STAPHYLOCOCCI By - OUR SITE
advertisement

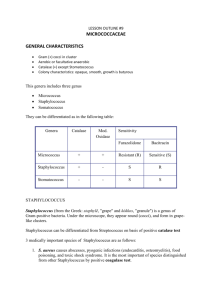
THERE ARE 3 SPECIES: Staph. aureus: pathogenic and is responsible for most of the Staphylococcal infections. Staph. epidermidis: members of the normal flora of skin and mucous membranes and can cause disease. Staph. saprophyticus: non-pathogenic S. AUREUS CAUSES Boils, styes , frunculosis , pneumonia, mastitis, phlebitis, meningitis, urinary tract infections , bacteremia , osteomyelitis and endocarditis . Toxigenic diseases in humans as Scalded skin syndrome in neonates (exfoliative toxin) and food poisoning (enterotoxins) . Samples: differ according to the clinical site of infection, may be swabs ,pus, sputum, C.S.F, blood , urine ,…….) , SAMPLES WILL BE EXAMINED BY : 1.Direct film Stained with Gram stain for characteristic morphology, but we cannot differentiate between S.aureus and other staphylococci on smears . S.aureus is Gram positive cocci arranged in clusters (The clusters arise because staphylococci divide in two planes), non spore forming and non motile. Staphylococci in pus Staphylococci in culture . Gram stain of Staphylococcus aureus in pus 2. CULTURE Staphylococci are facultative anaerobes, optimum temperature: 37C. It can grow in normal atmospheric Co2 concentration. Staphylococci can be grown on ordinary media On blood agar S. aureus cause hemolysis . S. aureus can grow on mannitol salt agar producing (yellow colonies).which is selective for its isolation , as S.aureus but not other staphylococci ferment mannitol and salt inhibits other normal flora but not S.aureus S. aureus produce golden yellow endopigments. GOLDEN YELLOW ENDOPIGMENTS. STAPHYLOCOCCUS AUREUS ON BLOOD AGAR 3. IDENTIFICATION OF COLONIES BY : a. Film stained by Gram for characteristic morphology . b. Biochemical reactions : All staphylococci are catalase positive. (This test differentiate staphylococci from streptococci which are catalase negative) . S. aureus can be identified by being coagulase and DNAase positive ,and by mannitol fermentation. CATALASE TEST: Use: The test is used to differentiate those bacteria that produce the enzyme catalase, such as Staphylococci, from non catalase producing bacteria such as Streptococci. Principle: the test is based on that some organisms produce catalase enzyme. Catalase acts as a catalyst in the breakdown of hydrogen peroxide to oxygen and water. CATALASE TEST: Method: Few drops of 3% hydrogen peroxide solution, are placed on a clean glass slide; a good growth of the organism is removed and immersed in the hydrogen peroxide solution. The culture should not be more than 24 hours old and from a blood-free culture medium such as nutrient agar. Interpretation: Immediate bubbling indicates positive results. CATALASE TEST: COAGULASE TEST: Use: The test is used to differentiate Staphylococcus aureus that produce the enzyme coagulase, from non coagulase producing bacteria such as S. epidermidis and S. saprophyticus. Principle: Coagulase causes plasma to clot by converting fibrinogen to fibrin. COAGULASE TEST: Two types of Coagulase are produced by most strains of Staph aureus : Free coagulase which converts fibrinogen to fibrin by activating a coagulase reacting factor present in plasma. Free coagulase is detected by the appearance of a fibrin clot in the tube test. Bound coagulase (clumping factor) which converts fibrinogen directly to fibrin without requiring a coagulase reacting factor. It can be detected by the clumping of bacterial cells in the rapid slide test. COAGULASE TEST: Slide coagulase test (to detect bound coagulase): a colony of the test organism is emulsified in a drop of physiological saline on a slide. A drop of plasma is added and mixed gently. Interpretation: Clumping of the organism within 10 seconds denotes positive results. COAGULASE TEST: Tube test (to detect free coagulase): 0.5 ml of the diluted plasma is pipetted into tube. 5 drops of the suspention of test organism is added to the plasma in the tube. The tube is mixed gently, incubated at 3537˚C. The tube is examined after 1 hour. If no clotting occurred, the tube is examined at 30 minute intervals for up to 6 hours. During examining the tube for clotting tilt the tube gently. COAGULASE TEST: Interpretation of tube test: positive result is indicated by the presence of fibrin clot. S. aureus strains produce fibrin clot within 1 hour of incubation. POSITIVE TUBE COAGULASE TEST DNASE AGAR Use: This test is used to differentiate S. aureus