Physiology Ch. 10 p115-120 [4-25
advertisement

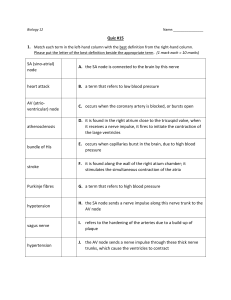
Physiology Ch. 10 p115-120 Rhythmic Excitation of the Heart -the heart can generate rhythmic electrical impulses for contraction and conduct them rapidly -atria contract 1/6s before the ventricles to allow filling of ventricles before their contraction Specialized Excitatory and Conductive System of the Heart – sinus node is where normal rhythmical impulses are generated and conduct to the atrioventricular node in which the message is delayed before passing into ventricles, and the AV bundle (conducts form atria into ventricles), and left and right bundle branches of purkinje fibers Sinus Node (SA Node) – small, flattened piece of cardiac muscle on the superior, posterolateral wall of R atrium below to superior vena cava. No contractile muscle filaments, but connect to atrial muscle fibers Automatic Electrical Rhythmicity of Sinus Fibers – some cardiac fibers are capable of self-excitation that can cause automatic rhythmic discharge and contraction, such as those of the heart and sinus node -resting membrane potential of sinus nodal fiber is -55mV, ventricular muscle fiber is -85mV -cell membranes of sinus fibers are naturally leaky to Na and Ca ions to neutralize some negativity -Cardiac muscle has 3 types of ion channels: 1. Fast Sodium Channels – opening these for 10^-5s causes rapid upstroke action potential in ventricular muscle because of rapid influx of positive Na ions to interior of fiber 2. Slow Na channels - Plateau of ventricular action potential caused by slower opening of which last for 0.3s 3. Potassium channels – allows diffusion of large amounts of positive K+ in outward direction and returns membrane to resting level -in the sinus node, resting membrane potential is -55mV, so the fast Na channels have been inactivated (meaning they have become blocked due to gates on inside of cell that close fast Na channels) -therefore, only slow Na channels can open and cause action potential in the SA node -this is why the atrial node action is slower than ventricular muscle -repolarization to -55mV occurs slowly as well Self-Excitation of Sinus Nodal Fibers – high Na concentration on extracellular fluid as well as number of already open channels on node fiber cause Na to leak from the outside in. In between heartbeats, influx of Na ions causes slow rise in resting membrane potential in positive direction -resting potential gradually rises and becomes less negative between each 2 heartbeats -When potential reaches -40mV, Na/Ca channels open to cause action potential -Two events occur to prevent SA node fibers from remaining depolarized: 1. Na/Ca channels become inactivated within 100ms after opening 2. Greatly increased numbers of potassium channels open after action potential to cause K+ efflux -both of these act to reduce intracellular potential back to negative state -K+ channels remain open for a few 10ths of a second to continue efflux and results in hyperpolarization -hyperpolarization doesn’t stay that negative because K+ channels close and efflux ceases Internodal Pathways and Transmission of Cardiac Impulse through Atria – SA fibers connect with atrial muscle fibers, so action potentials from SA node travel into these fibers and through entire atria to the AV node at a speed of 0.3m/s -several small bands of atrial fibers exist where conduction is more rapid. One of these is called anterior interatrial band which passes through anterior walls of atria to the left atrium -Three other bands exist that curve through anterior, lateral, and posterior walls called the antior, middle and posterior intermodal pathways AV Node and Delay of Impulse from Atria to Ventricles – impulse does not travel from atria to ventricles too rapidly, delay allows time for atria to empty blood into ventricles before ventricular contraction- AV node responsible for the delay -AV node is on posterior wall of right atrium immediately behind tricuspid valve -total delay is 0.16s between SA node signal reaches ventricles -slow conduction is caused by diminished numbers of gap junctions between successive cells in conducting pathways, so there is great resistance to conduction Rapid Transmission in Ventricle Purkinje System – purkinje fibers lead from AV node and AV bundle into the ventricles -very different from AV bundle fibers in that purkinje are large and transmit very fast signals (1.5-4m/s) to allow instantaneous transmission of cardiac impulse throughout the entire ventricular muscle -Speed is caused by high permeability of gap junctions at intercalated discs so ions can go from one cell to another easily to enhance velocity of transmission -have very few myofibrils meaning they do not contract during impulse transmission One Way Conduction through AV Bundle – action potentials from AV bundle cannot travel backward from ventricles to atria to prevent re-entry of impulses into atria and allowing only forward conduction -atria and ventricles separated by fibrous barrier to insulate signal between the two and only allowing it to go through AV node -an abnormal muscle bridge between atria and ventricles can