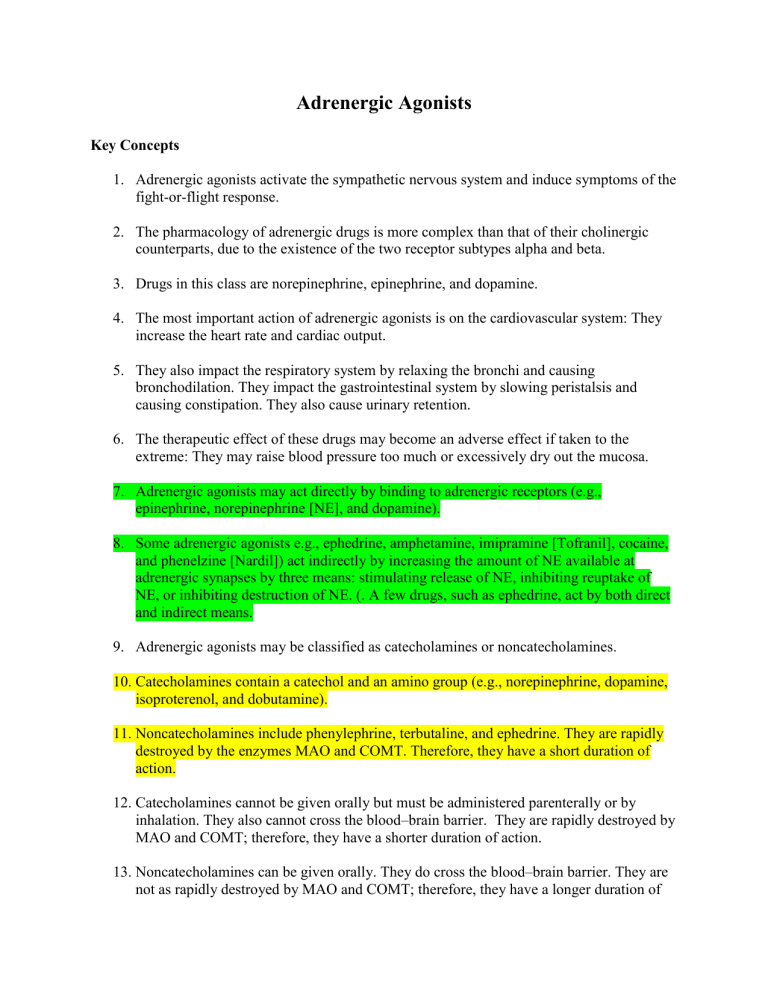
Adrenergic Agonists Key Concepts 1. Adrenergic agonists activate the sympathetic nervous system and induce symptoms of the fight-or-flight response. 2. The pharmacology of adrenergic drugs is more complex than that of their cholinergic counterparts, due to the existence of the two receptor subtypes alpha and beta. 3. Drugs in this class are norepinephrine, epinephrine, and dopamine. 4. The most important action of adrenergic agonists is on the cardiovascular system: They increase the heart rate and cardiac output. 5. They also impact the respiratory system by relaxing the bronchi and causing bronchodilation. They impact the gastrointestinal system by slowing peristalsis and causing constipation. They also cause urinary retention. 6. The therapeutic effect of these drugs may become an adverse effect if taken to the extreme: They may raise blood pressure too much or excessively dry out the mucosa. 7. Adrenergic agonists may act directly by binding to adrenergic receptors (e.g., epinephrine, norepinephrine [NE], and dopamine). 8. Some adrenergic agonists e.g., ephedrine, amphetamine, imipramine [Tofranil], cocaine, and phenelzine [Nardil]) act indirectly by increasing the amount of NE available at adrenergic synapses by three means: stimulating release of NE, inhibiting reuptake of NE, or inhibiting destruction of NE. (. A few drugs, such as ephedrine, act by both direct and indirect means. 9. Adrenergic agonists may be classified as catecholamines or noncatecholamines. 10. Catecholamines contain a catechol and an amino group (e.g., norepinephrine, dopamine, isoproterenol, and dobutamine). 11. Noncatecholamines include phenylephrine, terbutaline, and ephedrine. They are rapidly destroyed by the enzymes MAO and COMT. Therefore, they have a short duration of action. 12. Catecholamines cannot be given orally but must be administered parenterally or by inhalation. They also cannot cross the blood–brain barrier. They are rapidly destroyed by MAO and COMT; therefore, they have a shorter duration of action. 13. Noncatecholamines can be given orally. They do cross the blood–brain barrier. They are not as rapidly destroyed by MAO and COMT; therefore, they have a longer duration of action. 14. The nonselective adrenergic agonists activate both alpha and beta receptors. The specific effects of each drug are dependent on which receptor subtypes are stimulated. 15. The first subtype is the alpha1-receptor agonists. They are used for the treatment of nasal congestion and hypotension. They may also be used to produce mydriasis during ophthalmic examinations. 16. The second subtype is the alpha2-receptor agonists. They are used for the treatment of hypertension. 17. The third subtype is the beta1-receptor agonists. They are used for the treatment of cardiac arrest, heart failure, and shock. 18. The fourth subtype is the beta2-receptor agonists. They are used for the treatment of asthma and to reduce preterm labor. 19. Some sympathomimetics are nonselective, stimulating two or more adrenergic-receptor subtypes (e.g., epinephrine and ephedrine). The nonselective adrenergic agonists generally cause more autonomic-related side effects than the selective agents. 20. One of the most important applications of the nonselective adrenergic agonists is for the pharmacotherapy of shock and other life-threatening cardiac disorders. 21. Epinephrine, norepinephrine, and dopamine are nonselective agents for shock and anaphylaxis when blood pressure and heart rate need to be quickly restored to normal levels. 22. Epinephrine is the prototype drug for nonselective adrenergic agonists. It is used to treat shock and anaphylaxis and as a bronchodilator. 