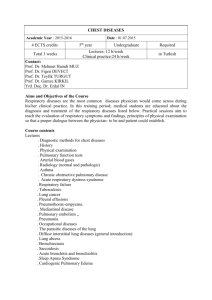
Chapter 6: Respiration
advertisement

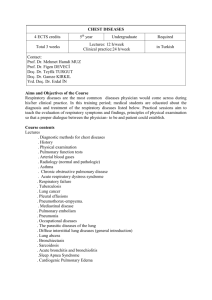
chapter 6 The Respiratory System and Its Regulation External Respiration Pulmonary ventilation involves inspiration and expiration. Pulmonary Diffusion is the exchange of oxygen and carbon dioxide between the lungs and the blood. RESPIRATORY SYSTEM Process of Inspiration and Expiration Lung Volumes Measured by Spirometry Reprinted, by permission, from J. West, 2000, Respiratory physiology: The essentials (Baltimore, MD: Lippincott, Williams, and Wilkins), 14. Pulmonary Diffusion • Replenishes blood's oxygen supply that has been depleted for oxidative energy production • Removes carbon dioxide from returning venous blood • Occurs across the thin respiratory membrane Laws of Gases Dalton's Law: The total pressure of a mixture of gases equals the sum of the partial pressures of the individual gases in the mixture. Henry's Law: Gases dissolve in liquids in proportion to their partial pressures, depending on their solubilities in the specific fluids and depending on the temperature. Partial Pressures of Air • Standard atmospheric pressure (at sea level) is 760 mmHg. • Nitrogen (N2) is 79.04% of air; the partial pressure of nitrogen (PN2) = 600.7 mmHg • Oxygen (O2) is 20.93% of air; PO2 = 159.1 mmHg. • Carbon dioxide (CO2) is 0.03%; PCO2 = 0.2 mmHg. Did You Know…? The solubility of a gas in blood and the temperature of blood are relatively constant. Differences in the partial pressures of gases in the alveoli and in the blood create a pressure gradient across the respiratory membrane. This difference in pressures leads to diffusion of gases across the respiratory membrane. The greater the pressure gradient, the more rapidly oxygen diffuses across it. Comparison of Pressure (mmHg) in the Pulmonary and Systemic Circulations Reprinted, by permission, from J. West, 2000, Respiratory physiology: The essentials (Baltimore, MD: Lippincott, Williams, and Wilkins), 36. Anatomy of the Respiratory Membrane Partial Pressures of Respiratory Gases at Sea Level Partial pressure (mmHg) Gas % in dry air Dry air Alveolar air Venous blood Diffusion gradient Total 100.00 760.0 760 760 0 H2O 0.00 0.0 47 47 0 20.93 159.1 104 40 64 0.03 0.2 40 45 5 79.04 600.7 569 573 0 O2 CO2 N2 Key Points Pulmonary Diffusion • Pulmonary diffusion is the process by which gases are exchanged across the respiratory membrane in the alveoli to the blood and vice versa. • The amount of gas exchange depends on the partial pressure of each gas. • Gases diffuse along a pressure gradient, moving from an area of higher pressure to lower pressure. (continued) Key Points (continued) Pulmonary Diffusion • Oxygen diffusion capacity increases as you move from rest to exercise. • The pressure gradient for carbon dioxide exchange is less than for oxygen exchange, but carbon dioxide’s membrane solubility is 20 times greater than oxygen, so CO2 crosses the membrane easily. Oxygen Transport • Hemoglobin concentration largely determines the oxygen-carrying capacity of blood. • Increased H+ (acidity) and temperature of a muscle allow more oxygen to be unloaded there. • Training affects oxygen transport in muscle. Oxyhemoglobin Dissociation Curve Carbon Dioxide Transport • Dissolved in blood plasma (7% to 10%) • As bicarbonate ions resulting from the dissociation of carbonic acid (60% to 70%) • Bound to hemoglobin (carbaminohemoglobin) (20% to 33%) Arterial–Venous Oxygen Difference Did You Know…? The increase in (a-v)O2 difference during strenuous exercise reflects increased oxygen use by muscle cells. This use increases oxygen removal from arterial blood, resulting in a decreased venous oxygen concentration. Factors Affecting Oxygen Uptake and Delivery 1. Oxygen content of blood 2. Amount of blood flow 3. Local conditions within the muscle Key Points External and Internal Respiration • Oxygen is largely transported in the blood bound to hemoglobin and in small amounts by dissolving in blood plasma. • Hemoglobin saturation decreases when PO2 or pH decreases or if temperature increases. These factors increase oxygen unloading in a tissue that needs it. • Hemoglobin is usually 98% saturated with oxygen, which is higher than what our bodies require, so the blood's oxygen-carrying capacity seldom limits performance. (continued) Key Points (continued) External and Internal Respiration • Carbon dioxide is transported in the blood as bicarbonate ion, in blood plasma or bound to hemoglobin. • The (a-v)O2 difference—a difference in the oxygen content of arterial and venous blood—reflects the amount of oxygen taken up by the tissues. • Carbon dioxide exchange at the tissues is similar to oxygen exchange except that it leaves the muscles and enters the blood to be transported to the lungs for clearance. Regulators of Pulmonary Ventilation at Rest • • • • • • Higher brain centers Chemical changes within the body Chemoreceptors Muscle mechanoreceptors Hypothalamic input Conscious control Pulmonary Ventilation Ventilation (VE) is the product of tidal volume (TV) and breathing frequency (f): VE = TV x f