S. aureus - logan2014
advertisement

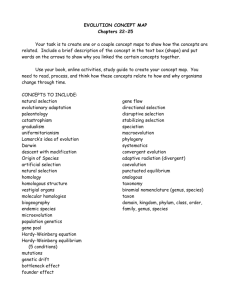
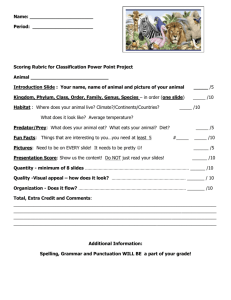
Microbiology II Final Lab Exam Study Guide The introduction and observation sections of Genus Streptococcus o The genus Streptococci contains a variety of species that will cause disease in humans. The group contains Gram positive cocci that occur in pairs or chains. They are a non-motile, non spore-forming group of bacteria that are negative for catalase production and typically attack media containing red blood cells. Most members are facultative anaerobes, although some members are strict anaerobes. They are fastidious in their nutritional demands and require a variety of substances that must be added to the medium in order to support growth. There have been several attempts to devise a classification scheme for the genus, but the method that is widely accepted was proposed in the early 1930s by Rebecca Lancefield. It is a serological classification based on serologic differences in an extractable carbohydrate in the cell walls of members of this genus. The five serological groups Lancefield identified are called A, B, C, D, and E. Additional groups have since been identified and the number is presently at >18. Group A is the most pathogenic group containing Streptococcus pyogenes, which is the causal agent of strep throat, as well as, erysipelas, impetigo, scarlet and rheumatic fever, glomerulonephritis, and necrotizing fasciaitis. Streptococcus pneumoniae is also a member of Group A. It is an encapsulated bacterium that causes lobar pneumonia, but also causes otitis media, sinusitis, meningitis, bacteremia, and endocarditis. The capsule has been shown to be an important virulence factor. Serologic identification of S. pneumoniae is enhanced because of the variety of capsular types. At present, there are more than 80 different types because of the differences in polysaccharide components in the capsule. Certain serotypes are epidemiologically important, whereas others are rarely associated with disease. Virulent strains produce moist, mucoid colonies because of the capsule, whereas nonencapsulated strains produce a translucent colony that is initially convex. With time the colony develops a central depression, a useful identification characteristic. Microscopically, pneumococci are lancetshaped coccoidal cells that appear as Gram-positive diplococci but sometimes develop into short, tight chains or singly.Group B contains the species Streptococcus agalactiae, which causes neonatal sepsis, pneumonia, and meningitis.Group D houses Streptococcus faecalis, which causes urinary tract infections.Streptococcus species are commonly found in the naso- and oropharyngeal cavity. Since there are many other bacteria found there also, it is important to have methods to distinguish between them. o Important characteristics of this genus are: Cell and colony morphology Hemolysis on blood agar Bacitracin susceptibility Growth in 6.5% NaCl Test Hemolytic type Bacitracin susceptibility Growth in methylene blue milk Esculin hydrolysis S. pyogenes Beta S. agalactiae Beta + - S. faecalis Alpha or Gamma - S. pneumoniae Alpha + The introduction and observation sections of Family Enterobacteriaceae o The enterics are an important group of Gram negative, non-sporeforming bacilli. They inhabit the intestinal tract of man and belong to the family Enterobacteriaceae. This is a large group of bacteria and is composed of a significant number of important species. Members of this family are often referred to as coliforms. More frequently, however, the term is used to describe only the fermentative inhabitants of the intestinal tract such as Escherichia coli, Klebsiella pneumoniae, and Enterobacter aerogenes. This group is known to contain species that cause a variety of infectious diseases, including typhoid fever, bacillary dysentery, diarrheal disease, bacteremia, meningitis, urinary tract infections, respiratory infections, and wound infections. In addition to the many pathogens in this family there are also a number of commensals in the group that can produce disease in the compromised patient. Patients with underlying disease or those who are immunosuppressed are particularly susceptible to the enterics. This family is responsible for 50% of nosocomial infections, most frequently caused by E. coli, Klebsiella, Enterobacter, Proteus, Providencia, and Serratia marcescens. The microbes of this family are distributed worldwide. They are found in soil, water, fruits, vegetables, grains, flowering plants and trees, and animals from worms and insects to humans. Escherichia coli is the most common facultative inhabitant of the intestine measuring 107-108 per gram