharynx). Prevention/Treatment: symptomatic- decongestants, antipyretics, fluids and bed rest. Avoid infecting others, along with good hand washing, are best measures to prevent spread. Sinusitis Aetiology: Acute sinusitis is most often a secondary response to a primary URT infection of either a bacterial, viral or fungal nature. (Chronic sinusitis - lasts minimum 8 weeks, bacterial origin). Pathogenesis: Impair ciliary action of epithelial lining of sinuses, increased mucous secretions- obstruction and impedes drainage. With bacterial multiplication in the sinus cavities, the mucus is converted to mucopurulent exudates. The pus further irritates the mucosal lining causing more oedema, epithelial destruction and obstruction. Week 5 Magic Bullets Clinical Manifestations: The paranasal sinuses (commonly maxillary, ethmoid) are implicated. Pain, sensation of pressure and tenderness over affected sinus exists. Malaise and low-grade fever may occur. Diagnosis: difficult to distinguish bacterial and viral sinusitis. If resolve within 10 days most likely viral, if persist generally bacterial and antibiotics prescribed. Pharyngitis Aetiology: inflammation of the pharynx. Can be bacterial, viral (adenovirus, herpes simplex virus, Epstein-Barr virus and cytomegalovirus infections) and less commonly fungus. Pathogenesis: viral pathogens invade the mucosal cells of the nasopharynx and oral cavity, resulting in oedema and hyperemia of the mucous membranes and tonsils. Clinical Manifestations: presents with a red, sore, scratchy throat. Inflammatory exudate may cover tonsils. Vesicles or ulcers may be seen on the pharyngeal linings. Depending on pathogen, fever and systemic manifestations such as malaise, myalgia, or headache may present. Diagnosis: Serologic tests may be used to confirm due to viral, mycoplasmal or chlamydial pathogens. Prevention/treatment: symptomatic treatment for viral pharyngitis. The exception is herpes simplex virus, which can be treated with acyclovir if clinically warranted or if diagnosed in immunocompromised patients. Lower Respiratory Infections: Bronchitis, Bronchiolitis and Pneumonia. Although viruses can cause lower respiratory tract infections, most LRI are of bacterial aetiology. Bronchitis and Bronchiolitis Aetiology: respiratory syncytial virus primary cause in infants. Other viruses, including influenza viruses and adenoviruses (as well as occasionally M pneumoniae) are also implicated. Pathogenesis: Infants initially have inflammation and sometimes necrosis of the respiratory epithelium, with eventual sloughing. Bronchial and bronchiolar walls are thickened. Exudate made up of necrotic material and respiratory secretions and the narrowing of the bronchial lumen lead to airway obstruction. Clinical Manifestations: bronchiolitis presents with a cough and fever is common. A deepening cough, increased respiratory rate, and restlessness follow. Retractions of the chest wall, nasal flaring, and grunting are prominent findings. Wheezing or actual lack of breath sounds may be noted, respiratory failure and death may result. Diagnosis: Aspirations of nasopharyngeal secretions or swabs are sufficient to obtain specimens for viral culture in infants with bronchiolitis. Rapid serological diagnostic tests for antibody or viral antigens may be performed on nasopharyngeal secretions. Prevention/Treatment: Respiratory syncytial virus infections in infants may be treated with ribavirin. Pneumonia inflammation of the lung parenchyma, consolidation of lung tissue may be identified by physical examination and chest x-ray. Aetiology: viral pneumonias are rare in healthy adults (exception of pneumonia caused by influenza viruses). A serious complication following influenza virus infection is secondary bacterial pneumonia, particularly s. pneumonia. Respiratory syncytial virus can cause severe pneumonia among infants as well as among institutionalized adults. Adenoviruses may also cause pneumonia. Measles pneumonia may occur in adults. Pathogenesis and Clinical Manifestations: Infectious agents gain access to the lower respiratory tract by the inhalation of aerosolized material, by aspiration of upper airway Week 5 Magic Bullets flora, or haematogenous seeding. Pneumonia occurs when lung defence mechanisms are diminished or overwhelmed. The major symptoms or pneumonia are cough, chest pain, fever, shortness of breath and sputum production. Patients are tachycardia. Headache, confusion, abdominal pain, nausea, vomiting and diarrhoea may be present, depending on the age of the patient and the organisms involved. Microbiologic Diagnosis: Viral infection may be diagnosed by demonstration of antigen in secretions or cultures or by an antibody response, or serologic tests. Prevention/Treatment: Until organism identified, therapy based upon clinical history. Therapy is then directed at the specific organism responsible. Week 5 Magic Bullets Antibiotics and antibacterial agents Antibiotics: 'Biochemicals, originally of microbial origin [now including synthetic and semi-synthetic compounds], that are capable, at low concentrations, of inhibiting the growth of microorganisms' – Macmillan Dictionary of Toxicology NB: Antibiotics are released naturally into the soil by bacteria and fungi, but only came to prominence in the medical sphere with the introduction of penicillin in 1941. Other useful definitions: Host In our case, this is the patient. The