Physical Disorders and Health Psychology
advertisement
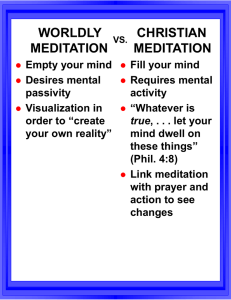
Physical Disorders and Health Psychology Psychological and Social Influences on Health Contribute to top fatal diseases 50% of deaths from 10 leading causes of death in US can be linked to behavior Behavioral medicine Prevention, diagnosis, treatment Interdisciplinary Health psychology Psychological factors important in promotion, maintenance of health Health care policy Ways Psychology Influences Health 1. Affect basic biological process that lead to illness E.g stress and cardiovascular health 2. Influence risky behavior Smoking Alcohol Nutrition Selye’s General Adaptation Syndrome 1. 2. 3. Body’s response to sustained stress Alarm Resistance Exhaustion Stress and the Immune System Early research on stress and cold viruses Psychological impact on immune functioning Depression has a direct effect? Self care and risky behaviors Psychological Effects on Physical Disorders AIDS Cancer Cardiovascular Problems 1. 2. 3. 1. 2. 4. 5. Hypertension Coronary Heart Disease Chronic Pain Chronic Fatigue Syndrome AIDS 40 million worldwide live with AIDS (2003) 20-40% of pop’n in southern Africa Course variable Up to years with no or minor symptoms Median time to full-blown AIDS 7.3-10 years Up to 15% live 5 years or longer Multiple medications 61% of patients discontinue due to side effects AIDS Stress of diagnosis Stress management interventions = less anxiety and depression and increased immune fx Less disease progression 2 year follow-up Ongoing stress CBT can buffer increased viral load Viral load predicts onset of full AIDS Cancer (Psychoncology) Psychological influences on development and course Early research prolonged survival with therapy (Spiegel) 2 times as long as controls at 4 years, 1/3rd tx group alive, no controls Ease of intervention Cancer How do psychological interventions work? Better health habits Closer adherence to treatment Improved endocrine functioning Better response to stress Improved immune functioning Enhanced social adjustment Better coping Cancer Psychological preparation for children Cardiovascular Problems Hypertension Risk for stroke, heart disease, kidney disease Symptoms can be invisible High association with early mortality Blood vessels constrict, heart works harder (wear and tear) Psychological Influences on Hypertension • personality •Coping style • stress levels •Social support •Loneliness, depression •Hostility •Time urgency Coronary Heart Disease Stress, anxiety, anger Poor coping Low social support Stress-reduction programs yield 34% reduction in death from heart attack Type A behavior pattern 2x likely to develop CHD (longitudinally) Coronary Heart Disease and Chronic Negative Emotions Mixed findings Type A Anger responsible for much of effect Measurement Some components, not others Impairs pumping efficiency in lab Associated with artery calcification Time urgency also important Anxiety/depression Depression = 3x likely death after heart attack Chronic Pain Pain as beneficial, motivational $125 billion annually is spent on chronic pain 80% of doctor’s visits due to pain Acute pain Chronic pain Psychological and Social Aspects of Pain Severity of pain does not predict reaction What impacts reaction? Sense of control Can I deal with the pain and it’s consequences? Positive control = less distress, disability Increase concrete coping (e.g., exercise) Depression, anxiety, social support Biological Aspects of Pain Gate Control Theory Nerve impulses from stimuli, to spine, to brain Dorsal horns of spinal column = gate If stimuli intense, gate open and pain signal sent Brain will send signals back to spinal cord, impacting gate Inhibitory or excitatory messages Biological Aspects of Pain Endogenous opiods Shut down pain In presence of injury or tissue damage Sense of control can increase endogenous opiods Chronic Fatigue Syndrome Lack of energy Marked fatigue Aches and pains Low-grade fever No physical pathology was found Neurasthenia (“lack of nerve strength”) Symptoms of Chronic Fatigue Syndrome Medically unexplained fatigue of at least 6 months Of new onset Not from exertion Not alleviated by rest Reduction in previous activity level 4 or more of: Subjective memory impairment Sore throat Tender lymph nodes muscle pain Joint pain Headache Unrefreshing sleep Postexertional malaise Chronic Fatigue Syndrome Often substantial disability Unsure of cause Viruses Immune system dysfunction Depression Toxins Nonspecific response to stress CBT seems relatively effective Psychosocial Treatment for Physical Disorders o o 1. 2. 3. 4. In animal models, pain can = death Stress management often component in medical treatment Biofeedback Relaxation & Meditation Comprehensive Stress & Pain Reduction Program Denial as Coping Biofeedback Patients aware of own bodily functions Blood pressure Brain waves Heart rate Muscle tension 1960s Miller - rats learn to control responses Physiological monitoring makes response visible Biofeedback Work with therapist to change response Success = signal People can control with good accuracy Relaxation and Meditation Progressive muscle relaxation Used in conjuction with other interventions Meditation Transcendental meditation (Focus on mantra) Mindfulness meditation Denial as a Means of Coping Optimism can speed recovery Rapid return to normal activities Better quality of life Less likely to use denial Denial Avoid treatment Not notice changes Denial as a Means of Coping Initial denial of seriousness can be helpful Better endurance shock Decreased time in ICU Modifying Behaviors to Promote Health Remember psychological factors influence health in 2 ways: 1. 2. o 1. 2. 3. 4. Direct effect on biological processes Risky health behavior Four areas of interest: Injury Prevention AIDS Prevention Smoking Stanford Community Study Injury Prevention Leading cause of death aged 1-45 High loss of productivity Prevention in children Escaping fire Reporting emergencies Crossing the street AIDS Prevention Changing behavior only effective prevention Testing does not necessarily change behavior Targeting risky behavioral effective Increase self-efficacy & control Comprehensive Stress- and Pain-Reduction Program Components of stress management Monitor stress and identify stressful events Deep muscle relaxation Appraisals of events Importance Impact Time management Assertiveness training Better than individual components