of feces.Because the family contains so many important disease-producing genera, it is the most frequently encountered group of bacteria in the clinical laboratory. Although they are normal inhabitants of the intestinal tract, they may be found in other clinical specimens such as blood and sputum. Although major characteristics separate individual species, they have many characteristics in common such as the ability to produce catalase of ferment glucose. Most are motile. Most laboratories have definite steps that are followed to identify an isolate. These steps are usually directed at showing Salmonella or Shigella to be the cause of the patient’s disease. As suggested, however, many other genera in the family may be involved. Perhaps the most important characteristics used to separate Salmonella and Shigella from the others is lactose utilization. These genera give a negative reaction while other enterics usually give a positive reaction. Escherichia and Enterobacter give a strong positive reaction, but Proteus is negative and is sometimes confused with the non-lactose fermenters. o Clinical specimens that are to be analyzed for enterics are usually taken through a series of procedures intended to aid identification as shown in the following table. Steps in the Identification of Enterics 1. Inoculate enrichment broth 2. Inoculate differential/selective media 3. Inoculate TSI agar 4. Determine biochemical reactions 5. Determine serological properties The specific characteristics that follow should be used in the identification of Enterobacteriaceae. Cell and colony morphology Motility Fermentative metabolism Glucose utilization Ornithine decarboxylation Oxidase reaction Nitrate reduction End-product identification Unfortunately, there is no single morphological or biochemical characteristic that can be used to distinguish individual members. Differential and selective plating media are useful for distinguishing particular microorganisms from others. Selective media allow growth of only one group while differential media allow growth of several groups but particular properties of the organism can be distinguished from others. Occasionally a single medium may have both selective and differential properties. The clinical microbiologist may want additional information concerning the biochemistry of an isolate. For that reason, there are numerous media and reagents in self-contained testing systems that give biochemical profiles of the microorganism in question. With the use of identification charts, results provide the name of the isolate. The following table contains information that will be useful for identification of the species under study. Test E. coli S. typhi S. dysenteriae K. pneumoniae TSI-slant + + TSI-H2S +/- (don’t production study, it’s variable) TSI-gas +/- (don’t +/- (don’t + production study it’s study it’s variable) variable) Simmons + + Citrate Motility + + - - Know the steps necessary to identify an unknown. What is the first step? o First step in identifying an unknown Prepare a smear for staining. Perform a Gram stain and note the reaction and morphology. From these determinations, decide what media and/or biochemical tests will be necessary to continue your identification. Introduction and observation sections of Staphyloslide o The Staphyloslide Latex test is an agglutination test for the differentiation of staphylococci which possess clumping factor and/or Protein A, usually present with Staphylococcus aureus, from staphylococci that do not possess these properties. Approximately 97% of human strains of S. aureus possess bound coagulase. This is evident by coagulase testing that detects clumping/clotting factor (bound coagulase) on the bacterial cell surface. Protein A is found on the cell surface of about 95% of human strains of S. aureus and has the ability to bind the Fc portion of immunoglobulin G.The Staphyloslide Latex test consists of blue latex particles coated with human fibrinogen and IgG. On mixing the latex reagent with staphylococci colonies that possess Protein A or bound coagulase, cross linking will occur causing an agglutination reaction. This occurs most notably with S. aureus. If neither bound coagulase nor Protein A are present, no agglutination will occur and the result will be negative. This occurs most frequently with Staphylococcus epidermidis. o PAY ATTENTION TO WHAT MAKES THEM POS AND NEG o Positive Result: A positive result is obtained if agglutination or the blue latex particles occurs within 20 sec in the test circle, with no agglutination in the control circle. The result is positive when there is noticeable clearing of the blue background in the test latex. This indicates the presence of S. aureus. o Negative Result: A negative result is obtained if no agglutination occurs and a smooth suspension remains at 20 sec in the test circle. The result is negative when there is no noticeable clearing of the blue background in the test latex. *Reactions occurring after 20 sec should be ignored. o Staph Aureus was positive o Staph Epidermidis was negative Introduction and observation sections of PYR Dry Slide o The DrySlide is used for detecting hydrolysis of L-pyrrolidonyl-βnaphthylamide (PYR). This indicates the presence of the enzyme pyrrolidonyl peptidase. This is a test for rapid presumptive identification of A streptococci and group D enterococci. 