organism harbouring the bacteria Bactericidal kills target pathogen Such agents have a low minimal lethal concentration (MLC) i.e. they are effective at relatively low concentrations that won't harm the host Bacteriostatic prevents growth only, and relies on the host's own resistance once treatment is stopped These agents would only be cidal at much higher concentrations which would be harmful to the host Prokaryote - 'before the nucleus' Bacteria, some algae and viruses First cells to evolve on earth, 4 billion years ago. Lack a nucleus or nuclear membrane - instead the DNA is just floating about Eukaryote - 'true nucleus' All multicellular, and some unicellular, organisms including fungi and HUMANS. Defining factor is the presence of a nucleus, nuclear membrane and membrane-bound organelles in the cells 1. Outline the major classes of antibiotics and antibacterial agents Antibiotics can be classified in several ways. The most common method classifies them according to their chemical structure as antibiotics sharing the same or similar chemical structure will generally show similar patterns of antibacterial activity, effectiveness, toxicity and allergic potential. Penicillins β-Lactam ring Mechanism not fully understood 1-5% US adults allergic Cephalosporins β-Lactam ring (very similar to penicillin - see below) Originally isolated from Cephalosporum fungus Broad spectrum Inhibit petpidoglycan synthesis Week 5 Magic Bullets Tetracyclines 4-ring stucture with variety of side chains semi-synthetic and naturally-occurring combine with ribosome subunit to inhibit protein synthesis bacteriostatic Aminoglycosides contain a cyclohexane ring + amino sugars Bind to ribosome subunit Bactericidal Most effective against Gram-negative bacteria Macrolides Erythromycin is the most common one 12-22 carbon latone ring linked to sugars Bacteriostatic binds with rRNA of ribosomal subunit inhibits peptide chain elongation during protein synthesis Sulphonamides structurally analogous to metabolic compounds needed by bacteria compete with these compounds to inhibit them Quinolones Contain 4-quinolone ring synthetic also a family of fluoroquinolones inhibit bacterial DNA gyrase or topoisomerase II broad-spectrum Glycopeptides peptide linked to a disaccharide block peptidoglycan synthesis, specifically the transpeptidation step affects the cell wall Week 5 Magic Bullets 2. Describe and classify their mechanisms of action according to the pathways and processes which are affected · Interfering with bacterial cell wall The most selective antibiotics will interfere with the synthesis of the bacterial cell wall, they do this by: inhibiting transpeptidation enzymes involved in the cross-linking of the polysaccharide chains of the bacterial cell wall peptidoglycan. activating the cell wall lytic enzymes and causing the wall to break down. inhibiting cell wall synthesis by interfering with the action of the lipid carrier that transports wall precursors across the plasma membrane Inhibition of protein synthesis Look back over your notes on protein synthesis to jog your memory about these processes. The antibiotic agent binds to the bacterial ribosome. They attach to either the 30s (small) subunit or the 50s (large) subunit of the bacterial ribosome. The steps in protein synthesis that this can affect are: aminoacyl-tRNA binding peptide bond formation mRNA reading translocation E.g. A) Erythromycin (a macrolide) binds to the rRNA of the 50s subunit and inhibits peptide chain elongation during protein synthesis. E.g. B) Aminoglycoside antibiotics bind to 30s subunit and interfere with protein synthesis in two ways: 1. directly inhibit protein synthesis 2. cause misreading of the genetic code on the mRNA Inhibition of nucleic acid synthesis They achieve this through: Inhibiting bacterial DNA gyrase and thus interfere with DNA replication, transcription and other activities Blocking RNA synthesis by binding to and inhibiting the DNA-dependent RNA polymerase Week 5 Magic Bullets This affects DNA replication and repair, and transcription as well as chromosome separation Damage to cell membranes the antibiotic binds to the bacterial plasma membrane and disrupts its structure and permeability properties Antimetabolites These antibiotics block metabolic pathways by competitively inhibiting the use of metabolites by key enzymes. For example, sulphonamides inhibit the folic acid metabolism of bacteria. Unlike humans, who get it from their diet, most bacterial pathogens must synthesise folic acid. The antibiotic competes with p-aminobenzoic acid for the active site of the enzyme involved in folic acid synthesis, and the folate production decreases. Because it's so important to their normal function, the bacterial growth will stop. 3. Identify the reasons for antibiotics being relatively less toxic to the host The key to antibiotic efficacy is selective toxicity - the ability to kill or cease growth in bacteria, but leave the host relatively unscathed. The degree of selectivity depends on: 1. Therapeutic dose - the level required for clinical treatment 2. Toxic dose - the level at which it's too toxic for the host (also referred to as the 'breakpoint' in our lab) The therapeutic index is the ratio of toxic dose: therapeutic dose, and the higher the better. If the antibiotic damages the host cell, you get side effects. The reason most antibiotics have very few side effects