Learning to Practice and Teach Evidence
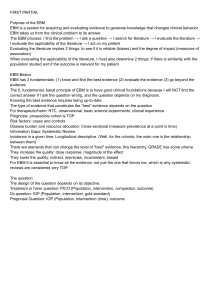
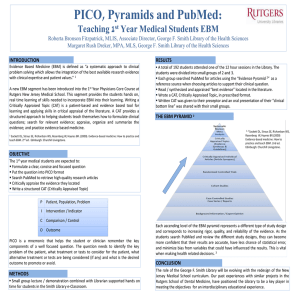
advertisement

(First Annual) Learning to Practice and Teach Evidence-based Health Care An Intensive Workshop Introductions • • • • • Robert Wild & Dave Thompson Susan Hollingsworth Speakers Facilitators Participants A true story • A randomized trial of treating high blood pressure on the jobsite (a steel mill) vs. referral for treatment to primary care doctor • Primary outcome: treatment compliance • No difference in compliance between the groups • Some patients who were referred with documented hypertension did not get treated Determinants of the clinical decision to treat some, but not other, high blood pressure patients: 1 The level of diastolic blood pressure. 2 The patient’s age. 3_ 4 The amount of target-organ damage. Determinants of the clinical decision to treat some, but not other, hypertensive patients: 1 The level of diastolic blood pressure. 2 The patient’s age. 3 The physician’s year of graduation from medical school. 4 The amount of target-organ damage. How we “know” • observations in the world • clinical experience – open to bias • specious causal connections • vividness and immediacy • small samples • laboratory and physiological research – systematic but generalization dangerous • observational studies – non-comparable groups What we (did) know that ain’t so: • HRT to decrease cardiovascular risk – observational studies consistently suggest decreased risk – RCTs show increased risk • High flow oxygen for RDS – My 6th grade pen-pal was in the “gifted children” class at the Ohio state school for the blind • Anti-arrythmics post-MI Contrasting Reasoning • Patho-physiologic reasoning – Depends on logic and knowledge of pathophysiology – This leads to a decision to prescribe flecainide to patients after heart attack • Evidence from systematic studies in human subjects: – Randomized trial of flecainide after MI: • 7.7% dead on flecainide • 3.0% dead on placebo – Leads to a decision NOT to prescribe flecainide after MI Hierarchy of Evidence Meta-analysis of RCTs systematic review of RCTs Individual RCT Observational studies patient-important outcomes Basic research test tube, animal, human physiology Clinical experience Why don’t we practice EBM? • • • • Exploding information supply Textbooks are out of date No time to read Traditional CME doesn’t work Asking questions • Practice identifying information needs: – Routinely question decisions – Question routine decisions • Identify the specific issue at hand • Do you need background or foreground information? Identify the type of information that is needed • Background information: What IS myelomonocytic leukemia?? Best source of information for background questions is recent textbooks or recent general review articles. • Foreground information: Should patients with myelomonocytic leukemia be treated with methotrexate? The best information for foreground questions comes from original research in human subjects. Asking Questions • Design a focused clinical question that addresses the information need – Patient/population – Intervention – Comparison if relevant – Outcome • The “PICO question” • PCOS Why bother with EBM? • without EBM we are helpless in the face of – misguided experts – overenthusiastic experts – drug company hype • without EBM our ability is limited – to understand difficult tradeoffs – to help our patients make difficult decisions • with EBM comes – understanding and power – greater effectiveness in helping our patients Seven Alternatives to Evidence Based Medicine • Eminence Based Medicine (marked by radiance of white hair) • Vehemence Based Medicine • Eloquence Based Medicine • Providence Based Medicine • Diffidence Based Medicine • Nervousness Based Medicine • Confidence Based Medicine – (Isaacs and Fitzgerald, BMJ 1999;319:1618) Structure of the Workshop • Breakfast at 8:00am both days • First plenary at 9:15 am on Friday and 9:00am Saturday • Small group sessions – 10:15-11:40 am Friday, 1:30-3:30 pm Friday – Saturday 10:15-11:30 adjourn Sat 11:30 am • Box Lunches Friday and Saturday • Lunchtime registrants hands - on searching session today – Sign up at registration table, limited space • facilitators go to room 251 Provost Conference PM • Reception this afternoon after last plenary 4:45PM • Please turn in your evaluations. CME can be obtained for an additional $25 , slide presentations, and the library resource guide with links to many, many helpful websites will be posted on URL http://moon.ouhsc.edu/dthompso/cdm/ebhc1/ … in your packet Goals of the workshop • To learn and practice skills of critical appraisal of the research literature • To learn techniques for teaching EBM Your own goals • You will have come with your own objectives for the workshop – Please share them with your group Ground Rules • Facilitators are there to facilitate and demonstrate • Please arrive on time and prepared for each session • Have a good time!