Chapter 8
advertisement
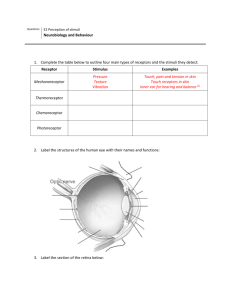
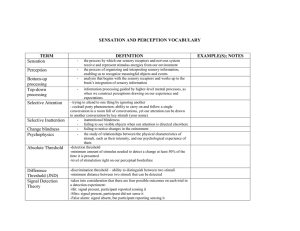
Chapter 12 Sense Organs I. Introduction • The body has millions of sense organs. • A. General sense organs – 1. Function • a. To produce the general or somatic senses such as touch, temperature, and pain, hunger, thirst…. • b. Initiate various reflexes necessary to maintain homeostasis (crucial to survival) • B. Special sense organs –1. Function •a. To produce the special senses of vision, hearing, balance, taste and smell •b. To initial various reflexes necessary to maintain homeostasis II. Receptors • A. Receptor response – responding to stimuli by converting them to serve impulses –1. Different types of receptors respond to different stimuli (ie: heat receptors do not respond to light) –2. when an adequate stimuli acts on a receptor, a sensory neuron’s axon is triggered. Impulses travel over sensory pathways to the brain where they are interpreted as a particular sensation such as heat or cold –3. Adaptation is a common phenomenon experiences by receptors – receptor will adapt to a continuous stimuli and thus the intensity of the resulting sensation decreases. (ie: hot water in a bath tub, feeling your clothes when you first put them on). • C. Classification of receptors –1. By location •a. Externoreceptors – on or near the surface of the body and respond to external stimuli. Sometimes called cutaneous receptors (skin). Examples include those that detect pressure, touch, pain, and temperature. Special sense organs are also classified as externoreceptors. •b. Visceroreceptors (or interoreceptors) – located internally within the substance of body organs (viscera). When stimulated provide info about internal stimuli such as pressure (urinary bladder), stretch, chemical changes, hunger, thirst….. •c. Proprioceptor – specialized type of visceroreceptor – located in skeletal muscles and joints. Provide information on position of body parts. –i. Tonic proprioceptors – locate body parts at resting without looking –ii. Phasic proprioceptors – located body parts during continuous movement. –2. By stimulus detected •a. Mechanoreceptors – activated by stimuli that “deform” the receptor or change its position. Pressure on the skin deform the underlying receptor. •b. Chemoreceptor – activated by amount or changing concentration of certain chemicals (ie: smell and taste) •c. Thermoreceptors – activated by change in temperature •d. Nociceptor – activated by intense stimuli that results in tissue damage. Stimuli can be toxic, chemical, intense light, sound, pressure, heat. The resulting sensation is pain. •e. Photoreceptors – activated by light. Located only in the eye. – 3. By structure •a. Free nerve ending – simplest, most common, widely distributed type of nerve ending. Located throughout the body (externoreceptor and interoreceptor) except in the brain. •The brain is incapable of sensing painful stimuli (so patients are typically awake during brain surgery). Also the receptor that picks up on itching, tickling, and touch. –i. Nociceptor – primary receptor for pain aa. Acute free nerve ending – mediates sharp pain and localized pain sensations bb. Chronic free nerve endings – mediates dull, aching pains –ii. Root hair plexus – a web-like arrangement around hair follicle which detects hair movement (hair standing up on the back of your neck in fight or flight mode) –iii. Merkel discs – sensitive to even the lightest touch •b. Encapsulated nerve endings – surrounded by connective tissue and all are mechanoreceptors –i. Touch and pressure receptors aa. Messiner’s corpuscle – found in hairless skin (fingertips and lips) (a). Two anatomic variations of Messiner’s (i). Krause’s end bulbs – less tightly coiled dentritic endings (ii). Ruffini’s – deeply located in dermis III. Special Sense Organs • A. Vision –1. Eye Anatomy •a. Schlera – outer coat, tough, white fibrous tissue •b. Cornea – transparent portion of the schlera that covers the iris •c. iris – colored portion of the eye. Made up of muscular tissue •d. Pupil – hole which allows light to pass through •e. Lens – refracting mechanism of the eye (bending of light) •f. Retina – innermost part of the eyeball where the image forms. Image is upside down…contains these photoreceptors: –i. Rods – specialized neurons that look like rods. Function best in dim light –ii. Cones – specialized neurons that look like cones. Function best in bright light •g. Accessory structures –i. Lacrimal glands – secretes tears that function to wash debris form the eye. They drain either out the tear ducts or down into the nose (which is why your nose runs when you cry) –ii. Eyebrows – keep sweat from getting into eyes –iii. Eyelashes – keeps foreign objects from getting into eyes –iv. Eyelids – function as the windshield wipers for the eye (keeps the eyeball moist) –2. Neural Pathway of vision •a. Fibers conduct impulses form the rods and cones to the optic nerve •b. Optic nerves from each eye cross in the optic chiasma •c. Optic tracts take the visual information to the visual cortex of the brain for interpretation –3. 