on the host is that they target structures, processes and compounds found in prokaryotic or bacterial cells, and not in eukaryotic or human cells. E.g. Cell wall = defining character of prokaryotes. Therefore will not harm the host if it's targeted Folic acid synthesis = a process you won't find going on in human cells, therefore the host isn't harmed when it's targeted Less selective antibiotics will be less effective. E.g. Antibiotics that target the cell membrane or nucleic acid synthesis will be less effective, as the prokaryotic and eukaryotic nucleic acids are not very different, and the same goes for the cell membrane structure Week 5 Magic Bullets Connective tissue LO’s 1) Know the basic composition of connective tissue - Cells (permanent and wandering) - Extracellular matrix (fibers, ground substance and tissue fluids) Embryonic CT CT Proper Specialized CT - mensenchyme - Loose CT - Adipose - Mucous CT - Dense CT; irregular - Blood and regular - Bone - Cartilage - Haemopoetic tissue - Lymphatic Tissue 2) Be able to demonstrate an understanding of the importance of glycosaminoglycans (GAGS) in the function of the extracellular matrix. - “Ground Substance consists of proteoglycans, very large macromolecules composed of core protein to which glycoaminoglycans are covalently bound.” - GAGS; long chain polysaccharides composed of repeating disaccharide units. - Function; -ve chain high density so attracts water; this forms a hydrated gel (hydration/storage of fluids). - Allows diffusion of water-soluble small molecules but movement of large molecules and bacteris is inhibited. - GAGS has binding sites fro mnany growth factors. - Examples of GAGS are Heparin, Keratin sulfate, dermatan and also the more distinctive hyaluronic acid. 3) Identify the key cells and components of connective tissue and describe their function. - Cells; Fibroblasts, myogibroblsast, macrophages, adipose cells, mast cells, mesenchyme calls, - Permanent Components; Collagen fibers, reticular fibers, elastic fibers, ground substances, -> viscous and clear. - Wandering components ; Lymphocytes, plasma cells, neutrophils, Eosinophils, Basophils, Monocytes. 4) Know the basic structure and function of the basement membrane in CT> - Observed with H&E stain (Haemotoxylin and Eosin) immediately adjacent to CT, closely associated layer of collagen fibrils that belong the CT. - Periodic acid-Schiff isolates BM as a clear magenta dense layer between epithelium and CT. Week 5 Magic Bullets Antibiotic Resistance 1. Briefly describe the consequences of antibiotic resistance at the individual and population health levels • If microbes in a patient develop antibiotic resistance, the antibiotic regime may not be effective next time – meaning the infection may not be treatable next time, leading to an infection causing serious illness or death • 1968 – Dysentery epidemic (caused by Shigella) in Guatemala affected 112, 000 and killed 12, 500. The strains responsible for this carried a resistance-plasmid containing resistance to cloramphenicol, tetracycline, streptomycin and sulphonamide • 1972 – Typhoid epidemic (caused by Salmonella typhi) in Mexico affected 100,000 and killed14,000 – with a drug resistance pattern the same as 1968 dysentery outbreak • Worlwide, many strains of S. aureus are already resistant to all antibiotics except vancomycin. Several cases of vancomycin-resistant S. aureus have been reported in US and Japan. If full resistance achieved, it will be unstoppable killer. • The impacts on the individual and population: Increased morbidity and mortality Increased length of hospital stay – leading to decreased bed availability and increased expenses for government health budget Increased cost to patients (increased time off work, increased length of hospital stay, increased expense of medications) Decreased protection from nosocomical infections (hospital acquired infections) 2. Outline measures to reduce its occurrence • Vaccination is one of the most cost-effective methods of microbial disease prevention, and bypasses the use of antibiotics • Prevent inappropriate or excessive prescribing of antibiotics will not solve problem, but will prevent it from worsening “It is estimated that over 50% of antibiotic prescriptions in hospital are given without clear evidence of infection or adequate medical indication” (Prescott 2005) • Renewed emphasis on prevention and control of infection – Improved sanitation, isolation of infected patients and improved hygiene will reduce need for antibiotics • Abolish use of antibiotics in animal food-source could decrease transfer of antibiotic resistant genes from animals to humans – Up to 70% of animal food-source are given antibiotics to mainly promote growth. More than 40% of antibiotics manufactured in U.S. are given to animals • Designing new drugs - In the 1980s pharmaceutical manufacturers, thinking infectious diseases were essentially conquered, cut back severely on searching for additional antibiotics. 