Urinary System
advertisement

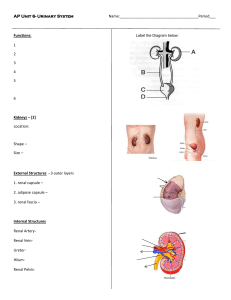
Urinary System Our Goals This Section.... • Identify and explain the functions of each of the following: – – – – – – – – kidney ureter urethra urinary bladder renal cortex renal medulla renal pelvis nephron – – – – – – – glomerulus Bowman’s capsule afferent and efferent arterioles peritubular capillary network proximal and distal convoluted tubules collecting duct loop of Henle • Identify and explain the functions of the following components of the nephron: Wastes Excretion Main wastes: carbon dioxide and ammonia Ammonia comes from the digestion of amino acids Ammonia goes to liver and is converted to UREA Digestion of nucleic acids produce URIC ACID Must be secreted so they don’t become toxic Some wastes and water are excreted when you exhale • Water is also excreted in sweat • Kidneys are the primary organ of waste excretion – they take urea, uric acid, excess H+, water soluble vitamins, etc from the blood and excrete as urine • • • • • • • Urinary System Kidneys • Renal arteries deliver blood to kidneys to “clean it” • Blood leaves the kidneys via the renal vein • Nephrons – – – – Functional unit of the kidney Remove wastes Make Urine Millions/kidney • Urine collects in the pelvic region of the kidney where peristalsis moves it to the ureters and then the urinary bladder Nephron Nephron • Tubules • All the same pattern • Start in the cortex of the kidneys with the Bowman’s capsule • Then loop down into the renal medulla • Bowman’s capsule →proximal convoluted tubule → loop of Henle → distal convoluted tubule → collecting duct Blood Flood • • • • • • • Renal Artery Afferent Arterioles Glomerulus Efferent Arterioles Peritubular Capillaries Venule Renal Vein Remember Our Goals Today.... • Identify and explain the functions of each of the following: – – – – – – – – kidney ureter urethra urinary bladder renal cortex renal medulla renal pelvis nephron – – – – – – – glomerulus Bowman’s capsule afferent and efferent arterioles peritubular capillary network proximal and distal convoluted tubules collecting duct loop of Henle • Identify and explain the functions of the following components of the nephron: Our Goals Today... • Describe the production of urine with reference to the following terms: – – – – – pressure filtration selective reabsorption reabsorption of water following an osmotic gradient tubular excretion metabolic waste (e.g., nitrogenous waste, urea, ammonia) • Describe how the kidneys maintain blood pH • Compare urea and glucose content of blood in the renal artery with that of the renal vein • Identify the source glands for antidiuretic hormone (ADH) and aldosterone • Describe how the hypothalamus, posterior pituitary, ADH, and the nephron achieve homeostasis of water levels in the blood • Describe how the adrenal cortex, aldosterone, and the nephron achieve homeostasis of water and sodium levels in the blood Urine Formation • Interaction between the tubules of nephrons and the blood capillaries • Modified version of blood capillary fluid exchange • There are 3 stages of urine formation 1. Pressure Filtration 2. Selective Reabsorption 3. Tubular Secretion Pressure Filtration • Blood slows down when it enters the cortex (enters the capillaries of the glomerulus) • Structure allows blood pressure to force small parts of the blood plasma into the spaces surrounding the glomerulus • Bowman’s capsules cup around each glomerulus • Substances removed from blood are forced into the beginning of the nephron tubules by constant blood pressure Pressure Filtration • Fluid entering tubules is called FILTRATE • Large components like blood cells and globulins are too big therefore stay in the blood • Creates an osmotic gradient between the blood and extracellular fluid Selective Reabsorption • Filtrate contains useful materials that the body needs (eg. Glucose, amino acids, nutrients, etc.) • Cells in the proximal convoluted tubule have CARRIER PROTEINS designed to pump these materials back into the peritubular capillaries • Requires ATP • Some Na+, Cl- and water are reabsorbed – Na+ is pumped out of filtrate – Cl- and water follow passively into the blood plasma Selective Reabsorption • As the filtrate moves through the nephron it makes 3 passes between the cortex and the medulla before entering the renal pelvis • Filtrate goes from the proximal convoluted tubule to the descending loop of Henle – Here the tubule is permeable to water but not Na+ – The extracellular region of this part of the tubule has a high solute concentration – therefore water moves out of the tubule and into blood (osmosis) • Filtrate is now very “salty” Selective Reabsorption • Permeability of the ascending loop of Henle is different – permeable to Na+ and not permeable to water • Na+ diffuses out of the tubule (concentration gradient) • When the filtrate gets closer to the cortex diffusion lessens so ATP is used to remove more Na+ from the filtrate • Once at the distal convoluted tubule in the cortex the filtrate is iso-osmotic to the extracellular fluids Tubular Secretion • Substances that are excess in the blood are pumped out of the peritubular capillaries around the distal convoluted tubule (enter filtrate) • Substances: penicillin, histamines, vitamins • In the distal tubule pH of the blood is also adjusted – absorption of H+ or HCO3- Final Phase of Urine Formation • Collecting duct moves the filtrate through the medulla one last time • Filtrate is subjected to the increasing concentration gradient of the extracellular fluids • Extracellular fluid in the medulla is hypertonic to the filtrate • Water is withdrawn as the filtrate as moves into the renal pelvis Final Phase of Urine Formation • ~99% of water in the filtrate is reabsorbed when urine is produced • Throughout the tubule urea is reabsorbed in very small amounts because of its low threshold level – However some urea will diffuse out of the collecting duct into the medulla (contributes to the high solute concentration around the loop of Henle) – It will re-enter the tubule along the ascending loop of Henle • Urine is what remains in the tubule Composition of Urine • Mainly water even though most of the water has been reabsorbed • Urea – low threshold in blood therefore stays in the nephron during urine formation Glucose • Blood has a high threshold level in the plasma so most of it is reabsorbed from the nephron • Requires ATP and transport proteins in the tubules • Liver removes excess glucose and stores it as glycogen • Diabetes is a malfunction in this system – higher glucose concentration in the blood causes glucose to be excreted in the urine (less water is reabsorbed) – Abnormal amounts of urine can be a symptom of diabetes • Diuretic versus Antidiuretic Regulation of Urine Formation • Antidiuretic Hormone (ADH) is secreted by the posterior pituitary gland when blood volume is low – ADH causes more water to be reabsorbed in the collecting duct – This increases blood volume (& blood pressure) • Alcohol is a diuretic because it inhibits ADH – Causes increased urine production – Excessive consumption leads to dehydration Aldosterone • If the blood pressure drops the regulation of urine is in danger • Aldosterone is released from the adrenal cortex • Increases the amount of Na+ absorption in the distal convoluted tubule • This in turn leads causes more water to be absorbed restoring the blood pressure Remember Our Goals Today... • Describe the production of urine with reference to the following terms: – – – – – pressure filtration selective reabsorption reabsorption of water following an osmotic gradient tubular excretion metabolic waste (e.g., nitrogenous waste, urea, ammonia) • Describe how the kidneys maintain blood pH • Compare urea and glucose content of blood in the renal artery with that of the renal vein • Identify the source glands for antidiuretic hormone (ADH) and aldosterone • Describe how the hypothalamus, posterior pituitary, ADH, and the nephron achieve homeostasis of water levels in the blood • Describe how the adrenal cortex, aldosterone, and the nephron achieve homeostasis of water and sodium levels in the blood