Biol 155 Human Physiology
advertisement

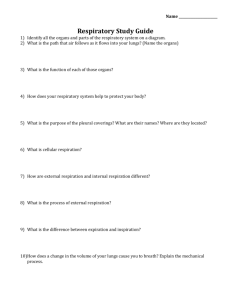
Respiratory physiology: Respiration Ventilation: Movement of air into and out of lungs External respiration: Gas exchange between air in lungs and blood Transport of oxygen and carbon dioxide in the blood Internal respiration: Gas exchange between the blood and tissues Respiratory System Functions Gas exchange: Oxygen enters blood and carbon dioxide leaves Regulation of blood pH: Altered by changing blood carbon dioxide levels Voice production: Movement of air past vocal folds makes sound and speech Olfaction: Smell occurs when airborne molecules drawn into nasal cavity Protection: Against microorganisms by preventing entry and removing them Respiratory System Divisions Upper tract Nose, pharynx and associated structures Lower tract Larynx, trachea, bronchi, lungs Nasal Cavity and Pharynx Nose and Pharynx Nose External nose Nasal cavity Functions Passageway for air Cleans the air Humidifies, warms air Smell Along with paranasal sinuses are resonating chambers for speech Pharynx Common opening for digestive and respiratory systems Three regions Nasopharynx Oropharynx Laryngopharynx Larynx Functions Maintain an open passageway for air movement Epiglottis and vestibular folds prevent swallowed material from moving into larynx Vocal folds are primary source of sound production Vocal Folds Trachea Windpipe Divides to form Primary bronchi Carina: Cough reflex Tracheobronchial Tree Conducting zone Trachea to terminal bronchioles which is ciliated for removal of debris Passageway for air movement Cartilage holds tube system open and smooth muscle controls tube diameter Respiratory zone Respiratory bronchioles to alveoli Site for gas exchange Tracheobronchial Tree Bronchioles and Alveoli Alveolus and Respiratory Membrane Fig. 4. Effects of methacholine on depth of airway surface liquid. a: control tissue not exposed to methacholine. b: 2-min methacholine exposure. Putative sol and mucous gel are clearly visible. c: 30-min exposure. Tissues were radiant etched for 20 s to 1 min. Scale bar 5 20 μm. From Am. J. Physiol. 274 (Lung Cell. Mol. Physiol. 18): L388–L395, 1998.— Lungs Two lungs: Principal organs of respiration Right lung: Three lobes Left lung: Two lobes Divisions Lobes, bronchopulmonary segments, lobules Thoracic Walls Muscles of Respiration Thoracic Volume Pleura Pleural fluid produced by pleural membranes Acts as lubricant Helps hold parietal and visceral pleural membranes together Ventilation Movement of air into and out of lungs Air moves from area of higher pressure to area of lower pressure Pressure is inversely related to volume Alveolar Pressure Changes Changing Alveolar Volume Lung recoil Causes alveoli to collapse resulting from Elastic recoil and surface tension Surfactant: Reduces tendency of lungs to collapse Pleural pressure Negative pressure can cause alveoli to expand Pneumothorax is an opening between pleural cavity and air that causes a loss of pleural pressure Normal Breathing Cycle Compliance Measure of the ease with which lungs and thorax expand The greater the compliance, the easier it is for a change in pressure to cause expansion A lower-than-normal compliance means the lungs and thorax are harder to expand Conditions that decrease compliance Pulmonary fibrosis Pulmonary edema Respiratory distress syndrome Pulmonary Volumes Tidal volume Inspiratory reserve volume Amount of air inspired forcefully after inspiration of normal tidal volume Expiratory reserve volume Volume of air inspired or expired during a normal inspiration or expiration Amount of air forcefully expired after expiration of normal tidal volume Residual volume Volume of air remaining in respiratory passages and lungs after the most forceful expiration Pulmonary Capacities Inspiratory capacity Functional residual capacity Expiratory reserve volume plus the residual volume Vital capacity Tidal volume plus inspiratory reserve volume Sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume Total lung capacity Sum of inspiratory and expiratory reserve volumes plus the tidal volume and residual volume Spirometer and Lung Volumes/Capacities Minute and Alveolar Ventilation Minute ventilation: Total amount of air moved into and out of respiratory system per minute Respiratory rate or frequency: Number of breaths taken per minute Anatomic dead space: Part of respiratory system where gas exchange does not take place Alveolar ventilation: How much air per minute enters the parts of the respiratory system in which gas exchange takes place Physical Principles of Gas Exchange Partial pressure The pressure exerted by each type of gas in a mixture Dalton’s law Water vapor pressure Diffusion of gases through liquids Concentration of a gas in a liquid is determined by its partial pressure and its solubility coefficient Henry’s law Physical Principles of Gas Exchange Diffusion of gases through