20/20 vision means that a person can see at 20 feet what the “normal” eye should see clearly at that distance. Some people see better than the “normal” eye: 20/15 means that they can see at 20 feet what the normal eye can see at 15 feet –4. Red eye in photographs – the flash reflects off the layer of blood vessels that lie between the retina and schlera • B. Smell –1. Olfactory Anatomy •a. Olfactory sense organs consist of: –i. Olfactory cilia – hair-like projections that wave around mixing the mucous in the upper surface of the nasal cavity (that is why you have to “sniff” or inhale big when you are trying to smell something, to get the gas molecules past the cilia ii. Olfactory cells – chemoreceptors that respond to gas molecules or chemicals in the air. iii. Olfactory epithelium – located in the superior portion of the nasal cavity iv. Olfactory receptors – extremely sensitive and easily fatigued when continuously stimulated (that is why smells that appear strong at first fade away…perfume, cologne, etc) – 2. Olfactory Physiology •a. Examples of primary scents are peppermint, putrid, floral and musk. •b. Most people can identify several hundred scents. Some people can identify as many as 1000’s of scents. Animals have a keen sense of olfaction. Dogs can pick up scents 32 times better than humans, and sharks can pick up scents 11,000 times better than humans. –3. Olfactory neural pathway of smell – if level of odor producing chemicals is sufficient, then the cilia will pick up the scent and pass the nerve impulse onto the olfactory nerve in the olfactory bulb. AFrom there, the impulse passes to the brain (thalamus to the cortex) for recognition and memory storage Olfactory nerves • C. Gustation (taste) –1. Gustatory anatomy •a. Taste buds – projections or papillae on tongue, lining of mouth, throat, roof of mouth, and lips –b. children have approximately 10,000 taste buds but nearly half of them will die by the time a person reaches age 60. –c. the white “stuff” on your tongue in the morning is skin cells that have died during the night. The “bad breath” is the decayed material still in your mouth –2. Gustatory Physiology •a. Taste buds are chemoreceptors that are stimulated by chemicals dissolved in saliva •b. Four primary taste sensations – bitter (back of tongue), sour (back sides of tongue), salty (front sides of tongue) and sweet (tip) •c. Taste cells are sensitive, but fatigue quickly with constant stimulation (ie: you don’t taste gum after chewing it for a little while) –3. Gustatory neural pathway – the taste sensation begins when the substance binds to the taste buds. From the taste buds the nerve impulse is carried via one of te cranial nerves to the medulla oblongata then to the thalamus and then on to the taste area of the cerebral cortex –4. Olfactory and Gustatory process interrelated as sense of taste is highly correlated to sense of smell. When a person has a head cold the nasal cavity becomes swollen and the pathway is blocked so that you can’t pick up the chemical signals resulting in tasteless food • D. Hearing –1. Hearing Anatomy •a. External ear –i. Pinna (auricle) acts as a funnel to bring soundwaves into ear –ii. External auditory meatus (ear canal) secretes ear wax (AKA: cerumen) which traps dirt and dust –iii. Tympanic membrane – (ear drum) stretches across the end of the auditory canal and separates the external ear from the middle ear –iv. Inflammation of the external ear is called swimmer’s ear. AKA: external otitis •b. Middle ear –i. Auditory ossicles (the bones in the ear) – malleus, incus and stapes –ii. Openings into the middle ear (a) one from the external auditory canal (covered by the tympanic membrane) (b) one from Eustachian tube (the tube that leads from the throat to the ear) (c) two from the inner ear – round window and oval window •iii. Eustachian tube – purpose is for equalization of pressure between the inner and outer surfaces of the tympanic membrane….preventing rupture. As you swallow or yawn, it forces air in through the throat which equalizes the pressure on the eardrum from the other side. •iv. Inflammation of the middle ear is called otitis media •C. Inner ear – functions for hearing and for maintaining balance….it is very intricate –i. Vestibule – involved with balance –Ii. Semicircular canals – involved with balance –iii. Chochlea – (means snail). The Organ of Corti is the organ inside the chochlea involved with hearing IV. Disorders of senses • A. Tinnitus – ringing in the ear • B. Sinusitis – inflammation of the sinus pathways • C. Cataracts – cloudy spots on the lens as we age • D. Glaucoma – increased pressure in the eye which damages the retina • E. Floaters – semitransparent specks that float in the field of vision. Some are red blood cells that have leaked out into the retina area and float around the retina • F. Vertigo – dizziness – primary symptom for inner ear infection • G. Visual acuity – clearness/sharpness of visual perception • H. Myopia – nearsightedness • I. Hyperopia - farsightedness V. Doctors of senses •A. Opthalmologist •B. Optometrist •C. ENT (ear, nose and throat) VI. Clinical surgeries • A. Radial keratomy (RK) – makes 6 small incisions around the cornea to allow it to flatten out for myopia patients • B. Astigmatic keratomy (AK) – transverse cuts across the cornea help astigmatism • C. Automated lamellar keratoplasty (ALK) - cuts a thin cap off the cornea surface to shave and reshape the tissue underneath • D. Photorefractice keratectomy (PRK) – “cool” lasers vaporize the cornea tissue to help correct myopia • E. Laser-assisted in situ keratomileusis (LASIK) – cuts the cornea like a lid and bends it back, then lasers are used to vaporize and reshape the tissue underneath. At the end, the cornea cap is replaced.