3D drug modeling or gene sequencing of bacterial/fungal DNA will help indentify new targets for drugs • Using multiple drugs simultaneously in order to target all microbes, preventing one strain thriving while others die Week 5 Magic Bullets “Consent and informed decision making” 1. Explain the ethical basis for obtaining consent to medical treatment. Revolves around the principles of autonomy and self-determination. Patient has right to choose what happens to his or her own body. Each person has a right to bodily integrity to choose what occurs with respect to his or her own body. ( Ref: “Marion’s Case” (1995) 172, CLR, 218-233 ) Revolves around the issues of patient autonomy and lf determination) 175 CLR 218 at 233 2. Describe the legal requirements for valid consent. Any procedure that involves intentional physical contact with a patient’s body is an invasion of the patient’s bodily integrity and requires valid consent. No consent = Legal action for Assault & Battery Medical practitioners have a legal duty to warn patients of the material risk(s) of the proposed treatment Failure to warn = Legal Action in Negligence Patient needs enough information relative to their particular circumstances to decide whether or not to undergo treatment. Necessary Components – Consent must be: • • • • Voluntary (no duress, pressure, coercion fraud, deceit or drugs) By person with capacity Procedure specific Informed Eg Dept Health and Ageing Immunisation Handbook 9th ed. For consent to be legally valid, the following elements must be present: It must be given by a person with legal capacity, and of sufficient intellectual capacity to understand the implications of being vaccinated. It must be given voluntarily. It can only be given after the relevant vaccine(s) and their potential risks and benefits have been explained to the individual. The individual must have sufficient opportunity to seek further details or explanations about the vaccine(s) and/or their administration. 3. List the exceptions to obtaining consent to medical treatment. In circumstances where immediate treatment is necessary to save a person’s life or to avert a serious and imminent threat (physical or Week 5 Magic Bullets mental), providing there is no unequivocal written direction by the patient to the contrary; If treatment has been authorised by order of a Court, for example, an order of the Supreme Court regarding specific treatment for minor; Procedures authorised by statute – such as compulsory blood, drug and alcohol estimation on the request of a Police Officer; Where a patient is unable to give consent, a guardian, a “person responsible”, or the Guardianship Tribunal may be authorised to give consent on behalf of the patient. 4. Explain the concepts of capacity and competence to consent and provide examples of reduced capacity. Capacity / Competence: Must be able to process the information. The patient must have: • • • • An ability to take in and retain treatment information; To believe it; and To be able to assess the information, balancing the risks and needs. If no capacity to consent – the Guardianship Act 1987 may apply. Or: put another way - the patient must be aware of and have a general level of understanding about the proposed procedure or treatment including associated risks and side-effects. Capacity/competency is also an issue when considering one’s right to refuse treatment. • Competent patients are entitled to refuse medical treatment, or withdraw their consent to treatment. ➝ The High Court of Australia in Marion’s case held that a competent person has the right “to choose what occurs with respect to his or her own person” 1. • Patients may not make logical or reasonable decisions, AND • Refusal of treatment must be documented in the patient notes 1 Secretary, of Health and Community Services v JWB and SMB (1992) 175 CLR 218-58. 5. Describe the elements of effective communication required to enable informed decision-making. • Informed decision making involves:-“A meaningful dialogue between physician and patient, instead of a unidirectional dutiful disclosure of alternatives, risks and benefits by the physician1.” Week 5 Magic Bullets • • • • Delivery of clear, concise unambiguous information. Use plain language to communicate information. Use interpreters when necessary. Ask questions and discuss issues with a person close to them (with their permission). Delivered in language appropriate to the age and interpretive ability of the client. Questioning of patient is encouraged to gauge level of understanding and find out what is important to the patient. Give patients time to reflect on the information. Questions should be answered as fully as possible. Check if patient feels question has been answered. The manner of delivering information may need to be modified if the patient is too ill or badly injured to digest a detailed explanation. Active consent involves both doctor and patient working together towards the achievement of mutually agreed goals, given the material risks of the situation and the expected outcome(s). From this perspective, the world of the doctorpatient relationship is the world where the doctor provides an evidence-based understanding of the risks of the procedure or intervention, and the patient provides the basis for understanding which risks are of personal and material significance for him or her. 6. Describe the requirements of provision of information and disclosure of risks for medical procedures. Need to inform patient of: - Nature of condition - Rationale for proposed treatment - Risks (general, specific and material)* - Alternatives - Time involved, recovery period, follow-up care - Costs *general risks = risks common to the type of procedure eg infection in surgery; specific risks = risks specific to the procedure eg gastric perforation in lap banding; material risks = risk relevant to the particular circumstances of the individual patient. The amount and level of information provided is proportional to the chances of and degree of seriousness of the risks involved. Complex interventions warrant more detailed explanation. 