Pulmonary Gas Exchange and Gas Transport
advertisement

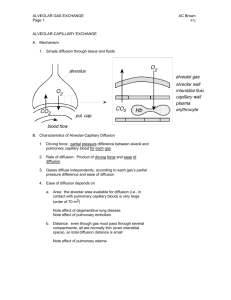
Pulmonary Gas Exchange and Gas Transport Dr. Meg-angela Christi Amores Physiologic Anatomy One of the most important problems in all the respiratory passages is to keep them open to allow easy passage of air to and from the alveoli • Trachea – with cartilage rings 5/6 of the way around • Bronchi – walls have less extensive cartilage plates • Bronchioles – no plates. Diameter <1.5mm, all smooth muscles – Kept expanded by same transpulmonary pressures that expand the alveoli Physiologic Anatomy All areas of the trachea and bronchi not occupied by cartilage plates, walls are composed of smooth muscles Resistance to flow is greatest NOT in the minute air passages of terminal bronchioles but in some of the larger bronchi near to the trachea. Smaller airways are easily occluded ; smooth muscles = contract easily Pulmonary Circulatory System • Pulmonary Vessels – Pulmonary artery (5 cm, thin, 2x VC, 1/3 aorta) • Right and Left main pulmonary branches – lungs • Large compliance (7 mL/mmHg) • Allows pulmonary arteries to accommodate 2/3 of stroke volume output of Right Ventricle – Bronchial Vessels – arterial supply to the lungs • 1/3 of cardiac output • Supplies supporting tissues (CT, septa, bronchi) • Drains to pulmonary veins Pulmonary vs. Alveolar Ventilation • Pulmonary Ventilation – Inflow and outflow of air between the atmosphere and the lung alveoli • Alveolar Ventilation – Rate at which new air reaches the areas in the lung where it is in proximity to the pulmonary blood or gas exchange areas (alveolar sacs, ducts, respiratory bronchioles) Diffusion of Gases • Diffusion – Random molecular motion of molecules with energy provided by kinetic motion of the molecules – All molecules are continually undergoing motion except in absolute zero temperature – Net diffusion • Product of diffusion from high to low concentration Gas Pressures • Partial Pressure – Pressure is directly proportional to the concentration of gas molecules; caused by impact of moving molecules against a surface – In respiration, there’s mixture of gases: O2, N2, CO2 – Rate of diffusion of each gas is directly proportional to the pressure caused by each gas alone • AIR = total Pressure 760 mmHg • 79% N, 21% O2 = PP N = 600mmHg , PP O2 =160mmHg Gas Pressure in Fluid • Determined by its concentration and by solubility coefficient • If gas is repelled, pressure increases • HENRY’s LAW : Pressure = concentration solubility coefficient Solubility of Gases in body temp. • • • • • O2 = 0.024 CO2 = 0.57 - 20x more soluble than O2 CO = 0.018 N2 = 0.012 He = 0.008 Factors that affect Rate of Gas Diffusion thru Respiratory Membrane • Respiratory Unit: – Respiratory bronchiole – Alveolar ducts – Atria – Alveoli (300 Million in both lungs) (0.2mm) *their membranes make up the respiratory membrane Respiratory Membrane • Layers: 1. Layer of fluid lining alveolus (surfactant) 2. Alveolar epithelium 3. Epithelial basement membrane 4. Interstitial Space 5. Capillary basement membrane 6. Capillary endothelial membrane Overall thickness: 0.2um (ave: 0.6 um) Total surface area: 70 m2 Factors that affect Rate of Gas Diffusion thru Respiratory Membrane 1. Thickness of membrane • Inc. in edema and fibrosis 2. Surface area of membrane • Dec. in removal of lung and emphysema 3. Diffusion coefficient of Gas in substance of membrane • Gas’ solubility 4. Pressure difference • Difference between partial pressure of gas in alveoli and pressure of gas in pulmonary capillary blood Ventilation-Perfusion Ratio • A concept developed to help us understand respiratory exchange where there is imbalance between alveolar ventilation and alveolar blood flow • Areas in lung with well ventilation but no bloodflow or excellent blood flow but no ventilation • Va – alveolar ventilation • Q – blood flow Ventilation-Perfusion Ratio Va/Q = normal • If Va is 0 (zero), but with perfusion: Va/Q = 0 • If Va is present, but no perfusion Va/Q = infinity • In both: there is no gas exchange Ventilation-Perfusion Ratio • Normal person : – Upright: Va and Q are less in Upper part but Q is more – At top of lung: Va/Q 2.5x > as ideal = physiologic dead space (ventilation but less blood flow) – At bottom: Va is less than Q • Va/Q is 0.6 < as ideal = physiologic shunt • COPD patient: – Smoker, emphysema, alveolar walls destroyed – Wasted blood flow = severe shunting Transport of O2 and CO2 • Pressure differences causes gas to diffuse Alveolus Capillaries Tissues (fluid) Tissues (cells) pO2 104 mmHg 95 mmHg 40 mmHg 5-40 (ave 23) mmHg pCO2 40 mmHg 45 mmHg 45 mmHg 46 mmHg Transport of O2 and CO2 • CO2 can diffuse about 20 times as rapidly as O2 Transport of O2 in blood: • 97% of O2 from lungs to tissues are carried in combination with hemoglobin • O2 combines loosely and reversibly with heme pO2 – O2 combines with heme (pulm capi) pO2 – O2 is released (tissue capillaries) • For the next meeting, read on Regulation of Respiration • Guyton Textbook of Medical Physiology, 10th edition Chapter 41