cause impulse to travel backwards and cause cardiac arrhythmia Distribution of Purkinje Fibers in Left and Right Bundle Branches – impulse travels down the AV bundle through ventricular septum toward apex and then divides into left and right bundle branches beneath endocardium and spreads around the apex to turn into each ventricular chamber and back towards the base Transmission of Cardiac Impulse in Ventricular Muscle – Once impulse reaches ends of purkinje fibers, it is transmitted through ventricular muscle mass by ventricular muscle themselves, slower than purkinje -cardiac muscle wraps around heart in double spiral with fibrous septa between layers, so the impulse does not travel directly outward toward surface of heart but instead angulates in spirals -Total time for transmission of impulse from initial bundle branches to ventricular muscle is 0.06s Control of Excitation and Conduction of the Heart – sinus node is the pacemaker of the heart in normal conditions, but in abnormal conditions this may not be the case, in which case other parts of the heart exhibit rhythmical excitation -AV node can discharge at 40-60 times/min if not stimulated by outside source, purkinje as well. -Sinus node is the main pacemaker because its discharge rate is faster than the natural rate of AV or purkinje fibers, so after wave from sinus node hits AV node, second wave comes before the AV’s natural pacemaker takes over Abnormal Pacemakers – some other part of the heart may develop a rhythmical discharge called an ectopic pacemaker such as one in AV node or in purkinje fibers -these cause abnormal sequence initiation and contraction debility -another cause of shift of pacemaker is blockage of transmission of cardiac impulse from SA node to other parts of heart, in which case new pacemaker occurs at AV node or AV bundle -When AV block occurs, when impulse fails to pass from atria into ventricles through AV node and bundle system -atria continue to beat at normal rhythm from sinus node, and a new pacemaker develops in purkinje system and drives ventricular muscle at a new rate -After sudden AV bundle block, purkinje system does not begin to emit intrinsic rhythmical impulses until 5-20s later because before blockage, purkinje system was overdriven by rapid sinus impulses and are in a suppressed state -ventricles fail to pump during these 5-20 seconds, and person faints after 5s -the delayed heartbeat is called Stokes-Adams Syndrome Role of Purkinje System in Synchronous Contraction of Ventricles – purkinje system is so fast that ventricles contract at the same time and continue for another 0.3s -effective pumping by both ventricles requires synchronous contraction, and if it was any slower, much of ventricles would contract slower than the rest to cause cardiac pumping debilities Control of Heart Rhythmicity and Impulse by Sympathetics and Parasympathetics – heart is supplied with both parasympathetic and sympathetic nerves. -Parasymp come from vagus nerve and are distributed to SA and AV nodes and somewhat to muscle of atria and little to ventricles -sympathetic nerves distributed to equal parts of the heart, strongly represented in ventricles -parasympathetic nerves cause acetylcholine to be released at vagal nerve endings -acetylcholine decreases rate of rhythm of sinus node and decreases excitability of AV junctional fibers between atrial musculature and AV node to slow transmission -weak vagal stimulation slows rate of heart pumping, maybe as little as ½ normal -strong vagal stimulation can stop rhythmic excitation by sinus node completely to stop excitatory signals from being transmitted to ventricles -ventricles stop beating for 5-20 seconds, but some small area in purkinje fibers in ventricular septal portion develop its on rhythm of 15-40beats/minute and is called ventricular escape Mechanism of Vagal Effects – ACh at vagal nerve endings increases permability of fibers to potassium ions which allow rapid leakage of K+ out of the fibers to cause hyperpolarization -state of hyperpolarization in the SA node alters membrane potential to -65mV rather than normal -55 -therefore, initial rise of SA node membrane potential caused by inward Na and Ca leakage requires much longer to reach threshold for action potential -in AV node, hyperpolarization caused by vagal stimulation makes it difficult for small atrial fibers entering node to generate enough electricity to excite fibers Effect of Sympathetic Stimulation on Conduction – sympathetics increase rate of SA discharge, increases rate of conduction and level of excitability in all portions of heart, and increases force of contraction of both atrial and ventricular cardiac musculature -stimulation of symp nerves releases norepinephrine at nerve endings to stimulate Beta-1 adrenergic receptors to mediate heart rate (increases permeability of muscle to Na and Ca ions) -this causes resting potential to increase and making it easier to shoot action potential -In AV node, increased Na and Ca permeability makes it easier to excite fiber bundles to decrease time -increase in Ca permeability is partially responsible for increase in contractile strength of muscle