Arizona Program of Applied Geriatrics: The Role of the
advertisement

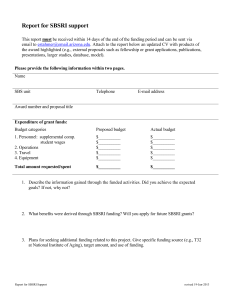
Arizona Program of Applied Geriatrics: The Role of the Informationist Carol Howe, MD, MLS: Librarian Sandra Kramer, MA, MS: Assistant Director for Services 1 College of Medicine (COM) and the Donald W. Reynolds Foundation In 2006 the COM of the Arizona Health Sciences Center (AHSC) was one of 10 academic centers chosen to receive an almost $2 million dollar grant in the third phase of the Reynolds Aging and Quality of Life Program. 2 The Aging and Quality of Life Program was established in 1996 by the Donald W. Reynolds foundation to revolutionize geriatric training within our medical centers in order to meet the complex needs of the ever-expanding population of elders in the United States From the Administration on Aging’s “A Profile of Older Americans : 2004” 3 So far, three cohorts of ten medical centers each have been awarded 4-year, approximately $2-million grants. 4 Each center has, or is in the process of, developing a unique approach to integrating geriatric awareness and expertise at every level of medical training and practice. 5 An annual meeting is held where all the Reynolds programs convene and exchange resources, ideas and educational products that they have developed or are working on. 6 Examples of innovative ideas that have emerged so far include: Geriatric Quick Consult Web site for students and clinicians --Virginia Commonwealth University A Chief Resident Immersion Training Program -Boston University CHAMP-Curriculum for the Hospitalized Aging Medical Patient—University of Chicago Focus on training primary care physicians – University of Utah 7 8 Reynolds Scholars in Aging Program Considered the “Key Driver” Based on principle that non-geriatrician physician leaders within both primary and specialty fields will become true agents of change when they themselves receive intensive training in the principles of geriatrics 9 The Informationist One of the unique features of the Arizona Reynolds Program is the inclusion of an informationist to participate at every level of the program. “The Librarian” a 1556 painting by Giuseppe Arcimboldo From Wikipedia.org 10 In their groundbreaking 2000 editorial in the Annals of Internal Medicine, Davidoff and Florance proposed the establishment of a “new health profession,” that of the informationist. With a “clear and solid understanding of both information science and the essentials of clinical work,”1 the informationist is poised to bridge the gap “between the huge body of information hidden away in the medical literature and the information needed at the point of care.”2 1- Davidoff F and Florance V. The informationist: a new health profession? Ann Intern Med. 2000 Jun 20; 132 (12):997. 2-Davidoff F and Florance V. The informationist: a new health profession? Ann Intern Med. 2000 Jun 20; 132 (12):996. 11 Informationist as Team Member Offers research support to Medical students Residents Fellows Faculty Members 12 Tied in to day to day information needs Attends weekly leadership meetings Answers reference questions as they arise Locates hard to find documents Composes bibliographies Contributes to Consumer Newsletters Contributes to Professional Journals (such as the Journal of the Arizona Geriatrics Society) 13 Most vital role, however, is with the Reynolds Scholar in Aging Program (RSIA) William Hogarth 's 1736 engraving, Scholars at a Lecture 14 Who are the scholars? Dr. C.C.: Associate Professor of Surgery/Urology; Chief of the Section of Urology; Residency Director. Dr. H.V., Professor of Surgery and Interim Head of the Department of Surgery Dr. W.G., Professor of Orthopedics and Head of Department of Orthopedics Dr. S.B., Professor of Anesthesiology and Head, Department of Anesthesiology Dr. G.W.: Associate Professor of Clinical Medicine-- actively involved in developing the new curriculum. Dr. H.M. Professor of Emergency Medicine; Department Head for Emergency Medicine; Director of the Arizona Emergency Medicine Research Center Dr. J.W.: Associate Professor, Department of Surgery; Residency Director. Dr. P. L.: Associate Professor, Clinical Family & Community Medicine; Program Director for the Family Medicine Residency--also completed a fellowship in Integrative Medicine in 2005. Dr. R.M.: Associate Professor, Clinical Medicine; Program Director for the Internal Medicine Residency Program; Section Head for the Medical Education Office; chair of the Graduate Medical Education Committee. Dr. S.C :Professor, Gynecologic Oncology; Director of Women’s Cancers, Arizona Cancer Center; Associate Head for Academic Affairs, Department of OB/GYN. Dr. J.U.: Hospitalist and Division Chair, Department of Medicine at the Southern Arizona Veterans Administration Health Care System 15 In addition to university-bases Scholars in Aging, physicians are also chosen from Indian Health Service (IHS) and tribal medical facilities. Whiteriver IHS Hospital Hopi Health Care Center 16 17 Reynolds Scholars in Aging: The Program 1. 