which produce the enzyme DNAase from other staphylococci which don’t produce the enzyme DNAase. It is particularly useful if plasma is not available to perform coagulase test or when the results of coagulase test are difficult to interpret. Principle: Deoxyribonuclease enzyme hydrolyses deoxyribonucleic acid (DNA) DNASE AGAR Method: The test organism is cultured on medium containing DNA(DNAase agar ) , after incubation at 37˚C for 1824 hours ,then the plate is flooded with a few millimeters of 1 mol/liter (3.6%) hydrochloric acid to precipitate unhydrolysed DNA. After standing few minutes the plate is examined against a dark background. Interpretation: Clear zone around spot culture is detected in case of positive result. DNase positive breakdown of the DNA in the agar. There is a clear zone (arrow) around the bacterial growth where there is no longer any DNA left in the agar to precipitate out of solution after the HCl was added. ANTIMICROBIAL SUSCEPTIBILITY Staphylococcal isolates should be tested to antimicrobial susceptibility to select the effective drug . NOVOBIOCIN SENSITIVITY TEST Principle: It is done to differentiate between the coagulase negative Staphylococci Method: The test is done by placing a filter paper disc impregnated with novobiocin on the surface of the culture plate after inoculating it with the organism A zone of inhibition of growth occurs around the disc if the organism is Staph. epidermidis No zone of inhibition of growth occurs if the organism is Staph. saprophyticus DIAGNOSIS OF STAPHYLOCOCCAL FOOD POISONING: The food remnants, vomitus and stools are cultured on mannitol-salt agar and the isolated staphylococci are identified by their biochemical activities, catalase, coagulase and DNase production. To trace the source of contamination of food, the food handlers are tested for the possibility of being nasal or skin carriers of strains belonging to the same phage type as the strain causing food poisoning. PHAGE TYPING: 1-Plates are inoculated with the test strain, and dried. 2-A drop of each phage is placed in a marked square area. 3-After incubation, lysis will occur in the areas of the corresponding phage type. PHAGE TYPING • • Aerobe Eukaryotic cells • 25 – 30ºC • 37ºC Saprophyte • Opportunistic - 1ry pathogen Shape Moulds ? Filaments Yeast-like - Candida - Cryptococcus NonSeptated septated Hyaline Yeast ? Brown Dimorphic -Histoplasma -Sporotrichosis Fungal Diagnosis Sample: •It's advisable to collect as much material as possible due to scaricity of many fungi in many specimens. •The type of the sample collected is determined according to the suspected site of infection such as:-skin scrapping – nail clipping – hair epilation – sputum – blood, c.s.f. Storage and transport: Skin, nail and hair: They are collected in air-tight containers such as small glass bottles. The fungi in test samples can remain viable for weeks or even months. They shouldn't be refergirated as the viability of some species of dermatophytes is affected. Other specimens should be collected, stored and transported in a manner similar to that employed for bacteriological investigation. If specific fungus is suspected, the lab should be notified as special media and culture procedures may be needed and that also will be helpful for the safety of lab personnel. Direct Ex.: Value: • Guide for Culture •Sometimes diagnositics 1- Unstained: - KOH - India ink 2- Stained: • Gram stain • Calcofluor white: fluor. M. • Giemsa: intracellular • PAS, GMS: in tissue Culture: Culture Chs.: • O2: • Temp.: Media: • SDA • Cyclohexamide ‘Actidion’ <> Saprophytes For isolation of ? • Chloramphenicol / Gentamicin <> Bacteria - Enriched: Dimorphic f. Colony identification: • Chs - Size, shape, recto-verso, texture • Stained film • BRs: - Sugar ferm. - Urease test Antigen detection: Ag as beta-glucan candida Serology: Antibodies / limited / Candida, Cryptococcus / ELISA Histopathology: Yeast cells, granules Molecular: PCR, probe Skin test: ? No diff. () active , past / Candidin Wood’s light: UV Hair, skin / not all fungi / if –ve ? Animal inoculation: Identification of Candida albicans:- The colony appears as a rounded white creamy in colour and creamy in texture. Film stained by lactophenol blue show budding yeast and filaments (pseudo-mycelium). If stained by Gram stain appear Gram positive. Germ tube test : culture of the yeast on serum causes rapid formation of filaments when incubated at 37°C for 4 hours. Fermentation of sugars.