7. Explain what is meant by ‘material risk’ in the context of informed decision making. material risks = risks relevant to the particular circumstances of the individual patient. o Medical practitioners have a legal duty to warn patients of the material risk(s) of the proposed treatment. Failure to warn = Legal Action in Negligence Week 5 Magic Bullets o o Material risks – Rogers v Whitaker: (eye surgery that went badly – not warned) A patient must be warned of all material risks before deciding whether to receive treatment. Courts adopt a patient centred approach. ie : A risk is material if: In the circumstances of a particular case, a reasonable person in the patient’s position, is warned of the risks, would be likely to attach significance to it (OBJECTIVE TEST): OR The medical practitioner is, or should reasonably be, aware that the particular patient, if warned of the risk, would be likely to attach significance to it (SUBJECTIVE TEST). Disclosing Material Risk: • The disclosure of material risks will depend on: – The nature of the risk. – The nature of the intervention. – Patient factors. – Desire for information, questions asked. – Temperament, attitude and level of understanding. 8. Describe the consequences of failure to obtain consent. Background: Criminal liability means the potential loss of freedom for breaking a law of the state prohibiting certain conduct. Civil lliability is generally an order for money damages to be paid to a private individual for a private wrong. · Criminal laws are malum per se, meaning that it is against the moral principles of society. They are normally punished with fines and/or loss of freedom through jail or probation. · Civil laws are malum prohibitum, meaning that they are against the law because someone has said so. These are things like speeding and parking violations. They do not result in loss of freedom, though they can result in loss of privilages or fines. Criminal or civil liability may occur where medical treatment is delivered without his/her consent. • • • • Assault: Conduct that causes a person to apprehend the infliction of bodily harm. Assault: A practitioner may be found to have committed assault if the patient is touched or physically examined without consent. This may extend to assault occasioning actual bodily harm (S59 Crimes Act, 1900) where such treatment results in physical or psychological harm. In addition, a medical practitioner could be liable for the common law offence of false imprisonment, if it can be proved that in treating the patient without consent, the medical practitioner unlawfully restrained the patient’s liberty or freedom of movement. Tort of trespass to the body Week 5 Magic Bullets • • Battery – act of one person which causes some physical contact with another person. Any unauthorised contact may constitute battery – even without hostile intent. Comes down to legally valid consent being sought and gained before examining or laying hands on a patient. Would include detailing what you are going to examine and specifically how you are going to examine. The more invasive or intimate the situation is should dictate how specifically and in what detail you deliver the information. Medical Boards may discipline practitioners failing to gain consent. 9. Describe the consequences of failure to provide information and disclose the risks of a medical procedure. • • • • Goes to the issue of “informed” when looking at consent. Action in negligence can result from failure to obtain informed consent. Action in negligence is to be contrasted to action in trespass. Based on failure to obtain a patient’s informed consent, which requires medical practitioners to disclose more information to the patient, in particular, any material risk of the proposed treatment. Week 5 Magic Bullets Hypotheses of Disease Causation: 1. Examine theories of proving hypotheses & disease causation. (History & Philosophy of Science &Medicine). Sir Bradford Hill: nine criteria for causation, outlining the minimal conditions needed to establish a causal relationship between two items. 1. Strength of the association. How large is the effect? This is defined by the size of the association as measured by appropriate statistical tests. The stronger the association, the more likely it is that the relation of "A" to "B" is causal. 2. The consistency of the association. Has the same association been observed by others, in different populations, using a different method? The association is consistent when results are replicated in studies in different settings using different methods. That is, if a relationship is causal, we would expect to find it consistently in different studies and in different populations. This is why numerous experiments have to be done before meaningful statements can be made about the causal relationship between two or more factors 3. Specificity. Does altering only the cause alter the effect? This is established when a single putative cause produces a specific effect. Can be determined if altering only the cause alters the effect. 