2. Intensive training in basic principles of geriatric care with particular attention to how it relates to their individual specialties. Collaboration between scholar and mentor (physician with additional training and certification in geriatrics). The scholar and mentor team in turn work closely with the informationist. 18 3. 4. 5. Development of Reynolds Care in Aging (CAPstone) Project-in which each scholar develops a research question that addresses and contributes to the solution of a real world problem. Integration of geriatric themes into the physicianscholars’ teaching at every level—from undergraduate medical student to colleagues at international conferences. Generation of Scholarly Activity- such as lectures, publications and abstracts in an aging-related aspect of the individual scholar’s field. 19 The Scholars and the Informationist The informationist is available to assist the scholars with any and all of the above. 20 One of the most unique features of the informationist's role in the Scholar in Aging Program, however, is the “Question of the Month” 21 In collaboration with their mentors, scholars compose queries which run the full range from very specific, technical, medical questions to very broad cultural/ethical/philosophical questions. 22 Examples of focused medical questions: In PICO format: in older adults who have been vaccinated for zoster, compared with similar adults who have not been so vaccinated, what is the event rate of herpes zoster? What are causes of persistently elevated d dimers in older patients with recurring clots (PE/DVT etc)? 23 Examples of broader medical questions: How does treatment of ovarian cancer differ between younger and older women? What is the evaluation and management of hypogonadism in elderly men? What tools, if any, are validated for comprehensive evaluation of the older adult (>65) with cancer to determine his/her ability to tolerate chemotherapy? 24 Example of broader systems-type questions: What is known about creating an effective ED Emergency Department] care environment for elder care (from first responders, through discharge)-- in terms of obtaining adequate data, maximizing communication, supporting sensory deficits, configuring the physical environment to optimize functioning, incorporating safety features, enabling efficient care for providers, and providing transitional data to discharge environment? 25 Example of a question embedded in a case scenario: Older male from NH [nursing home] with advanced dementia admitted to hospital as full code. No MPOA, [medical power of attorney] no relatives, no guardian per records from NH. His wishes are unobtainable given current dementia or perhaps co-existing delirium due to acute illness – i.e., he is oriented only to self. He has progressive respiratory failure and team forced to make decision to intubate/send to ICU or no. Given current legal climate in US, team decides to send to ICU, is intubated, and eventually dies while in ICU. [Physician] wonders if there is any literature to support not sending him to the ICU - could he have decided on hospice or similar using ethics committee - or any recommendations on this topic in the geriatric literature? 26 Examples of questions in which cultural context plays a major role: Are there references for discussing or implementing code status (do not resuscitate/allow natural death) in Navajo or Hopi communities? (see appendix) What is known about depression among American Indian/ Apache and/or Navajo? Or other tribes? In terms of epidemiology and risk factors, clinical presentation, effects of treatments? 27 After receiving a question, the informationist Conducts a search in PubMed Looks at many of the evidence based databases such as Cochrane Database of Systematic Reviews Database of Abstracts of Reviews of Effectiveness (DARE) ACP Journal Club Up to Date Our own AHSL custom search engine 28 The informationist then summarizes and synthesizes a response. 