23. The most common adverse effects of epinephrine are nervousness, tremors, palpitations, tachycardia, dizziness, headache, and stinging at the site of application. Serious adverse effects include HTN, dysrhythmias, pulmonary edema, and cardiac arrest. 24. Drugs similar to epinephrine include dopamine, droxidopa, ephedrine, and NE. 25. Activation of alpha-adrenergic receptors causes a number of important physiologic responses, most of which relate to contraction of vascular smooth muscle. 26. Alpha-adrenergic agonists are used for treatment of hypotension associated with shock and for treatment of orthostatic hypotension. 27. Another major action of alpha-adrenergic agonists is vasoconstriction of vessels in the nasal mucosa. These agents are used for upper respiratory tract infection or allergic rhinitis. An intranasal agent is phenylephrine. An oral agent is phenylephedrine. 28. A third action of alpha1-adrenergic agonists is vasoconstriction of arterioles in the eye and mydriasis. These agents are topically instilled into the eye and relieve conjunctival congestion and redness. They are also used for ophthalmic examination but are not the drug of choice for this purpose. 29. Activation of alpha2 receptors produces important responses in the brain rather than the peripheral nervous system. 30. The prototype alpha-adrenergic agonist is phenylephrine (Neo-Synephrine). Side effects are few and minor in character. 31. Drugs similar to phenylephrine are classified as intranasal decongestants or ocular decongestants. 32. Activation of beta1 receptors results in cardiac actions typical of the fight-or-flight response: Heart rate, force of contraction, and velocity of impulse conduction through the myocardium all increase. 33. Drugs with significant beta1 activity may be called cardiotonic or inotropic drugs. 34. Beta2-adrenergic receptors are more widely distributed than beta1 receptors. Pharmacologically, the most important site is in the lung. 35. Activation of beta2 receptors leads to relaxation of bronchial smooth muscle. Beta2adrenergic agonists are commonly referred to as bronchodilators and are used for treatment of bronchial asthma and other pulmonary disorders. 36. Beta2-adrenergic agonists are also used for the treatment of preterm labor contractions. These drugs are called tocolytics. 37. Isoproterenol (Isuprel) is the prototype nonselective beta-adrenergic agonist and is used as a bronchodilator and as a cardiac stimulator. 38. Common adverse effects of isoproterenol include headache, nausea, vomiting, and symptoms of CNS stimulation such as tremors, anxiety, and insomnia. Adverse effects on the heart include serious dysrhythmias. 39. Drugs similar to isoproterenol (Isuprel) are grouped into two primary subclasses: bronchodilators and tocolytics. Tocolytics are used for the treatment of preterm labor contractions. 40. Adrenergic agonist therapy requires continued frequent and careful monitoring of vital signs and urinary and cardiac output as appropriate, especially if IV administration is used. 41. Instruct the patient to report palpitations, shortness of breath, chest pain, excessive nervousness or tremors, headache, or urinary retention immediately. 42. Caffeine intake should be limited or eliminated to reduce nervousness, insomnia, and tremors. 43. IV adrenergic drips may cause intense vasoconstriction if extravasated. 44. Patients who have diabetes may experience increased blood glucose. 45. Photosensitivity may occur. 46. Nasal sprays should not be used longer than 3 to 5 days without consulting the prescriber.