4. Temporal relationship. Does the cause precede the effect? Exposure always precedes the outcome. If factor "A" is believed to cause a disease, then it is clear that factor "A" must necessarily always precede the occurrence of the disease. 5. Biological gradient. Is there a dose response? An increasing amount of exposure increases the risk. If a dose-response relationship is present, it is strong evidence for a causal relationship 6. Biological plausibility. Does it make sense? The association agrees with currently accepted understanding of pathological processes. In other words, there needs to be some theoretical basis for positing an association between a vector and disease, or one social phenomenon and another. 7. Coherence. Does the evidence fit with what is known regarding the natural history and biology of the outcome? The association should be compatible with existing theory and knowledge. In other words, it is necessary to evaluate claims of causality within the context of the current state of knowledge within a given field and in related fields. 8. Experimental evidence. Are there any clinical studies supporting the association and can the condition be altered (prevented or ameliorated) by an appropriate experimental regimen? 9. Reasoning by analogy. Is the observed association supported by similar associations? In judging whether a reported association is causal, it is necessary to determine the extent to which researchers have taken other possible explanations into account and have effectively ruled out such alternate explanations. In other words, it is always necessary to consider multiple hypotheses before making conclusions about the causal relationship between any two items under investigation. Historically speaking, discussions of causal criteria arose from the recognised limitations of the Henle-Koch postulates, formalised in the late 19th century to establish causation for infectious agents. These postulates required the causal factor to be necessary and present, applied only to a subset of infectious organisms, and conflict with multifactorial causal explanations. The non-specificity of causal agents was of particular concern Two lists of criteria published before 1960 did not include specificity, and instead included consistency and replication, strength, dose-response, Week 5 Magic Bullets experimentation, temporality and biological reasonableness. The term ‘criteria for causation’ applied to Hill’s list of factors to consider before inferring causation from an observed association. Hill himself however never called these considerations criteria, but rather referred to them as viewpoints and never saw them as the ‘hard-and-fast’ rules of evidence. Nevertheless, the publication of his landmark address to the Royal Society of Medicine is frequently cited as the authorative source for causal criteria in epidemiological practice. 2. Compare and contrast an evidence based medicine approach to disease causation with alternate theories which may be held by patients. Use immunisation as an example of this. Evidence Based Medicine (EBM) is the "conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research." EBM is a movement which aims to increase the use of high quality clinical research in clinical decision making. EBM/EBP recognizes that many aspects of health care depend on individual factors such as quality and vol judgments, which are only partially subject to scientific methods. EBP, however, seeks to clarify those parts of medical practice that are in principle subject to scientific methods and to apply these methods to ensure the best prediction of outcomes in medical treatment, finding out what the patient wants to know and the best possible evidence on which to base answers. Alternative medicine can be seen as any healing practice that does not fall within the realm of conventional medicine or treatments shown not to always be consistently to be effective. Traditional Chinese medicine has been practiced for over 3000 years and over one quarter of the world's population now uses one or more of its component therapies. It combines the use of medicinal herbs, acupuncture, and the use of therapeutic exercises such as Qi Gong. It has proven to be effective in the treatment of many chronic diseases including cancer, allergies, heart disease and AIDS. TCM takes a personalised look at the patient and corrects the underlying causes of imbalance and patterns of disharmony, thus taking a holistic approach. Homeopathy is a non-toxic health care system now used by hundreds of millions of people around the world. An excellent first-aid system and is also superb in the treatment of minor ailments such as earaches, the common cold, and flu. Homeopathy is again based on the treatment of the individual and when used by a knowledgeable practitioner can also be very effective in the cure of conditions such as hay fever, digestive problems, rheumatoid arthritis, and respiratory infections. Naturopathic medicine also strongly believes in the body's inherent ability to heal itself. Naturopathy emphasizes the need for seeking and treating the causes of a disease rather than simply suppressing its symptoms. Naturopaths use dietary modifications, herbal medicines, homeopathy, acupuncture, hydrotherapy, massage, and lifestyle counseling to achieve healing. In terms of immunisation: -immunisation is essentially implemented by Governments and Doctors to which the patient feels they have no autonomy or part in aiding their health. Week 5 Magic Bullets -immunisation is viewed as the use of chemicals and foreign, potentially harmful substances into the body. -immunisations are a general, common, mass made product that can have different side affects for different people. 