29 An annotated bibliography with links to full text is appended to the response and submitted to the mentor/scholar team References Balducci, L., & Extermann, M. (2000). Management of cancer in the older person: A practical approach. The oncologist, 5(3), 224-237. The management of cancer in the older aged person is an increasingly common problem. The questions arising from this problem are: Is the patient going to die with cancer or of cancer? Is the patient able to tolerate the stress of antineoplastic therapy? Is the treatment producing more benefits than harm? ….. Chen, C. C., Kenefick, A. L., Tang, S. T., & McCorkle, R. (2004). Utilization of comprehensive geriatric assessment in cancer patients. Critical reviews in oncology/hematology, 49(1), 53-67. A growing and diverse aging population, recent advances in research on aging and cancer, and the fact that a disproportional burden of cancer still occurs in people aged 65 years and older have generated great interest … articles were identified through the bibliography of relevant articles. Extermann, M. (2003). Comprehensive geriatric assessment basics for the cancer professional. The Journal of oncology management : the official journal of the American College of Oncology Administrators, 12(2), 13-17. A comprehensive geriatric assessment (CGA) has been a cornerstone of geriatric practice for many years. However, oncology practitioners are still unfamiliar with it. Yet, recent …… Extermann, M. (2003). Studies of comprehensive geriatric assessment in patients with cancer. Cancer control : journal of the Moffitt Cancer Center, 10(6), 463-468. BACKGROUND: The comprehensive geriatric assessment (CGA) has been developed to individually assess the health status of older patients. METHODS: This article reviews the findings ….pact on patients with this disease. CONCLUSIONS: More work is needed to simplify such assessments to make them more feasible and to determine when they should be used during a patient's clinical course. Fosser, V. (2002). Multidimensional evaluation in geriatric oncology: The reasons "contra". Tumori, 88(1 Suppl 1), S103-4; discussion S105. Friedrich, C., Kolb, G., Wedding, U., Pientka, L., & Interdisziplinare Arbeitsgruppe der DGHO/DGG. (2003). Comprehensive geriatric assessment in the elderly cancer patient. Onkologie, 26(4), 355-360. The proportion of older cancer patients is increasing due to demographic and disease-specific reasons., as CGA has also a key role in the decision process…. 30 The teams are invited to submit further clarifying questions and also to evaluate the usefulness of the response. 31 Through this process, we hope to achieve the goal, articulated in the original Arizona Reynolds Program Summary, of providing evidence based material in response to clinical questions.This inquiry process is important because it… 32 1. 2. 3. Provides a real ‘needs assessment’ from which the curriculum can be modified Builds an evidence-based library within each specialty Can be the basis for extension of academic activities, such as lectures, web-based training, case-based training or journal articles 33 The responses will form the basis of a regular feature in the Arizona Geriatrics Society Journal 34 There will also be a “Question of the Month” feature on the Web Site of the Arizona Reynolds Program of Applied Geriatrics 35 As our program progresses we are realizing that not only is there a gap between the vast stores of information available and actual medical practice at the bedside, but equally vast gaps between information that is needed at the bedside and available information. 36 Particularly in geriatrics, there simply are not conclusive evidence-based answers to many of the questions that clinicians are asking. 37 It is our hope, therefore, that through the collaboration of the Arizona Health Sciences Library and the Arizona Reynolds Program of Applied Geriatrics we will be able to positively influence not only the practice patterns of physicians caring for older individuals, but the nature and structure of the research and clinical studies upon which those thought and practice patterns ultimately depend. 38 References Arizona Reynolds Program of Applied Geriatrics: Program Summary (2006) (internal document). Davidoff, F. & Florance, V. (2000). The Informationist: A New Health Profession? Annals of Internal Medicine 132(12) 996-998. 39 The Arizona Reynolds Program of Applied Geriatrics is Funded by the Donald W. Reynolds Foundation through its Aging and Quality of Life Program. The goal of the program is to improve the quality of life for America’s elderly by preparing physicians to provide better care for them when they become ill. The Donald W. Reynolds Foundation is a national philanthropic organization founded in 1954 by the late media entrepreneur for whom it is named. Headquartered in Las Vegas, Nevada, it is one of the largest private foundations in the United States. 40