Huffman PowerPoint Slides - HomePage Server for UT Psychology
advertisement

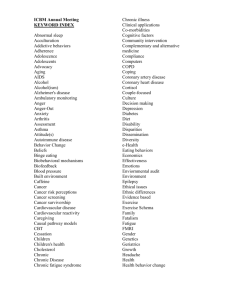
Chapter 8 Psychophysiological Disorders and Health Psychology Ch 8 Psychophysiological Disorders • Psychophysiological Disorders involve genuine physical disorders – Physical symptoms can be caused by or worsened by emotional distress – The category recognizes that a broad range of diseases involving the circulatory, respiratory, digestive and central nervous systems can be influenced by stress Ch 8.1 Leading Causes of Death (1993) – Cardiovascular Diseases – Cancer – Pulmonary Disease – Accidents Disorders of Lifestyle / Behavior Historical Developments – Psychosomatic Medicine – Behavioral Medicine Apply Behavioral Science to the Prevention, Diagnosis, and Treatment of Medical Problems Interdisciplinary Historical Developments – Psychosomatic Medicine – Behavioral Medicine – Health Psychology Study Psychological Factors Important for the Promotion and Maintenance of Heath Not Interdisciplinary Two Kinds of Influence Factors That: – Lead to Illness and Disease – Increase Risk of Developing Disease – Influence Etiology & Maintenance How Do Psychological and Social Factors Influence Medical Illness? Figure 9.2 Psychosocial factors directly affect physical health Definitions of Stress • Stress is: – An environmental condition that may trigger psychopathology – A response to environmental conditions that leads to emotional upset, deteriorating performance or physiological changes • Stressors are stimuli • Cognitive view of stress places emphasis on the interpretation of external stimuli – Coping refers to how people deal with stress Ch 8.2 The General Adaptation Syndrome Ch 8.3 Measuring Stress: Social Readjustment Rating Scale • The Social Readjustment Rating Scale (SRRS) – Rates the stressfulness of various life events. – Initial scale development • Research participants asked to rate various life experiences for stress impact (marriage = 500) • Final version of scale rank orders life events and assigns proportional score to each event. – Total score on the scale is correlated with diseases such as heart attack and leukemia Ch 8.4 Measuring Stress: Assessment of Daily Experience Scale • Assessment of Daily Experience (ADE, Stone & Neale, 1982) – Respondents record and rate their life experiences during each day – Research shows that adverse life events increase prior to an illness Daily Stress & Illness Figure 8.3 Number of desirable events for the ten days preceding an episode of respiratory infection. After Stone, Reed, & Neale, 1987 Figure 8.4 Number of undesirable events in the ten days preceding an episode of respiratory infection. After Stone, Reed, and Neale, 1987 What Influences the Stress Response? – A Sense of Control – Coping Skills – Self-Efficacy – Health and Wellness Behaviors – Social Support – Immune System Functioning Social Support and Stress •Karmarck et al. (1995) studied effect of social support on BP in a laboratory experiment. •Stress led to increases in both diastolic and systolic blood pressure but BP increases were greatest when the research participant was alone. •The stress had less of an impact on BP when participant was accompanied by a friend. Biological Theories of the Stress-Illness Link • • • Somatic-Weakness theory holds that a weak organ system may be susceptible to disruption by stress Specific-Reaction theory suggests that people respond to stress in unique ways, some organ systems show greater reactivity than do other systems Allostatic load (McEwen & Seeman, 1999) – When stressors are acute or occur repeatedly, the biological responses to stress (e.g., cortisol secretion) can an have aversive impact on body. – Over time, stress response itself may overwhelm the system Ch 8.5 Stress and the Immune System Psychological Theories of the Stress-Illness Link • Psychoanalytic view holds that specific conflicts give rise to psychophysiological disorders • Cognitive-Behavioral view proposes that humans have higher cognitive functions which can amplify and extend the duration of arousal of our bodies Ch 8.6 Hypertension • Hypertension is high blood pressure (bp) – Hypertension leads to heart attacks and strokes • Systolic bp is arterial pressure during contraction of the ventricles of the heart • Diastolic bp is arterial pressure during relaxation of the ventricles of the heart – Increased bp is brought on by increased cardiac output (more blood leaving the heart) or by vasoconstriction of the arteries Ch 8.7 Stress and BP • Stressful conditions produce a short-term increase in blood pressure – These increases return to baseline when the stressor is withdrawn • Studies of blood pressure done on ambulatory subjects reveal that anger is most strongly linked to elevated bp – The changes were large in a subset of subjects – Reactivity refers to increased bp and heart rate in response to stress Ch 8.8 Coronary Heart Disease • Coronary Heart Disease refers to – Angina pectoris: periodic chest pains • Reduced oxygen supply to heart – Myocardial infarction: heart attack • Brought on by a cutoff of oxygen to the heart muscle • Risk factors for MI include age, gender (males), elevated blood pressure, elevated cholesterol, obesity, physical inactivity, excessive use of alcohol and diabetes Ch 8.9 Diatheses for Coronary Heart Disease • Psychological diatheses for CHD include: – Type A behavior pattern (time urgency, competitive, aggressive/hostile) – High levels of anger – Cynicism – Type D personality: high levels of anger, anxiety and depression as well as low levels of emotional expression • Biological diatheses: focus is on reactivity Ch 8.10 Asthma • Characteristics: air passages suddenly narrow, breathing becomes hard (wheezy) • Triggered by allergens, pollution, viruses, cold, and emotional states • Dominant Etiologic Factor (Rees, 1964) – Allergic (23%) – Infective (38%) (but 86% had had infection) – Psychological (37%) AIDS • AIDS – Is a fatal disease caused viral infection – Compromises the immune system • AIDS – May arise from irrational and self-defeating behavior – Is treatable, but not presently curable or preventable by medical means – Is preventable by psychological means Ch 8.11 Gender & Health • Mortality rates • • Higher for men at every age Men more likely to die – – • Why differential mortality rates? – – – Hormones may confer protection against life threatening diseases. Men more likely to be Type A which may increase risk of heart disease. • However, recent research indicates that women may be as prone to anger as men. Lifestyle differences such as increased consumption of alcohol. • Lifestyle differences may be narrowing – • • Women drink more alcohol and smoke more than in the past. Morbidity rates – • In auto accidents or by homicide Of cirrhosis, heart & lung disease, lung cancer, & suicide Higher for women • Women more likely to – – Have specific diseases such as diabetes, rheumatoid arthritis, etc. Visit physicians and use prescription drugs Why differential morbidity rates? • • • • • Women live longer and therefore may be more likely to develop diseases associated with aging. Women more likely to visit physicians, therefore increasing the likelihood that the diseases they experience are reported to health tracking agencies. Women experience more stress than men, and rate stress as having a greater impact. MD’s may treat women’s health concerns less seriously than men’s health concerns Lower levels of women’s income seem to play a role as does ethnicity. Research studies on health and stress should include women and men in equal numbers Socioeconomic Status, Ethnicity, & Health • Low SES is associated with higher rates of mortality from all causes • Disease and mortality rates differ by race and ethnicity (perhaps due to association with low SES) • What factors may account for this relationship? – – – – Environmental factors Increased stressors Limited access to health services Unable to afford medical insurance & health care • Biological/genetic differences in incidence of illness may be mediated by behavioral variables (e.g., diet and lifestyle) Therapies for Psychophysiological Disorders • Drug interventions can be used to reduce the physical symptoms brought on by stress • Reduction of anxiety, depression or anger is a key element in the treatment of stress-related disorders – Psychoanalysis: uses free association – Cognitive/behavioral: uses systematic desensitization, in vivo exposure, assertion training Ch 8.12 Treating Hypertension • Non-pharmacological treatments include: – Losing weight – Reducing salt intake – Giving up smoking – Limiting alcohol intake – Getting regular exercise – Relaxation training – Reducing anger Ch 8.13 Psychosocial Link to Disease – AIDS – Cardiovascular Diseases – Cancer – Chronic Pain – Chronic Fatigue Syndrome – Treatment and Outcome The Field of Psychological Oncology – Stress Reduction Prolongs Life – Psychological Factors Influence – Course and Development – Response to Aversive Medical Treatment – Improve Quality of Life – Slow Disease Progression – Psychological Factors are Not Cures! Psychosocial Link to Disease – AIDS – Cardiovascular Diseases – Cancer – Chronic Pain – Chronic Fatigue Syndrome – Treatment and Outcome The Nature of Chronic Pain – $100 Billion Spent on Main Medication in U.S. – Worldwide, 20 Million Tons of Aspirin Two Kinds of Clinical Pain – Acute Pain – Chronic Pain Psychological and Social Dimensions – Pain Severity Does not Predict One’s Reaction – Differences Are Psychological Biological Dimensions – Gate Control Theory – Endogenous Opiods (“Endorphins”) Phantom Limb Pain Psychosocial Link to Disease – AIDS – Cardiovascular Diseases – Cancer – Chronic Pain – Chronic Fatigue Syndrome – Treatment The Nature of Chronic Fatigue – Unexplained Fatigue – Variety of Physical Symptoms – Most Common in Women – Often Debilitating Psychosocial Link to Disease – AIDS –Cardiovascular Diseases – Cancer – Chronic Pain – Chronic Fatigue Syndrome – Treatment and Outcome Available Treatments – Biofeedback – Relaxation Procedures – Hypnosis – Comprehensive Stress Management Obstacles to Treatment – Denial and Noncompliance Prevention Efforts Stress Management • Stress Management is a set of techniques used to cope with stress – Arousal can be reduced through relaxation training or by biofeedback – Cognitive restructuring can be used to alter the thought patterns of a person and to increase their perceived level of control – Behavioral skills training relating to time management and how to prioritize – Train the person in how to alter their environment Ch 8.14 Pain Management • Pain can be modified by – Distraction – Refocusing attention – Lowering anxiety – Effecting a sense of control over pain – Re-labeling the sensation as tickling or numbness – Use of biofeedback • Sensitive instruments that give information about psychophysiological states (e.g., skin temp., muscle tension, EEGs) to increase voluntary control Ch 8.15