98% of group A and 96% of group D streptococci hydrolyze PYR. Nearly 100% of all other groups and species of streptococci yield a negative PYR test result. While this test may be used as a presumptive diagnostic aid for identifying these organisms, additional biochemical and serological tests should be performed for complete identification. o Positive Result: PYR positive organisms change the color of the reaction area from pale yellow to pink/fuchsia within 1 minute of adding the color developer. This indicates the presence of either a Group A or Group D streptococcus species.*Some streptococcal strains produce only a small amount of enzyme, so the color change is weak. A weak positive reaction can be enhanced by allowing the test organism to incubate 5 minutes rather than 2 minutes at room temperature before adding the color developer. (HE SAID PAY ATTENTION TO THIS PARAGRAPH) o Negative Result: A negative result is obtained if no color change from yellow occurs upon addition of the color developer within 1 minute. o S. pyogenes was positive o S. agalactiae was negative Be able to tell me how you inoculated the enterotube, how long it was incubated, and how you found out what organism you had. o Inoculation of Enterotube by first twisting the wire, then withdrawing it through all twelve compartments using a turning motion. o Reinsert wire into Enterotube using a turning motion through all twelve compartments, until the notch on the wire is aligned with the opening of the tube. The tip of the wire should be visible in the citrate compartment. Break the wire at the notch by bending. o Punch holes with the broken off part of the wire through the foil covering the air inlets of the last eight compartments (adonitol, lactose, arabinose, sorbitol, Voges-Proskauer, dulcitol/PA, urea, and citrate) in order to support aerobic growth in these compartments. Replace both caps. o Incubate at 37oC for 24 hours with Enterotube lying on its flat surface. o Indicate each positive test reaction by circling the number appearing below the appropriate compartment on the Results Pad. o Add the circled numbers in the bracketed section and enter the sum in the space provided below the arrow. o Locate the five-digit number in the CCIS and find the best answer in the column entitled “ID Value”. NOTE: Should more than one organism be listed, the confirmatory test required to correctly identify the organism will be indicated in the CCIS. Introduction and observations of the Genus Staphylococcus o The genus Staphylococcus is one of the most important members of the family Micrococcaceae, which also includes Streptococcus and Micrococcus. The staphylococci are a medically significant genus in that Staphylococcus aureus is the number one causative organism for skin abscesses. Furthermore, species from this genus are known to cause cellulitis, impetigo, bacteremia, endocarditis, brain abscesses, osteomyelitis, urinary tract infection, toxic shock syndrome, scalded skin syndrome, and food poisoning. The staphylococci are Gram-positive cocci occurring singly, in pairs, and irregular clusters. They are facultative anaerobes with both oxidative and fermentative metabolism. Colonies are usually opaque and may be white or cream and sometimes yellow to orange. They are usually catalase positive; nitrate is often reduced to nitrite, and grows well at high osmotic pressures (20% NaCl). There are specific methods, which are used to separate the staphylococci from other Gram-positive cocci as well as methods that are used to distinguish each species of the genus. Important characteristics that are used to identify these microorganisms are listed below: 1. Cell and colony morphology 2. Growth on Mannitol Salt Agar 3. Pigment production 4. Hemolysis on Blood agar 5. Catalase production 6. DNAse production 7. Coagulase production 8. Novobiocin resistance 9. Fermentation of mannitol Nitrate reduction Hemolytic type DNAse production Novobiocin resistance S. aureus + Beta + - S. epidermidis Variable (don’t study) Gamma - S. saprophyticus Gamma +