Lecture 1: Introduction to Pharmacology
advertisement

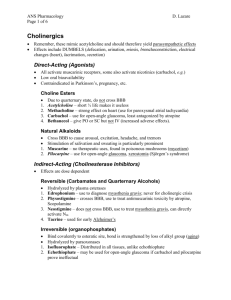
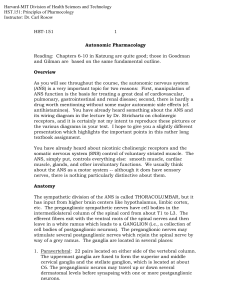
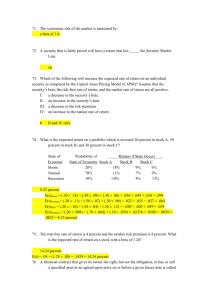
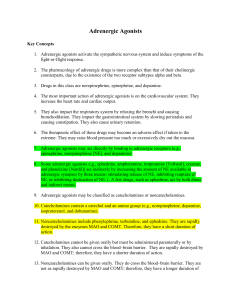
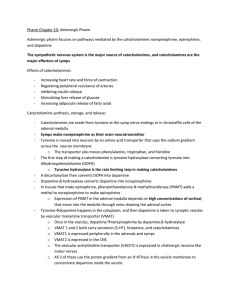
Drugs Affecting the Autonomic Nervous System Pharmacology 49.222 Bill Diehl-Jones RN, PhD Faculty of Nursing and Department of Zoology Agenda • • • • • • A Zen Review Overview of CNS and ANS Neurotransmitters and 2nd Messengers Cholinergic Agonists and Antagonists Adrenergic Agonists and Antagonists Movement Disorder Drugs Organization of the Nervous System: CNS • Three divisions of brain: – Forebrain • cerebral hemispheres – Midbrain • Corpora quadrigemini, tegmentum, cerebral peduncles – Hindbrain • Cerebellum, pons, medulla • Brainstem: – Midbrain, medulla, pons – Connects cerebrum, cerebeluum, spinal cord Organization of the Nervous System: Reticular Activating System • Key Regulatory Functions: Radiation Fibres – CV, respiratory systems – Wakefulness • Clinical Link: Thalamus – Disturbances in the RAS are linked to sleep-wake Visual Inputs Reticular Formation disturbances Ascending Sensory Tracts Organization of the Peripheral Nervous System • Three major divisions: – Efferent • Somatic (motor) • Autonomic – Sympathetic and Parasympathetic – Afferent • Sensory Some Basic Plumbing: The Peripheral Nervous System Parasympathetic Sensory Sympathetic Motor Parasympathetic Preganglionic Nerves Sympathetic Parasympathetic Sympathetic AND Parasympathetic preganglionic fibres release Acetylcholine (ACh) ACh has two types of receptors: Muscarinic and Nicotinic Postganglionic nerves have Nicotinic receptors ACh Postganglionic Nerves Sympathetic Parasympathetic • Sympathetics release Norepinephrine • Parasympathetics release ACh • Norepinephrine binds to adrenergic receptors ACh • ACh binds to Muscarinic receptors NE What Happens at the Effectors? • NE from postganglionic sympathetics binds to Adrenergic Receptors • ACh from postganglionic parasympathetics binds to Muscarinic Receptors NE ACh Adrenergic Receptor Muscarinic Receptor Sympathetic Parasympathetic Cholinergic Neurons Na+ Choline Acetylation Ca++ Acetylcholinesterase Receptor Cholinergic Receptors • Muscarinic receptors come in 5 flavours – M1, M2, M3, M4, M5 – Found in different locations – Research is on-going to identify specific agonists and antagonists • Nicotinic receptors come in 1 flavour Cholinergic Agonists • • • • Acetylcholine Bethanechol Carbachol Pilocarpine General Effects of Cholinergic Agonists • Decrease heart rate and cardiac output • Decrease blood pressure • Increases GI motility and secretion • Pupillary constriction Cholinergic Antagonists • Antimuscarinic agents – Atropine, ipratropium • Ganglion blockers – nicotine • Neuromuscular blockers – Vecuronium, tubocuarine, pancuronium Where are some of these drugs used? Atropine (a cholinergic antagonist) • Comes from Belladonna – High affinity for muscarinic receptors – Causes “mydriasis” (dilation of the pupil) and “cycloplegia” • Useful for eye exams, tmt of organophosphate poisoning, antisecretory effects • Side effects? Scopalamine (also a cholinergic antagonist) • Also from Belladonna • Peripheral effects similar to atropine • More CNS effects: – Anti-motion sickness – amnesiac Trimethaphan (yet another cholinergic antagonist) • Competitive nicotinic ganglion blocker • Used to lower blood pressure in emergencies Neuromuscular Blockers • Look like acetylcholine • Either work as antagonists or agonists • Two flavours: – Non-depolarizing (antagonist) • Eg: tubocurarine • Block ion channels at motor end plate – Depolarizing (agonist) • Eg: succinylcholine • Activates receptor Turbocurarine • Used during surgery to relax muscles – Increase safety of anaesthetics ACh Curare • Do not cross bloodNicotinic Receptor brain barrier Na+ Na+ Channel Succinylcholine • Uses: – endotracheal intubations • What is this? • Why? Na+ - - - - - - + ++ + + + + Phase I – electroconvulsive shock therapy Na+ • Problem: can cause apnea ++ + - - - ++ + - - Phase II Adrenergic Neurons Na+ Tyrosine Dopa MAO Ca++ Dopamine Dopamine is converted to epinephrine Receptor Word of the Day: • SYMPATHOMIMETIC – Adrenergic drug which acts directly on adrenergic receptor, activating it Adrenergic Agonists • Direct – – – – Albuterol Dobutamine Dopamine Isoproteranol • Indirect – Amphetamine • Mixed – Ephidrine Adrenergic Receptors • Two Families: – Alpha and Beta – Based on affinity to adrenergic agonists Epinephrine Norepinephrine Isoproteranol Epinephrine Isoproteranol • Alpha affinity: • epinephrine≥norepinephrine>> isoproteranol • Beta affinity: • Isoproteranol>epinephrine> norepinephrine Norepinephrine What do these receptors do? • Alpha 1 – Vasoconstriction, ↑ BP, ↑ tonus sphincter muscles • Alpha 2 – Inhibit norepinephrine, insulin release • Beta 1 – Tachycardia, ↑ lipolysis, ↑ myocardial contractility • Beta 2 – Vasodilation, bronchodilation, ↓insulin release Adrenergic Angonists • Direct acting: – Epinephrine: interacts with both alpha and beta • Low dose: mainly beta effects (vasodilation) • High dose: alpha effects (vasoconstriction) • Therapeutic uses: emerg tmt of asthma, glaucoma, anaphyslaxis – (what about terbutaline?) Adrenergic Agonists • Indirect: – Cause NE release only – Example: • Amphetamine – CNS stimulant – Increases BP by alpha effect on vasculature, beta effect on heart Mixed-Action • Causes NE release AND stimulates receptor • Example: – Ephedrine: • • • • What type of drug? Alpha and beta stimulant Use: asthma, nasal sprays slower action Adrenergic Antagonists • Alpha blockers – Eg: Prazosin • Selective alpha 1 blocker • Tmt: hypertension – relaxes arterial and venous smooth muscle – Causes “first dose” response (what is this?) Adrenergic Antagonists • Beta Blockers • Example: Propranolol – Non-selective (blocks beta 1 and beta 2) – Effects: • ↓ cardiac output, vasodilation, bronchoconstriction Adrenergic Antagonists • Eg: Atenolol, Metoprolol – Preferentially block beta 1; no beta effects (why is this good?) • Partial Agonists: – Pindolol, acebutolol • Weakly stimulate beta 1 and beta 2 • Causes less bradycardia Adrenergic Antagonists • Eg: Nadolol – Nonselective beta blocker – Used for glaucoma • Eg: Labetolol – Alpha AND beta blocker – Used in treating PIH Drugs that Affect Uptake/Release • Eg: Cocaine – Blocks Na+/K+ ATPase – Prevents reuptake of epinephrine/norepinephrine Treatment of Movement Disorders What Regulates Movement? Basal Ganglia are involved Example: Parkinsons’s Disease • Symptoms ? FRONTAL SECTION OF BRAIN Sherwood, 2001 p 145 BASAL GANGLIA cont’d • Role of basal ganglia: 1. Inhibit muscle tone throughout the body 2. Select & maintain purposeful motor activity while suppressing useless/unwanted patterns of movement 3. Coordination of slow, sustained movements (especially those related to posture & support) 4. Help regulate activity of the cerebral cortex BASAL GANGLIA SYSTEM Feedback loops - complex - form direct & indirect pathways - balance excitatory & inhibitory activities Neurotransimitters: Excitatory - ACh glutamate Inhibitory - dopamine GABA DOPAMINE • major NT regulating subconscious movements of skeletal muscles • majority located in the terminals of pathway stretching from the neuronal cell bodies in SNc to the striatum • generally inhibits the function of striatal neurons & striatal outputs • when dopamine production is , a chemical imbalance occurs affecting movement, balance and gait PATHOPHYSIOLOGY OF PARKINSON’S DISEASE • Major pathological features: 1. Death of dopamine producing cells in the SNc leads to overactivation of the indirect pathway 2. Presence of Lewy bodies –small eosinophilic inclusions found in the neurons of SNc Results in:- degeneration of the nigrostriatal pathway - decreased thalamic excitation of the motor cortex 4. Drug of Choice: LEVODOPA Why is it used? - virtually all pt’s with PD show a response to levodopa - improves quality of life - in use since 1960’s - easy to administer (non-invasive) - relatively inexpensive - useful in diagnosing PD • Mechanism of action: is a precursor to dopamine helps restore the balance of dopamine in striatum –most effective in combo with Carbidopa ( ’s levodopa’s peripheral conversion to dopamine) 5. OTHER APPROACHES TO TREATMENT • Pharmacological: – Dopamine agonists: ie. Bromocriptine or pergolide mesylate – Selective inhibitor of type B monoamine oxidase: ie.Selegiline – Antivirals: ie. Amantadine – Anticholinergics: ie. Trihexyphenidyl – COMT inhibitors: ie. Entacapone APPROACHES cont’d • Surgical: • Pallidotomy & Thalotomy: – microelectrode destruction of specific site in the basal ganglia • Deep brain stimulation: – electrode implantation with external pacemaker • Fetal nigral transplantation: – Implantation of embryonic dopaminergic neurons into the substantia nigra for growth and supply of dopamine