3. Identify and discuss ethical issues in immunisation. Reason people vaccinate (Some of these reasons also follow into reasons why people do/do not consent for other medical procedures) Anticipatory regret “I will never forgive myself if something went wrong Band wagoning Other people do it, therefore I will do the same Omission bias ‘Feel bad if my failure to do something causes a detrimental outcome to someone else Availability heuristic ‘I just know that it will happen to me, therefore I need to have this done’ Altruism ‘I want to protect others’ ‘recommended’ guidelines say so, therefore I should Want immunity Required by schools, childcare centres Financial incentives/work/employment requirements Reason people don’t vaccinate Adverse reactions often given excessive media coverage such as flu injection last year, the recent case of ‘Tourette’s like symptoms in the US, groups that argue there is a link between the MMR vaccine and autism (google Jenny McCarthy website) Optimism bias ‘It won’t happen to me, therefore it is unnecessary’ Ambiguity aversion too much uncertainty, therefore rather not elect procedure Prefer natural alternatives Preference to receive immunity by contracting the disease (in the case of the pox party) Preference to go ‘against the trend’ Don’t know the importance (eg whopping cough) Presume that if vaccinated as child, then covered (eg: tb) Cost Belief that “I will get the disease if vaccinated “measles vaccine causes measles” Immunisation is not responsible for the decline in communicable diseases; rather improved sanitation, nutrition etc Risk versus benefit The overall risks outweight the benefits further a majority of the risks include minor and limited local irritation and fever. Most people over emphasise the risks associated with vaccinations and underplay those related to catching the actual disease. Relates to the fear of commission compared with omission; side effects from vaccinations is directly from the parents actions whilst obtaining a disease has no level of blame on parents. Public health and paternalism In this process a foreign material is injected into an individual hence compelling one to be immunised against their will and therefore can constitute assault Herd immunity and paradox of free riders Week 5 Magic Bullets Herd immunity is whereby once a critical proportion of a population is immune to a particular disease the disease can no longer circulate through the community. The implication of herd immunity is that if children are not immunised this will not only make them susceptible to infection but also increase risk for others not yet able to be vaccinated. Free riders are parents who live in a highly immunised population and elect not to immunise their children and thus rely on protection of the herd. Week 5 Magic Bullets Measuring Disease Frequency and Association 1. Define prevalence and incidence and discuss the relationship between these measures How does epidemiology describe disease? Incidence How frequently do new cases occur? The incidence rate provides us with a standardised measure, allowing comparison across populations and the testing of hypotheses. It takes into account the population size, and the duration of exposure - it reflects the true magnitude of the disease in the population. It seems there are quite a few meanings and terms used in different ways. Our lecturer described incidence thus: Incidence is a measure of the FREQUENCY of new cases occurring Incidence reflects the pathology of the disease, i.e. a fast-onset disease would have a higher frequency in a defined period than a slow-developing disease There are two types of incidence: 1. Cumulative incidence (incidence) 2. Incidence rate (incidence density) Cumulative incidence (CI) no. of people who get the disease over a certain period ÷ no. of individuals in the population at the beginning of the period Incidence rate (IR) no. of people who get the disease over a certain period ÷ number of person-time when people were at risk of developing the disease The lecturer used the example of students developing glandular fever during their first semester, as follows: 50 students enroll, 5 with a history of GF During semester 1, 5 develop GF No drop outs Once infected with glandular fever, you have lifelong immunity number of persons who develop the disease over time period ÷ average number of people–time they were at risk of developing the disease over same period numerator: 5 developed the disease Week 5 Magic Bullets Denominator: (average number of people at risk) 45 at beginning of semester, and at the end of semester it’s only 40. So the average of the two is 42.5 Now add the time factor: Full semester = 10 weeks 42.5 x 10 weeks = 425 person-time average The incidence rate of glandular fever = 5/425 = 0.012/person-weeks Remember: IR = Figure per person-time (month, year, day etc.) Sometimes you’ll see it as a percentage. Prevalence The amount of disease in a population at a given point in time Prevalence reflects the burden of disease in a population at a single point in time, i.e. the proportion of the population who actually have the disease at