the respiratory membrane Depends on membrane’s thickness, the diffusion coefficient of gas, surface areas of membrane, partial pressure of gases in alveoli and blood Relationship between ventilation and pulmonary capillary flow Increased ventilation or increased pulmonary capillary blood flow increases gas exchange Physiologic shunt is deoxygenated blood returning from lungs Oxygen and Carbon Dioxide Diffusion Gradients Oxygen Moves from alveoli into blood. Blood is almost completely saturated with oxygen when it leaves the capillary P02 in blood decreases because of mixing with deoxygenated blood Oxygen moves from tissue capillaries into the tissues Carbon dioxide Moves from tissues into tissue capillaries Moves from pulmonary capillaries into the alveoli Changes in Partial Pressures Hemoglobin and Oxygen Transport Oxygen is transported by hemoglobin (98.5%) and is dissolved in plasma (1.5%) Oxygen-hemoglobin dissociation curve shows that hemoglobin is almost completely saturated when P02 is 80 mm Hg or above. At lower partial pressures, the hemoglobin releases oxygen. A shift of the curve to the left because of an increase in pH, a decrease in carbon dioxide, or a decrease in temperature results in an increase in the ability of hemoglobin to hold oxygen Hemoglobin and Oxygen Transport A shift of the curve to the right because of a decrease in pH, an increase in carbon dioxide, or an increase in temperature results in a decrease in the ability of hemoglobin to hold oxygen The substance 2.3-bisphosphoglycerate increases the ability of hemoglobin to release oxygen Fetal hemoglobin has a higher affinity for oxygen than does maternal Oxygen-Hemoglobin Dissociation Curve at Rest Bohr effect: Temperature effects: Shifting the Curve Transport of Carbon Dioxide Carbon dioxide is transported as bicarbonate ions (70%) in combination with blood proteins (23%) and in solution with plasma (7%) Hemoglobin that has released oxygen binds more readily to carbon dioxide than hemoglobin that has oxygen bound to it (Haldane effect) In tissue capillaries, carbon dioxide combines with water inside RBCs to form carbonic acid which dissociates to form bicarbonate ions and hydrogen ions Transport of Carbon Dioxide In lung capillaries, bicarbonate ions and hydrogen ions move into RBCs and chloride ions move out. Bicarbonate ions combine with hydrogen ions to form carbonic acid. The carbonic acid is converted to carbon dioxide and water. The carbon dioxide diffuses out of the RBCs. Increased plasma carbon dioxide lowers blood pH. The respiratory system regulates blood pH by regulating plasma carbon dioxide levels CO2 Transport and Cl- Movement Ventilation-perfusion coupling: Respiratory Areas in Brainstem Medullary respiratory center Dorsal groups stimulate the diaphragm Ventral groups stimulate the intercostal and abdominal muscles Pontine (pneumotaxic) respiratory group Involved with switching between inspiration and expiration Respiratory Structures in Brainstem Rhythmic Ventilation Starting inspiration Increasing inspiration Medullary respiratory center neurons are continuously active Center receives stimulation from receptors and simulation from parts of brain concerned with voluntary respiratory movements and emotion Combined input from all sources causes action potentials to stimulate respiratory muscles More and more neurons are activated Stopping inspiration Neurons stimulating also responsible for stopping inspiration and receive input from pontine group and stretch receptors in lungs. Inhibitory neurons activated and relaxation of respiratory muscles results in expiration. Modification of Ventilation Cerebral and limbic system Chemical control Respiration can be voluntarily controlled and modified by emotions Carbon dioxide is major regulator Increase or decrease in pH can stimulate chemosensitive area, causing a greater rate and depth of respiration Oxygen levels in blood affect respiration when a 50% or greater decrease from normal levels exists Modifying Respiration Regulation of Blood pH and Gases Herring-Breuer Reflex Limits the degree of inspiration and prevents overinflation of the lungs Infants Reflex plays a role in regulating basic rhythm of breathing and preventing overinflation of lungs Adults Reflex important only when tidal volume large as in exercise Ventilation in Exercise Ventilation increases abruptly At onset of exercise Movement of limbs has strong influence Learned component Ventilation increases gradually After immediate increase, gradual increase occurs (4-6 minutes) Anaerobic threshold is highest level of exercise without causing significant change in blood pH If exceeded, lactic acid produced by skeletal muscles Effects of Aging Vital capacity and maximum minute ventilation decrease Residual volume and dead space increase Ability to remove mucus from respiratory passageways decreases Gas exchange across respiratory membrane is reduced