that instant. It can show us what the most common disease is in a population, and it is used to assess the impact of disease on public health. number of people who have the disease at time t ÷ total number of people in the population at time t It's expressed as a rate, either as a percentage or per thousand. E.g. the glandular fever scenario: The prevalence of glandular fever is 5 out of 50 = 10% = 100/1000 Prevalence can be divided into two categories: Point prevalence - at a single point in time e.g. on 1/1/12 Period prevalence - from one point in time to another e.g. from 1/1/12 - 3/1/12 The relationship between incidence and prevalence Prevalence measures the existing disease, while incidence measures the rate at which new cases of the disease occur. Prevalence depends on the frequency of new cases duration of the disease population movement prevalence diagram.docx 27.3 KB Week 5 Magic Bullets If incidence increases, so will prevalence (in general - This assumes a static population, however, and a prevalence of 10% or less) Ponder this: If you find a treatment for the disease which means it's no longer fatal, the prevalence will increase because people are no longer dying from the disease, resulting in a higher number of people with the disease in the population However if you find a cure the prevalence will decrease since you've got rid of the disease from the population 2. Identify and interpret measures of association used to describe the relationship between exposure and outcome in epidemiological studies How does epidemiology identify the cause of disease? In order to identify the cause of a disease, we measure the association Association = statistical relationship between two events or characteristics in epidemiology, the association = relationship between exposure and disease Relationship does not imply causation The relationship between cause and effect when we're looking at EXPOSURE Measures of association: Absolute measures: Difference measurement Relative measures: Risk ratios (RR) and odds ratios (OR) The difference between these measurements is illustrated with an example: Week 5 Magic Bullets The absolute risk difference between men and women developing a myocardial infarction is 5 cases/1000/year in males - 1 case/1000/year in females = 4 cases/1000/year The relative risk of myocardial infarction in men compared with women is 5 cases/1000/year in males ÷ 1 case/1000/year in females = 5 1. Difference measures E.g. Attributable risk = risk (exposed) – risk (unexposed) The attributable risk shows the difference in incidence rates between exposed and nonexposed AR<1 cases are less likely to have been exposed likely to have been exposed AR=1 AR>1 exposure has no effect on likelihood of disease cases are more 2. Relative risk Relative risk = measure of disease in the 'exposed population' ÷ measure of the disease in the 'unexposed population' This shows the risk that exposure will have on the outcome RR<1 exposure DECREASES likelihood of disease likelihood of disease NEGATIVE association exposure provides protection RR=1 exposure has no effect on likelihood of disease NO association RR>1 exposure increases POSITIVE association 3. Odds ratio Used as an estimate of risk when disease is rare, and difficult to find in the population Odds ratio = OR<1 Odds of exposure in 'cases' ÷ odds of exposure in 'non-cases' cases are less likely to have been exposed have been exposed OR=1 exposure has no effect on likelihood of disease OR>1 cases are more likely to Week 5 Magic Bullets Communication skills IDENTIFY AND PRACTICE THE COMMUNICATION SKILLS REQUIRED TO ESTABLISH RAPPORT Why establish rapport? It is important to try to put the patient at ease immediately, because unless a rapport is established, the history taking is likely to be unrewarding The treatment of a patient begins the moment one reaches the beside/ the patient enters the consulting rooms The patient’s first impressions of a doctor’s professional manner will have a lasting effect As a doctor (or a medical student in training) you should aim to leave the patient feeling better for their visit How do you establish good rapport? Make a deliberate point of introducing yourself Make a deliberate point of explaining your role. Eg: “Good afternoon, Mrs. Smith. My name is Jess Quinn. I am Dr. Fotheringham’s medical student.” Offer the patient a seat Ensure privacy Sit near the patient close to eye level Address the patient respectfully DISCUSS STRATEGIES FOR EFFECTIVE COMMUNICATION WITH PATIENTS As above In addition – as part of taking patient history, ensure to ask patient what concern has brought them to see doctor today, don’t just make presumption (patientfocussed interview vs. doctor focussed interview) Interview in careful and logical manner Listen carefully Ask questions when appropriately (do not ask questions that patient has already answered – appears that patient has not been listened to) Note non-verbal clues Correctly interpret information obtained IDENTIFY WHAT YOU NEED TO KNOW WHEN INTERVIEWING AND EXAMINING PATIENTS This depends on exactly what patient complaint it, however a general overview at this stage is: o Presenting symptom o History of presenting illness o Past history o Social history o Family history o Systems review DEMONSTRATE THE USE OF APPROPRIATE COMMUNICATION SKILLS IN ELICITING A MEDICAL HISTORY Time for some CCS practice!! Week 5 Magic Bullets